Course
Endovascular Thrombectomy and Its Role in Ischemic Stroke Treatment
Course Highlights
- In this course we will learn about endovascular thrombectomies (EVT), and why nurses play an essential role in patient evaluation both pre- and post- procedure.
- You’ll also learn the basics of IV altephase (TPA).
- You’ll leave this course with a broader understanding of the key processes, risks, and success rate of EVT.
About
Contact Hours Awarded: 1.5
Course By:
Joanne Kuplicki
MA, RN, ccrn, Nc-bc
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
As healthcare professionals, it is our responsibility to be up to date on of all the new medical advancements and treatment options available to our patients; this is no different for stroke care and in this case specifically, ischemic stroke treatment.
Patients who suffer a stroke due to clotting or blockages typically will have general medical options. For example, medication treatments with IV alteplase (TPA), as well as interventional procedures that include clot removal/retrieval known as Endovascular Thrombectomy (EVT). Are we as caregivers familiar with these newer ischemic stroke treatment procedures beyond the IV infusions of “clot-busters?” These interventional treatments can be done up to 24 hours post-ischemic stroke.
Nurses are vital in the education of patients and families regarding signs and symptoms of stroke and the options that are offered, as well as knowing contraindications, essential monitoring, and complications.
Stroke Guidelines and Incidence:
The American Stroke Association (ASA) released updates in 2019 to the “2018 Guidelines for Early Management of Patients with Acute Ischemic Stroke” to reflect new clinical studies.
The guideline, which is available on the ASA website, enables clinicians to be aware of the best ischemic stroke treatment for improved patient outcomes (1). There are many acute care centers nationwide that are certified by the Joint Commission in Stroke Care that must follow these guidelines.

Self Quiz
Ask yourself...
Do neighbors and relatives ever ask you for referrals to the “best hospital” for stroke?
Do you know where the nearest certified stroke center is in your area since time is of the essence?
Ischemic Stroke Treatment: IV TPA and/or EVT
IV TPA:
An IV TPA is given once a hemorrhagic stroke has been ruled out by a CT scan of the head. This infusion is given within 4.5 hours of stroke onset and is standard for most ischemic stroke patients, even if EVT is being considered as an option.
- The nursing staff should have access to the complete list of contraindications to this medication which include (1):
- Acute intracranial hemorrhage
- Recent head trauma
- Intracranial or spine surgery in the past three months
- Recent GI bleed or malignancy
- The time frame should be as short as possible and is driven by the last time the patient was experienced as normal.
- IV TPA is given at a rate of 0.9 mg/kg IV, not to exceed a 90 mg total dose. It is preceded by giving a bolus dose of 10% of the total dose over 1 minute and the remainder of the infusion is given over 60 minutes (2).
- Post– infusion, the patient is admitted to the intensive care unit (ICU) for 24-hour monitoring. The ASA guideline recommends that vital signs, including a neurological assessment. The neuro assessment must be done every 15 minutes during and after TPA for 24 hours. This is followed by vital signs and neurological assessment every 30 minutes for 6 hours, and every 1 hour for 24 hours (2).
- Invasive lines (like central and arterial) and urethral catheter insertion should be delayed during immediate and post– TPA administration due to the increased risk of site bleeding (2).

Self Quiz
Ask yourself...
Does your facility have the ability to give IV alteplase (TPA) timely?
Are there trained practitioners, nurses and pharmacists available 24/7 to prepare and administer this IV infusion since it is time-sensitive?
EVT
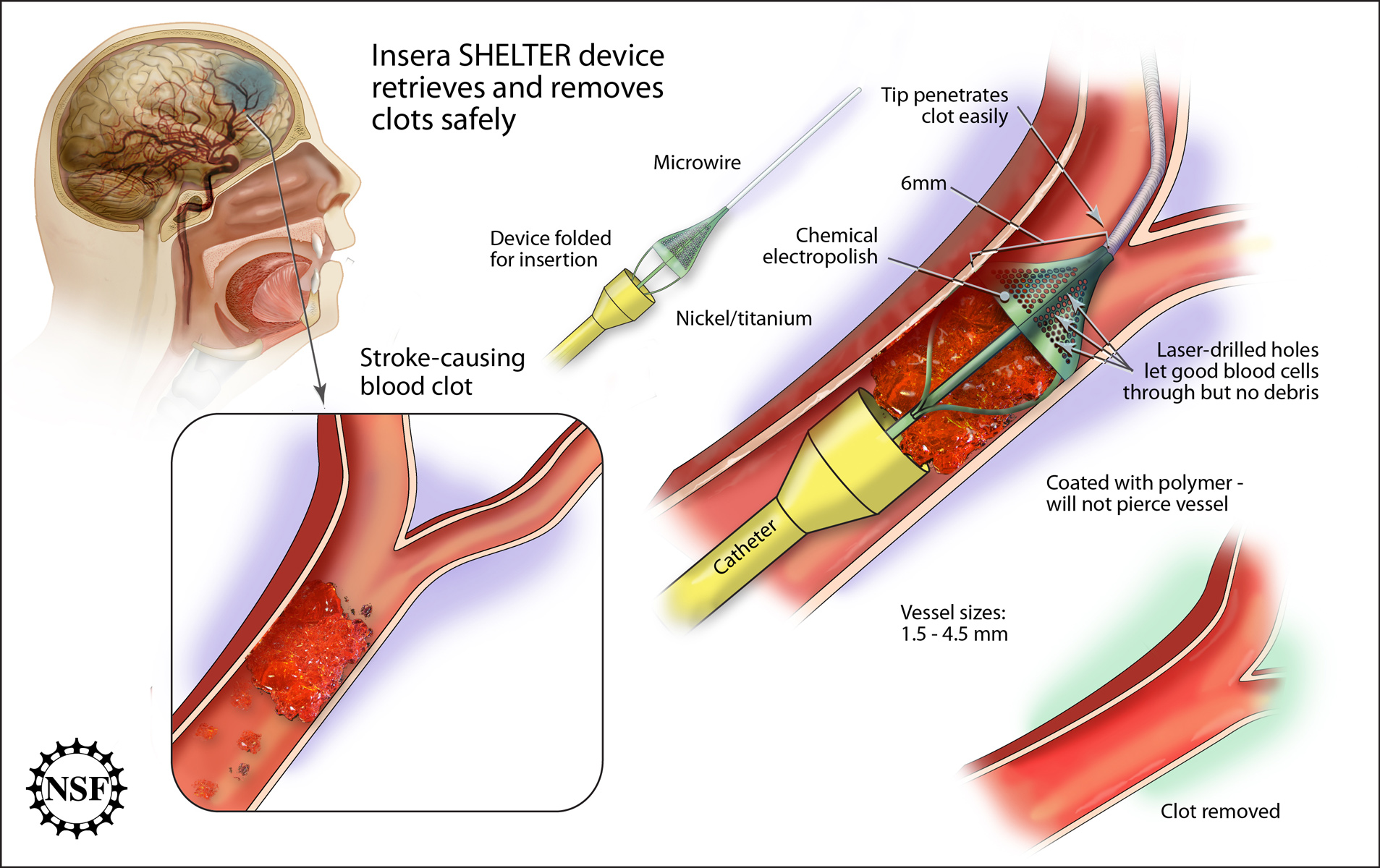
An EVT is the removal of a thrombus or blood clot under image guidance (4). It is one of the newer ischemic stroke treatment options available to patients.
EVT evaluation and treatment should be performed as soon as feasibly possible to patients who meet the criteria and are eligible. However, remember that not all acute care facilities have this capability, so urgent transport options may need to be considered as well.
- The time frame for EVT is recommended to be within 16 and up to 24 hours, in some patients with acute ischemic stroke (4).
- There are specific imaging criteria that must be met:
- The occlusion must be located within a larger, more proximal cerebral vessel, usually in the anterior circulation of the brain. (Remember that most of the anterior circulation is fed from the internal carotid artery, which ends in the anterior and middle cerebral artery. Blockage in these vessels can have devastating outcomes) (4).
- IV TPA and EVT interventions are time sensitive. Processes should be in place to avoid delay from “symptoms to definitive treatment” per ASA guidelines (1).
- As mentioned, the non-contrast CT scan is done as soon as possible to rule out hemorrhage prior to any treatment with IV clot-dissolving medications or neuro-vascular intervention.
- A finger-stick blood glucose is recommended prior to TPA IV administration, since glucose abnormalities can mimic stroke, as can other disorders such as drug overdoses, etc. A thorough history and physical examination is crucial, and the patient’s family and/or significant others can provide additional specific vital information.
- Vital signs (including oxygen saturation) are done along with neurological assessments.
- Lab work on stroke patients includes cardiac markers for ischemia (ex. troponin) and platelet count. IV TPA is contraindicated in those with platelet count less than 100,000 mm3. PT/INR and aPTT coagulation studies are part of the initial standard of treatment. Alteplase (TPA) is contraindicated with PT greater than 15 sec, INR greater than 1.7 and/or aPTT greater than 40 (1).

Self Quiz
Ask yourself...
- Does your facility have a timely lab turnaround time? Has there been any improvement in this process to include unit-based phlebotomists or nursing personnel trained to draw stat and time-sensitive lab specimens?
Key Processes:
- EVT can be done within 6-24 hours, and up to 24 hours after “last known well” time, not from the start of symptoms. Patients who present with symptoms after sleeping can have difficulty in establishing this timeframe.
- The patient’s Modified Rankin Score (MRS) pre-stroke should be 0-1 (out of 6), meaning a low level of existing disability prior to acute stroke.
- The CT scan with perfusion or MRI/MRA which shows brain circulation must reveal occlusion of the internal carotid artery or proximal (larger vessel width) middle cerebral artery.
- EVT is not an acceptable procedure for those under 18 OR for patients with an NIHSS score ≤of 6. (1)

Self Quiz
Ask yourself...
- Have you had experience either observing or performing the National institute of Health Stroke Scale (NIHSS) assessment on any potential or confirmed stroke patients?
- Do you know where to find resources quickly (for example www.stroke.nih.gov) for this vital assessment at your organization?
Potential Complications:
EVTs are now the most recommended ischemic stroke treatment option for patients. The entire team must be aware of potential intra-procedural and post-procedure complications. Complications should be minimized and effectively treated quickly.
Unfortunately, there is still approximately a “15% rate of complications with sequelae,“ and these include (3):
- Groin access site complications or infection
- Arterial vessel or nerve injury
- Hematoma
- Vasospasm
- Arterial perforation or dissection
- Device misplacement
- Rarely symptomatic intracerebral hemorrhage or subarachnoid hemorrhage occurs
- Embolic formation in the target vessel, or other areas that are listed as a potential complication
The nursing and neuro team members are key players in monitoring subtle neurological changes, although anesthesia during the procedure can delay post-procedure accuracy. The clinical staff should have unit-based training and education on assessing groin vascular puncture sites, care, and quickly controlling bleeding, assessing labs, and reporting findings in a timely manner. My organization added toe pulse oximetry as an additional tool to assess lower limb perfusion.

Self Quiz
Ask yourself...
Have you ever been responsible for monitoring patients post intra-vascular procedure?
Is there specific equipment or response team available for urgent intervention of complications (like Hemorrhage)?
Are they available 24/7 in your organization?
Nursing Role Post- Ischemic Stroke Treatment: IV TPA and/or EVT
For patients who have undergone an ischemic stroke treatment such as IV TPA and/or EVT, it is essential for nurses to frequently check vital signs and perform neurological evaluations, as this can work to ensure positive patient outcomes. Although this task predominately falls under the nursing role, all team members should be trained to recognize any change in signs/symptoms, including our interdisciplinary colleagues (supportive personnel, physical therapist, occupational therapist, and speech therapist, etc.). Here are a few details all nurses should be aware of post- IV TPA and/or EVT.
- If the patient’s blood pressure is greater than 180 systolic or 105 diastolic, they should be treated with an antihypertensive agent (1).
- Labetalol (Trandate) IV or nicardipine (Cardene) IV may be used for blood pressure management.
- Dysphagia evaluation early in the care of a stroke patient can determine the patient’s choking risk. This is a critical safety step to help prevent any aspiration event.
- Aspirin is part of the ASA’s ischemic stroke guidelines and is to be given at a dose of 325mg orally or rectally if the patient is NPO and within 48 hours of stroke/transient ischemic attack (TIA) onset.
- No aspirin is given within 90 minutes up to 24 hours post– IV TPA.

Self Quiz
Ask yourself...
- If you work in an area that takes care of stroke patients, have you had formal training on how to perform a standardized dysphagia evaluation?
- Is this documentation part of your electronic medical record to improve the continuum of care and transfer between units?
Experience of Regional Stroke Service: Ischemic Stroke Treatment
In 2015, a recognized Stoke Center evaluated 93 cases of EVT procedures. At the time of the study, this organization had an 86% success rate in obtaining cerebral reperfusion of ischemic stroke. The retrospective examination of these cases revealed a 14% failed vessel recanalization, meaning lack of restoration of blood flow in the cerebral artery to the brain. A positive functional outcome was measured by the MRS of equal to or less than 2 (low level of disability) in 55% of studied cases.
It is hopeful in 2021 that the functional outcome percentage is higher with more experienced stroke centers and a higher volume of procedures. Sadly, this review did reveal 90-day mortality of 22%. It is noted that most cases were received as transfers from outside centers. Again, this proves that timeliness of recognition of ischemic stroke and definitive treatment either within or outside the organization is crucial for improved outcomes, morbidity, and mortality.
Conclusion
Ischemic stroke treatment options have advanced beyond just medical therapies including IV TPA. The clinical team must recognize EVT as an advanced ischemic stroke treatment that is available in some stroke centers across the country. More importantly, the nurse plays a vital role in assisting the neurological team with obtaining detailed symptom presentation and time frames, as well as frequently monitoring vital and neurological statuses and being cognizant of complications and urgent interventions if needed.
References + Disclaimer
- American Stroke Association (2012, March 9) “Acute Ischemic Stroke Initiative” https://www.stroke.org/en/professionals/stroke-resource-library/acute-treatment
- Medscape (2021, March 9) “alteplase (TPA) -Dosage and Indications for Acute Ischemic Stroke.” https://reference.medscape.com/drug/342287?src=mbl_msp_android&ref=share#0
- Balami, Joyce et al. (2018, June 13) “Complications of endovascular treatment for ischemic stroke: Prevention and management” International Journal of Stroke 13 (4) pp. 348-361 https://doi.org/10.1177/1747493017743051
- McCusker, M.W et al. (2015, December) “Endovascular treatment for acute ischemic stroke with large vessel occlusion: The experience of a regional stroke service” Clinical Radiology 75 (12) pp. 1408-1413 https://doi.org/10.1016/j.crad.2015.08.007
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate

