Course
Understanding the Different Types of Strokes
Course Highlights
- In this course we will learn about the non-ischemic causes of a stroke, and why it is important for nurses to recognize early symptoms for all types of strokes.
- You’ll also learn the causes of subarachnoid, intracerebral, and intracranial hemorrhages.
- You’ll leave this course with a better understanding of how to calculate cerebral perfusion pressure.
About
Contact Hours Awarded: 1.5
Course By:
Joanne Kuplicki
MA, RN, ccrn, Nc-bc
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Nurses are at the forefront of recognition and treatment of all types of strokes. It is imperative that we as nurses are aware that there are multiple causes and types of strokes, each of which has a varied treatment. The health care team must be mindful of newly recognized treatments for strokes related to the anatomical disorder causing it. Ischemic stroke is still the leading cause of a stroke, but we will expand our knowledge of other reasons for it during this course. The entire multidisciplinary team can make a difference in patient outcomes with swift assessment and treatment of the several types of strokes.
Epidemiology
17 million people (global population) suffer from one of the distinct types of strokes each year, resulting in being the 5th leading cause of death. In 2010, the World Stroke Organization (WSO) declared strokes a public health emergency. Strokes occur when the blood vessels that carry oxygen and nutrients to the brain are either blocked by clots or bursts (ruptures), causing reduced blood flow and oxygen (1). Most types of strokes are 80% preventable, increasing the need for patient/family education and the aggressive treatment of risk factors. The American Stroke Association (ASA) and WSO provide both public and professional education links and materials for all. World stroke day occurs on October 29 each year to increase public awareness of all types of strokes and prevention.

Self Quiz
Ask yourself...
- Are you aware of your organization‘s Stroke Awareness activities?
- Do they include this public awareness education for women on their “GO RED“ day as well in February?
Stroke Causes
Nurses are often given rigorous training on the several types of stroke’s recognition and treatment(s). However, we often make assumptions that an ischemic stroke from a clot is the main culprit since it is the more prevalent cause. Ischemia occurs from a blockage or clot, and Transient Ischemic Attack (TIA) occurs when there is a temporary blockage or clot causing symptoms that are shorter in length and often fleeting. Some refer to TIA as a “mini-stroke.” TIA’s should be taken seriously because they can increase future risk of a stroke. A cryptogenic stroke is one in which a cause cannot be determined.
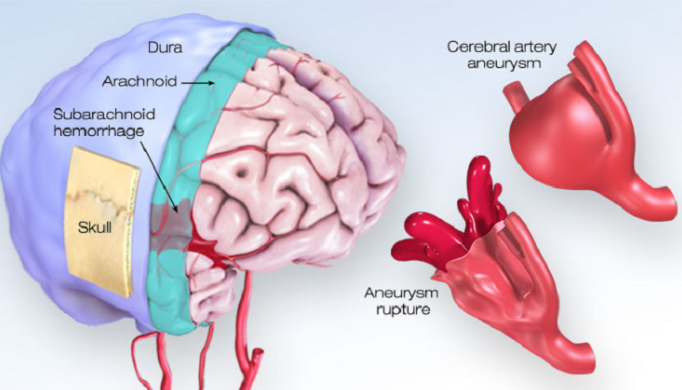
Intracranial hemorrhage refers to bleeding that occurs within the skull, and an Intracerebral hemorrhage refers bleeding within the brain parenchyma.

Self Quiz
Ask yourself...
- Have you had a patient or client in your practice that described symptoms of stroke and may have mistaken this due to other reasons? For example, “I slept on my arm,“ or “I get weak when I overdue activities since I am older,“ or “my speech was slow but passed quickly.“
Intracerebral Hemorrhage
The bleeding that occurs within the brain from an Intracerebral hemorrhage is due to either traumatic or non-traumatic events, which may include (4):
- Hypertension
- Eclampsia
- Drug abuse
- Excess blood flow from aneurysm rupture
- Reperfusion injury
- Cold exposure
Cerebral bleeding is often seen in “non-penetrating” falls in the elderly that are on anticoagulation therapy.

Self Quiz
Ask yourself...
- My first experience with cerebral bleed from a cerebral aneurysm was in a 30-year-old post-partum patient who bled during the later stages of labor, became obtunded, and was transferred post-delivery to the Surgical ICU. Naturally, all of the nurses were newly exposed to a case like this. What fears would this present to the staff, and how would you react to caring for someone so young with a significant neurological presentation?
Intracranial Hemorrhage
The skull is a closed space, and hence an increase in pressure from any of the contents, mainly the brain, blood, and cerebral spinal fluid (CSP), will cause an increase in intracranial pressure. Most signs and symptoms are related to this premise which was originated from the Monro-Kellie Doctrine. Unless there is a reduction of pressure of another content of the brain, any increase in the volume of CSP, blood, or edema will cause the patient to have signs of intracranial pressure or (ICP).
Cerebral Perfusion
The concept of cerebral perfusion is important for nursing clinicians to understand, due to their frequent performance of bedside assessments, including vital signs and ICPs. Cerebral perfusion is the pressure needed to maintain blood flow to the brain for survival (5). The normal range for cerebral perfusion pressure (CPP) is 60-80 mmHg, calculated by subtracting ICP, the downward pressure, from the mean arterial pressure (MAP), the upward pressure.
MAP is calculated either automatically or mathematically by vital sign monitors (see formula below). Remember that a tachycardic patient does have more systolic time, so the MAP will be slightly higher. Normal intracranial pressure (ICP) in adults is 5-15 mmHg. It can be regulated to some degree in the body by shifting cerebral spinal fluid into the spinal area rather than the brain and some cerebral regulation to create a steady flow of blood.
Formulas
CPP=MAP-ICP in mmHg
MAP= (Systolic BP x1) + (Diastolic BP x 2) in mmHg
Divided by 3

Self Quiz
Ask yourself...
- So let us calculate CPP in a normal healthy patient with BP of 120/80 mmHg and ICP 13. Using the MAP formula above to start: 120 (Systolic BP) + 160 (Diastolic x 2) = 280 divided by 3 = 93.3 MAP. Subtract ICP of 13, and the CPP is 80.3 (normal range 60-80).
- Now calculate the CPP for a patient with BP 180/100 (MAP 126.6) and ICP 26
- Are these within normal range?
- Can ICP and blood pressure be improved? How?
Intracranial Pressure
The symptoms of ICP include headache, blurred vision, vomiting, lack of energy, and change in mood or alertness. Increased ICP can be diagnosed within history/physical, spinal tap, CAT scan, or MRI.
A study looking at the effects of nursing interventions on intracranial pressure found some interesting results. It examined the “relationship between intracranial pressure and specific nursing interventions observed during routine care“ (6). The study recorded 3,118 direct observations at 1 minute and 5-minute time frames while monitoring intracranial pressure using a variety of methods in an intensive care unit setting. It found that drainage of cerebral spinal fluid did not have a significant effect. However, other studies have found there is some effect of cerebral spinal fluid drainage only in those with higher starting ICP pressures (greater than 25 mmHg).
Some nurses may assume that repositioning will increase ICP, but the study found that repositioning uncomfortable items like cervical collars and endotracheal tubes, as well as raising the head of the bed, talking, decreasing stimulation and sedative medications improve and reduce ICP (6). It is vital that the multidisciplinary team recognize normal levels of ICP at 5-15 mmHg with variations up to 20-30 mmHg defined as intracranial hypertension. It is essential that we prevent significantly elevated levels of ICP, which can lead to fatal cerebral herniation or shifting of the brain contents out of the skull.

Self Quiz
Ask yourself...
- Have you ever had a patient that had a change in neurological condition and/or ICP after a procedure or nursing intervention?
- Did the ICP status improve or change in a restful state?
Treatment of Cerebral Subarachnoid Hemorrhage
The initial treatment of a cerebral subarachnoid hemorrhage relates first to its diagnosis. Treatment for the various assessment symptoms are as follows:
- Respiratory: A primary assessment of ABCs, validating whether the patient can maintain and protect their airway is necessary. If they are unable, then mechanical ventilation is warranted. Blood pressure: Blood pressure goals are typically aimed at maintaining Systolic BP less than 160 mmHg.
- Temperature: A temperature greater than 101 is treated and imperative to brain integrity.
- Glucose: Glucose management is imperative for brain integrity.
The treatment related to an aneurysm is the placement of a clip at the neck of the outpouching or a coil placed inside the aneurysm, which creates intravascular clotting and prevents blood from getting into the aneurysm defect. Both procedures are performed in a specialized lab using catheters threaded through the groin up to the artery and into the brain. General treatments include treatment of electrolyte imbalance, especially hyponatremia, anemia from bleeding, and seizures. A ventricular drain may be placed if evidence of hydrocephalus (excess cerebral spinal fluid).
Several grading systems score the severity of the hemorrhage and clinical data. The incidence of re–bleed typically occurs 24 hours after onset“. (3) The fear of delayed neurological deterioration is real and can be from cerebral ischemia, edema, or vasospasms. Some centers will utilize transcranial Doppler monitoring post–event or nimodipine (Nimotop) 60 mg orally every 4 hours after 4 days for vasospasm after subarachnoid hemorrhage.
Free water (like hypotonic D5W) is avoided since it increases cerebral edema, and some hypertonic solutions (higher saline and dextrose percentages) may be given cautiously.

Self Quiz
Ask yourself...
- Have you ever had professional discussions and/or discord among the disciplines about what type of IV fluids should be prescribed for a particular patient?
- How was that resolved as a patient advocate?
Conclusion
Nurses are at the forefront in recognition, monitoring, and intervention of the several types of strokes. We are especially vital since the time at the bedside enables us to assess subtle changes in vital signs, behavior, or ICP signs and symptoms and report these findings timely for intervention. Patient and family communication is essential because conditions can change rapidly, and this injury to the brain can be severe. Neurological care can be challenging but rewarding at the same time.
References + Disclaimer
- American Stroke Association. (2021, February 11) “About Stroke“. https://www.stroke.org/en/about-stroke
- World Stroke Organization. (2021, March 01) “World Stroke Campaign-2010 Declared Stroke a Public Health Emergency“. https://www.world-stroke.org/
- Boling, B. & Groves, T.R. (2019) “Management of Subarachnoid Hemorrhage“. Critical Care Nurse, 39 (5), 58-67. https://doi.org/10.4037/ccn2019882
- Liebeskind, David S. (2018, December 07) “Intracranial Hemorrhage-Overview“. Medscape Update accessed March 01, 2021. https://emedicine.medscape.com/article/1163977-oerview?src=mbl_android&ref=share
- Mount, C.A. &Das, J. (2020, May 26) “Cerebral Perfusion Pressure“ Stat Pearls. https://www.ncbi.nlm.gov/books/NBK537271/#_NBK537271_pubdeet_
- Olson, D.M. et al. (2013) “Effects of Nursing Interventions on Intracranial Pressure“. American Journal of Critical Care, 22 (5), 431-438. https://doi.org/10.4037/ajcc2013751
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate

