Course
The Role of a Nurse in the Correctional Setting
Course Highlights
- In this course we will learn about the role of a nurse in the correctional setting and the unique patient population.
- You’ll also learn about the health disparities of incarcerated populations.
- You’ll leave this course with a broader understanding of the evolution of correctional healthcare.
About
Contact Hours Awarded: 2
Course By:
Sheila Burns
MSc, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Nurses are often unaware of the opportunities and realities of working in the correctional setting, as few nursing schools can find placements for students during their training. This course is intended for nurses who are interested in correctional nursing to understand what their role may be and the importance of it. This course will also be beneficial for current correctional nurses to review different ideas and perspectives that may help to improve their provision of care.
Introduction
Correctional Nursing is a specialty in the nursing world that gets little attention and is usually poorly funded. However, it is a specialty that is key to our community‘s health and public health as well. Over 77% of incarcerated people are released back into the community. Thus, we are actually looking after our own community most of the time.
Nurses are often unaware of the importance of the opportunities and realities of working in this setting, as few nursing schools are able to find placements for students to be exposed to it during their training. This article is intended to allow nurses who may be interested in correctional nursing to determine what the role may involve and allow for current correctional nurses to review different ideas and perspectives that can allow them to improve their provision of care.
Evolution of Correctional Health Care
Nursing, as a profession, is ever evolving and changing. Nurses are constantly pioneering and working within a research-driven environment. The profession is supported by a multidisciplinary team of medical and nursing personnel who can collaborate effectively and who are all focused on the same goal.
However, Correctional nursing is a smaller specialty, which involves a smaller team environment with limited access to resources such as training, research, staffing, etc. Correctional nurses are also faced with a different financial outlook than other privately or publicly funded specialties and institutions. Correctional healthcare is reliant upon national or local funding determined by the government. As a result, extra-curricular services, such as research, are not prioritized in this environment.
Correctional nurses have frequently been seen as inferior to other nursing professional groups and get pulled into ‘caring for the order of the prison rather than ordering care for the prisoners’ (2). Without research into the role of the nurse in corrections, there should be no surprise that the definition in the literature is unclear (1).
The literature that does exist on the nursing profession in correctional settings is largely based in other parts of the world. The World Health Organization (WHO) has been active in prison health care since the Ottawa Charter for Health Promotion in 1986 (3). This charter provided the impetus which led to the Health Promoting Prison (HPP) movement in which 25 European and former Eastern Bloc countries participated (to varying degrees). Within this movement, progress was made with documents/reports related to mental health promotion topics, prison health as a part of public health, HIV in Prisons, Drugs, and Society, and promoting young people’s health.
***Note: Jails and Prisons are interchangeable terms when discussing correctional settings abroad. Some countries house all prisoners in the same building and call it a “jail” or “prison” – this does not distinguish their legal standing).
Unfortunately, there is no similar information regarding the US using this method to progress correctional care (1). The WHO promotes an organizational commitment to correctional health care – to include policy and lawmakers at the Government level, right down to the facilities’ security and health team.
The US has the National Commission on Correctional Health Care (NCCHC), established in 1983. Their mission is “to improve the quality of health care in jails, prisons, and juvenile confinement facilities. NCCHC establishes standards for health services in correctional facilities, operates a voluntary accreditation program for institutions that meet those standards, produces resource publications, conducts educational conferences and offers certification for correctional health professionals” (4). The NCCHC can certainly be viewed as the gold standard. Still, there is no government policy to ensure that all facilities are abiding by these standards– being accredited by NCCHC is optional.

Self Quiz
Ask yourself...
- In your facility, do you perform any research?
- What kind of research do you think would benefit correctional nursing?
- Have you been part of any improvements – small or large – in your facility?
Who are our Patients?
To identify the role a nurse can play, we first need to identify our patients. It can become overwhelming at times with the comings and goings in a correctional setting. Unlike a hospital setting or a long-term care facility, correctional nurses are often caring for hundreds of patients at one time. Therefore, identifying the patients who require time and care in an efficient manner is an essential part of nursing within this field.
Our patient population is directly affected by what is happening in other spheres. It is important to understand where we stand today with regards to the pressures on a jail. Looking at crime and imprisonment rates in the graph below shows a dramatic increase in the 1990s despite a reduction in homicide rates, motor vehicle thefts, and burglary (5). So, what happened?
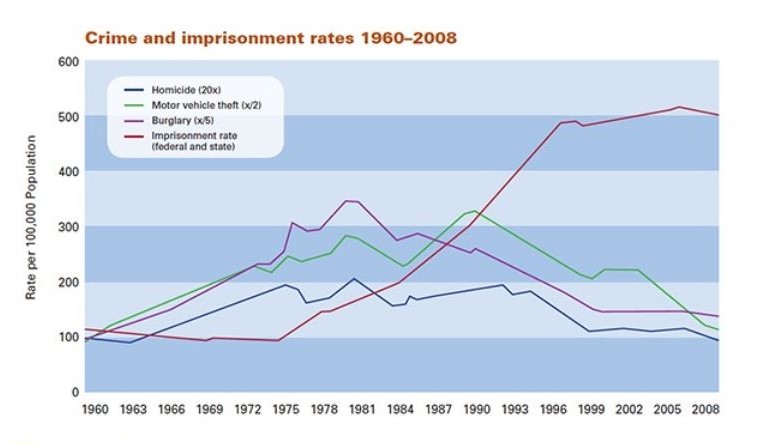
In the 1960s, when the major mental health institutions that housed the mentally ill closed and the community resources were not prepared nor equipped to deal with this need. One study showed that this accounted for around 7% of the increase in jails and prisons from the 1980s to 2000 (7).
There were also some politically based decisions made to deal with the drug issue in the 1980s. This led to an increase in drug crime penalties, including minimum sentencing and the “three-strikes” law, leading to people needing to serve 85% of their sentence (7). Lawmakers have a direct impact on our patient population, from the massive increase in population shown in the graph to the more recent decrease in population due to the Covid-19 pandemic.

Self Quiz
Ask yourself...
- Have you noticed an increase or decrease in your patient population?
- Does this impact the type of work you can do?
Health Disparities of Incarcerated Populations
Today, 64% of patients being incarcerated in jails have mental health disorders (7), and 65% qualify as having substance abuse or addiction to drugs and/or alcohol (8). It is also widely reported that substance/alcohol abuse is interlinked with mental health issues.
40% of all incarcerated patients have a chronic medical condition (9). For specific disease groups, the prevalence inside facilities is higher than the general US population, please see the chart below (9).
| Disease | % US Population | % Incarcerated Population* |
| Diabetes | 6.5% | 9.8% |
| Hypertension | 25.6% | 29.4% |
| Asthma | 7.5% | 8.7% |
| HIV | 0.5% | 1.4% |
*This percentage of incarcerated population includes both federal and state facilities.
Demographics are also key factors to consider. 9.8% of incarcerated people are females (10). Females clearly have different medical and nursing needs than men do, and healthcare must be flexible enough to manage this, especially with pregnancy and childbirth issues.
The racial disparities are also a reflection of community and governance issues outside the jail walls. 40% of the inmate population is African American, despite being only 13% of the US population. The Hispanics are also disproportionately detained – 20% of the inmate population but only makeup 17% of the US population (7). Health issues that are more prevalent in the African American population, for example, such as hypertension or sickle cell disease, reflect the need for a robust health system.

Self Quiz
Ask yourself...
- Think of your facility – what is the racial mix?
- Does this bring different challenges to how you can deliver care?
- Do you look after females?
- If so, what extra care plans are in place to ensure they are appropriately cared for?
Nurses’ Role
If you are reading this to find out what happens inside a correctional facility, then this section might be for you! Correctional nursing is a constant challenge to your own personal growth and being able to hone in on your clinical assessment skills.
The environment in which correctional nurses work is not conducive to good health. In fact, it is quite the opposite. For a human being to be kept in a small space with limited access to socializing, a poor diet, minimal exercise, and no personal growth are nowhere near a healthy existence. Not only are the patients’ conditions poor, but the system we must work within is focused on security, and thus delivering care is met with challenges.
This is when nurses can excel by being innovative and determined to deliver the care that our population really needs. When faced with a difficult case, thinking of your community is a great coping tool. This difficult patient will more than likely be released and getting his or her health care to a gold standard will positively impact not only their life but your community’s health too. This is the adage that Prison/Jail Health is part of Public Health comes to the fore.
A correctional nurse‘s role is varied from facility to facility; however, there are consistencies in job responsibilities in any correctional setting.
Intake and Screening
All patients should be screened on arrival to the facility to “ensure that emergent and urgent health needs are met” (11). Once the patient’s potential immediate needs are identified and managed – such as injuries, intoxication, psychosis, the potential for being contagious, the nurse must spend some concentrated time with the patient for further investigation.
Obtaining a comprehensive medical and psychiatric history sets the care pathway for the patient on a strong trajectory. The receiving screening is often referred to as a pivotal point when we can get information on patients’ needs, and if we miss this opportunity, patients can miss out on vital intervention later in their incarceration. For example, during morbidity or mortality reviews, the receiving screening is the first document that is examined. This allows the team to look for improvements in how questions are worded or if a question was not included, which may have prevented the negative outcome.
Being in the moment with the patient is an important aspect of the assessment. Often our patients are not happy to be where they are, belligerent, intoxicated, and sometimes aggressive. Being able to empathize with the patient is important.
It is often particularly challenging to have empathy for someone you know may have done something heinous. However, it is our job to find out their medical and psychiatric needs. The assessment still needs to be made care must be provided, ensuring that their pathway is the same as everyone else’s.
A patient’s security is also part of our assessment outcomes. Placing an 18-year-old male with educational difficulties in for his first arrest as ready for the general population is not protecting our patients. We must alert security staff to our findings and work with them to ensure the vulnerable patients are protected.
Follow-up care is also a critical process that the intake nurse must activate. Chronic Care services, Mental Health Services, Dental Services, Chaplain Services, Medication Verification, Medical Records from an outside Provider, etc. are all examples of follow–up care that the intake nurse can put into place.

Self Quiz
Ask yourself...
- Do you feel empathetic to someone who has been arrested for a heinous crime?
- Does knowing what the patient has been accused of change the way you may treat them?
Case Study:
Cindy is a 23-year-old female. It is her first time in jail, and she presents extremely intoxicated. Cindy states she has had six shots of vodka and has verbally admitted to consuming cocaine. She also states that she takes benzodiazepines for anxiety. She admits to currently seeing a psychiatrist for her suicide attempt three months ago. During your assessment, you find she is pregnant, and she has no idea when her last period was.
Who does Cindy need to see?
How urgent do you think Cindy’s needs are?
What personal security concerns do you have for Cindy?
Our actions, or inactions, with Cindy can have a long-lasting effect on not just Cindy’s health but on her unborn baby.
What could happen to Cindy if we did nothing?
It is vital for the nurse to be able to recognize all the services that Cindy may needs. This may involve an urgent referral to OB/GYN or potentially ER, depending on the site’s relationship with the local specialties.
A referral to the Mental Health team would be appropriate for her history and to support her regarding her pregnancy. A medication verification form and medical records request form may also need to be sent to the Pharmacy/Doctor’s Office to support the Mental Health team in their care pathway.
If the Chaplain deals with diet preferences, it may be an option to help her with that process too.
Security will also need to be made aware of Cindy’s vulnerability and her pregnancy status to allow them to house her in a protected area.
Working in intake and completing receiving screenings can be an incredibly challenging job. There are often time pressures put upon the nurse to get patients processed quickly. Using communication skills to the highest level – from watching, actively listening, honing in on specific information, focusing your attention on clinical assessments, and being in the moment with your patient helps not only get the task completed but also gathers quality information for the patient to be on the correct care pathway.
Medication Administration
Medication administration is a large part of nurses’ role in the correctional setting, as it is in most settings.
The Pharmaceutical service set-up can vary significantly from facility to facility. In some facilities, correctional officers administer medications, some have Medication Technicians, and some rely purely on the nursing staff.
Either way, patients have the right to receive their treatment in a timely manner (11).
Along with the actual medication administration, managing medication ordering is often a role fulfilled by nursing staff. Ensuring patients are not going to run out of their medications and ensuring new orders from Providers are fulfilled also often falls on ta nurse’s responsibility.

Self Quiz
Ask yourself...
- Think of your facility – how many obstacles get in the way for you to administer medications on time?
Non-Emergent Health Care Requests – Sick Calls
Incarcerated individuals have no choice about who provides their care, but they do have the right to access care. In some facilities, the patient has access to an internal system that allows them to complete a form to describe their health needs electronically. In other facilities, the patient completes a paper form which gets picked up by the nurses and managed appropriately.
The challenge for the nursing team is time management. Sick calls can be extremely time–consuming to complete, and in large facilities, the sick call list can be extensive. A face-to-face encounter must be conducted within 24hours of receiving the sick call, and an evaluation must be completed in a clinical setting (11).
Clinic Care
There is usually a medical center inside a facility – this can be from one small clinic room to numerous clinical spaces and even short-term accommodation for medical observations.
The nurses’ role in the clinic is one of managing the patient load, similar to an outpatient clinic in the community. Providers are often in the clinic rooms with patients referred from the sick call process for emergent/urgent issues and see patients who have chronic care issues. The nurses work alongside these Providers to take vital signs before the appointment, conduct other tests such as EKGs, lab draws, urine samples, etc., during or after the Provider appointment.
The clinic can also have outside health care professionals seeing patients. Physical Therapists, X-Ray Technicians, Dental Services, Telehealth sessions for a variety of specialists, for example, are supported by the nursing team.
Initial Health Assessments are also a nurse’s responsibility within the correctional setting. All patients are required to have this assessment completed before Day 14 of their stay in the facility (11). This assessment consists of reviewing the receiving screening information, asking more detailed questions regarding identified issues, as well as a physical examination of the patient. Any immediate needs are referred to the appropriate level of care.
Emergency Response
Emergency calls happen regularly, and it is the role of the nurses to respond without delay.
Emergency equipment- whether in carts or bags- should be available at a moment’s notice. This includes everything from Band-Aids to Glucose tablets to a defibrillator. The emergency bags should be checked every shift and restocked after every use. Nothing worse than speedily getting to a scene, and the emergency bag has “lost” its SpO2 monitor…
Educational aspects to this practice can be a whole couple of days’ worth of training for nurses. Our role here is more like an EMT, and we are often not trained or experienced in this kind of care before coming to work in a jail or prison. As a result, the nursing team must have a strategy for answering emergency calls –who has what role, etc. to maximize the chances of a positive outcome for the patient. Using critical thinking skills, completing a primary and secondary assessment on the patient, and deciding on the best level of care are key factors.

Self Quiz
Ask yourself...
- Does your facility have an emergency response plan for individual emergencies?
- Who takes responsibility for the emergency equipment?
- Does your facility have a plan for a mass disaster?
- Think of a time when you have had to respond to an emergency with a positive or negative outcome. What skills did you feel comfortable using, and what skills did you feel you lacked?
Conclusion
Correctional health services continue to evolve, improve, and respond to the needs of their patients. The nurse has a pivotal role in identifying gaps in care provision and work at a local level to improve patient outcomes.
There are many challenges to being a correctional nurse – most coming from political and judicial structures and the fact that the environment that we work in is, fundamentally, not healthy. Also, the patients we serve are often the most vulnerable in society and have complex medical and mental health issues.
The role of the nurse involves wearing many hats (not all roles are described above) – from handing out eyeglasses to responding to a mass disaster. Maintaining standards of care and using NCCHC (11) as a platform will enable nurses to stay focused on optimum patient care.
References + Disclaimer
- Whitehead, D. (2006). The health–promoting prison (HPP) and its imperative for nursing. International Journal of Nursing Studies, 43(1), 123-131. https://www.researchgate.net/profile/Dean-Whitehead/publication/7443428_The_Health_Promoting_Prison_HPP_and_its_imperative_for_nursing/links/5c70ddf9a6fdcc47159430aa/The-Health-Promoting-Prison-HPP-and-its-imperative-for-nursing.pdf
- Sim, J., 2002. The future of prison health care: a critical analysis. Critical Social Policy 22 (2), 300–323.
- World Health Organization (WHO), 1986. The Ottawa Charter for Health Promotion. WHO, Copenhagen
- https://www.ncchc.org/about.
- “The Growth of Incarceration in the United States: Exploring Causes and Consequences,” The National Research Council, 2014
- Almost, J., Gifford, W.A., Doran, D., et al. Correctional nursing: a study protocol to develop an educational intervention to optimize nursing practice in a unique context. Implementation Sci 8, 71 (2013). https://doi.org/10.1186/1748-5908-8-71
- Collier, L. (2014, October). Incarceration nation. Monitor on Psychology, 45(9). http://www.apa.org/monitor/2014/10/incarceration
- https://www.thenationshealth.org/content/40/3/E11
- Andrew P. Wilper, Steffie Woolhandler, J. Wesley Boyd, Karen E. Lasser, Danny McCormick, David H. Bor, and David U. Himmelstein, 2009: The Health and Health Care of US Prisoners: Results of a Nationwide Survey American Journal of Public Health 99, 666_672, https://doi.org/10.2105/AJPH.2008.144279
- https://www.prisonstudies.org/country/united-states-america.
- NCCHC “Standards for Health Services in Jails” 2018
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate

