Course
2021 Texas License Renewal Bundle
Course Highlights
- In this course we will cover various topics, including ethics, forensics, geriatric care, Alzheimer’s disease, opioid abuse, and more!
- You’ll learn the basics of nursing jurisprudence and ethics and nursing forensics, as required by the Texas Board of Nursing.
- You’ll leave this course with a broader understanding of effective communication habits to implement in your daily practice.
About
Contact Hours Awarded: 20
Course By:
Multiple Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
This 2021 Texas License Renewal Bundle meets renewal requirements for Texas LPNs and RNs. Upon completion of this course, you will receive a certificate of completion for 20 CNE contact hours.
This course is accredited and approved by American Nurses Credentialing Center (ANCC) (Provider Number: P0614) and includes multiple interesting topics in one easy course.
Course Outline:
- Texas Nursing Jurisprudence and Ethics (Meets TX BON Requirement)
- Texas Nursing Forensics (Meets TX BON Requirement)
- End of Life Care for Geriatric Patients (Meets TX BON Requirement)
- Alzheimer’s Nursing Care
- Nursing Care for Pediatric Patients by Stage of Development
- Opioid Abuse
- Vaping Induced Lung Injuries
- LGBTQ Cultural competence
- Coronavirus: Nursing Considerations
- Effective Communication in Nursing
- Nursing Documentation 101
- References
Texas Nursing Jurisprudence and Ethics
Introduction
The purpose of this course is to review nursing ethics and jurisprudence specifically as these relate to Texas state nursing practice and law. Each state nursing board works to promote the safety and welfare of clients in their state by ensuring nurses are competent to practice nursing safely. As outlined by Texas Board of Nursing continuing education requirements, Nursing Jurisprudence and Nursing Ethics Board Rule 216.3, all nurses, including APRNs, must complete the required two contact hours of CNE relating to nursing jurisprudence and ethics before the end of every third two-year licensing period. This requirement is applicable to licensing periods that began on or after January 1, 2014. All new nurses must also take and successfully pass the Nursing Jurisprudence Exam (NJE). (2,3)
Requirements also outline that education include information related to the Texas Nursing Practice Act, the Board’s rules including Standards of Nursing Practice, the Board’s position statements, principles of nursing ethics, and professional boundaries. Nurses are named in negligence and malpractice lawsuits that may claim unethical behavior/conduct, practice outside the scope of licensure or lack of nursing supervision. It is important that nurses understand their state nurse practice act, scope of practice of nurse licensure, standards of practice, ethics, and professional boundaries in order to avoid litigation. (2)

Self Quiz
Ask yourself...
- What is the number of contact hours required by the Texas Board of Nursing in Nursing Jurisprudence and Ethics before the end of every third two-year licensing period?
- What are the categories of required course information that must be contained?
The Texas Nursing Practice Act – Overview
Registered Nurse Scope of Practice
The Texas Nursing Practice Act (NPA) defines the legal scope of practice for professional registered nurses (RNs). “Professional nursing” means the performance of an act that requires substantial specialized judgment and skill, the proper performance of which is based on knowledge and application of the principles of biological, physical, and social science as acquired by a completed course in an approved school of professional nursing. The term does not include acts of medical diagnosis or the prescription of therapeutic or corrective measures. Professional nursing involves: (all from 12)
- the observation, assessment, intervention, evaluation, rehabilitation, care, and Counsel, or health teachings of a person who is ill, injured, infirm, or experiencing a change in normal health processes.
- the maintenance of health or prevention of illness.
- the administration of a medication or treatment as ordered by a physician, podiatrist, or dentist.
- the supervision or teaching of nursing.
- the administration, supervision, and evaluation of nursing practices, policies, and procedures.
- the requesting, receiving, signing for, and distribution of prescription drug samples to patients at practices at which an advanced practice registered nurse is authorized to sign prescription drug orders as provided by Subchapter B, Chapter 157.
- the performance of an act delegated by a physician under Section 157.0512, 157.054, 157.058, or 157.059.
- the development of the nursing care plan.
The RN takes responsibility and accepts accountability for practicing within the legal scope of practice and is prepared to work in all health care settings and may engage in the independent nursing practice without supervision by another health care provider. The RN, with a focus on patient safety, is required to function within the parameters of the legal scope of practice and in accordance with the federal, state, and local laws; rules and regulations; and policies, procedures, and guidelines of the employing health care institution or practice setting. The RN is responsible for providing safe, compassionate, and comprehensive nursing care to patients and their families with complex healthcare needs. (12)

Self Quiz
Ask yourself...
- What does the term “Professional nursing” mean?
- What is professional nursing performance based on?
- Does professional nursing include medical diagnosis or the prescription of therapeutic or corrective measures?
- Does professional nursing involve the supervision or teaching of nursing or the development of the nursing care plan?
- Can an RN engage in independent nursing practice without the supervision by another health care provider?
Texas Board Rules
Texas Board of Nursing, Chapter 217, Rule §217.11, Standards of Nursing Practice (4)
The Texas Board of Nursing is responsible for regulating the practice of nursing within the State of Texas for Vocational Nurses, Registered Nurses, and Registered Nurses with advanced practice authorization. The standards of practice establish a minimum acceptable level of nursing practice in any setting for each level of nursing licensure or advanced practice authorization. Failure to meet these standards may result in action against the nurse’s license even if no actual patient injury resulted. (4)
- Standards Applicable to All Nurses. All vocational nurses, registered nurses and registered nurses with advanced practice authorization shall:
- Know and conform to the Texas Nursing Practice Act and the Board’s rules and regulations as well as all federal, state, or local laws, rules or regulations affecting the nurse’s current area of nursing practice.
- Implement measures to promote a safe environment for clients and others.
- Know the rationale for and the effects of medications and treatments and shall correctly administer the same.
- Accurately and completely report and document:
- the client’s status including signs and symptoms.
- nursing care rendered.
- physician, dentist, or podiatrist orders.
- administration of medications and treatments.
- client response(s).
- Contacts with other health care team members concerning significant events regarding client’s status.
- Respect the client’s right to privacy by protecting confidential information unless required or allowed by law to disclose the information.
- Promote and participate in education and counseling to a client(s) and, where applicable, the family/significant other(s) based on health needs.
- Obtain instruction and supervision as necessary when implementing nursing procedures or practices.
- Make a reasonable effort to obtain orientation/training for competency when encountering new equipment and technology or unfamiliar care situations.
- Notify the appropriate supervisor when leaving a nursing assignment.
- Know, recognize, and maintain professional boundaries of the nurse-client relationship.
- Comply with mandatory reporting requirements of Texas Occupations Code Chapter 301 (Nursing Practice Act), Subchapter I, which include reporting a nurse:
- who violates the Nursing Practice Act or a board rule and contributed to the death or serious injury of a patient.
- whose conduct causes a person to suspect that the nurse’s practice is impaired by chemical dependency or drug or alcohol abuse.
- whose actions constitute abuse, exploitation, fraud, or a violation of professional boundaries.
- whose actions indicate that the nurse lacks knowledge, skill, judgment, or conscientiousness to such an extent that the nurse’s continued practice of nursing could reasonably be expected to pose a risk of harm to a patient or another person, regardless of whether the conduct consists of a single incident or a pattern of behavior.
- except for minor incidents (Texas Occupations Code §§301.401(2), 301.419, 22 TAC §217.16), peer review (Texas Occupations Code §§301.403, 303.007, 22 TAC §217.19), or peer assistance if no practice violation (Texas Occupations Code §301.410) as stated in the Nursing Practice Act and Board rules (22 TAC Chapter 217).
- Provide, without discrimination, nursing services regardless of the age, disability, economic status, gender, national origin, race, religion, health problems, or sexual orientation of the client served.
- Institute appropriate nursing interventions that might be required to stabilize a client’s condition and/or prevent complications.
- Clarify any order or treatment regimen that the nurse has reason to believe is inaccurate, non-efficacious or contraindicated by consulting with the appropriate licensed practitioner and notifying the ordering practitioner when the nurse makes the decision not to administer the medication or treatment.
- Implement measures to prevent exposure to infectious pathogens and communicable conditions.
- Collaborate with the client, members of the health care team and, when appropriate, the client’s significant other(s) in the interest of the client’s health care.
- Consult with, utilize, and make referrals to appropriate community agencies and health care resources to provide continuity of care.
- Be responsible for one’s own continuing competence in nursing practice and individual professional growth.
- Make assignments to others that take into consideration client safety and that are commensurate with the educational preparation, experience, knowledge, and physical and emotional ability of the person to whom the assignments are made.
- Accept only those nursing assignments that take into consideration client safety and that are commensurate with the nurse’s educational preparation, experience, knowledge, and physical and emotional ability.
- Supervise nursing care provided by others for whom the nurse is professionally responsible.
- Ensure the verification of current Texas licensure or other Compact State licensure privilege and credentials of personnel for whom the nurse is administratively responsible, when acting in the role of nurse administrator.
- Standards Specific to Vocational Nurses. The licensed vocational nurse practice is a directed scope of nursing practice under the supervision of a registered nurse, advanced practice registered nurse, physician’s assistant, physician, podiatrist, or dentist. Supervision is the process of directing, guiding, and influencing the outcome of an individual’s performance of an activity. The licensed vocational nurse shall assist in the determination of predictable healthcare needs of clients within healthcare settings and:
- Shall utilize a systematic approach to provide individualized, goal-directed nursing care by:
- collecting data and performing focused nursing assessments.
- participating in the planning of nursing care needs for clients.
- participating in the development and modification of the comprehensive nursing care plan for assigned clients.
- implementing appropriate aspects of care within the LVN’s scope of practice.
- assisting in the evaluation of the client’s responses to nursing interventions and the identification of client needs.
- Shall assign specific tasks, activities, and functions to unlicensed personnel commensurate with the educational preparation, experience, knowledge, and physical and emotional ability of the person to whom the assignments are made and shall maintain appropriate supervision of unlicensed personnel.
- May perform other acts that require education and training as prescribed by board rules and policies, commensurate with the licensed vocational nurse’s experience, continuing education, and demonstrated licensed vocational nurse competencies.
- Shall utilize a systematic approach to provide individualized, goal-directed nursing care by:
- Standards Specific to Registered Nurses. The registered nurse shall assist in the determination of healthcare needs of clients and shall:
- Utilize a systematic approach to provide individualized, goal-directed, nursing care by:
- performing comprehensive nursing assessments regarding the health status of the client.
- making nursing diagnoses that serve as the basis for the strategy of care.
- developing a plan of care based on the assessment and nursing diagnosis.
- implementing nursing care.
- evaluating the client’s responses to nursing interventions.
- Delegate tasks to unlicensed personnel in compliance with Chapter 224 of this title, relating to clients with acute conditions or in acute are environments, and Chapter 225 of this title, relating to independent living environments for clients with stable and predictable conditions.
- Utilize a systematic approach to provide individualized, goal-directed, nursing care by:
- Standards Specific to Registered Nurses with Advanced Practice Authorization. Standards for a specific role and specialty of advanced practice nurse supersede standards for registered nurses where conflict between the standards, if any, exist. In addition to paragraphs (1) and (3) of this subsection, a registered nurse who holds authorization to practice as an advanced practice nurse (APN) shall:
- Practice in an advanced nursing practice role and specialty in accordance with authorization granted under Board Rule Chapter 221 of this title (relating to practicing in an APN role; 22 TAC Chapter 221) and standards set out in that chapter.
- Prescribe medications in accordance with prescriptive authority granted under Board Rule Chapter 222 of this title (relating to APNs prescribing; 22 TAC Chapter 222) and standards set out in that chapter and in compliance with state and federal laws and regulations relating to prescription of dangerous drugs and controlled substances. (4)

Self Quiz
Ask yourself...
- Why is it important that a nurse know the rationale for and the effects of medications and treatments before administering these to a client?
- Are there negative consequences if a nurse is not trained to perform a task or procedure? If so, what are 1-2 consequences of lack or training or errors?
- How do nurses utilize a systematic approach to providing individualized, goal-directed, nursing care?
The Board’s Position Statements
15.28 The Registered Nurse Scope of Practice (See also the LVN Scope of Practice) (10)
The Board of Nursing recommends that all nurses utilize the Scope of Practice Decision-Making Model (DMM) when deciding if an employer’s assignment is safe and legally within the nurse’s scope of practice. (10)
The Texas Board of Nursing (BON or Board) is authorized by the Texas Legislature to regulate the nursing profession to ensure that every licensee is competent to practice safely. The Texas Nursing Practice Act (NPA) defines the legal scope of practice for professional registered nurses (RN).
The RN takes responsibility and accepts accountability for practicing within the legal scope of practice, is prepared to work in all health care settings, and may engage in the independent nursing practice without supervision by another health care provider. With a focus on patient safety, the RN is required to function within the parameters of the legal scope of practice and in accordance with the federal, state, and local laws, rules, and regulations. In addition, the RN must comply with policies, procedures and guidelines of the employing health care institution or practice setting. The RN is responsible for providing safe, compassionate, and comprehensive nursing care to patients and their families with complex healthcare needs. (10)
The purpose of this position statement is to provide direction and recommendations for nurses and their employers regarding the safe and legal scope of practice for RNs and to promote an understanding of the differences in the RN programs of study and between the RN and LVN levels of licensure. The LVN scope of practice is interpreted in Position Statement. (10)
Every nursing education program in the state of Texas is required to ensure that their graduates exhibit competencies outlined in the Board’s Differentiated Essential Competencies of Graduates of Texas Nursing Programs Evidenced by Knowledge, Clinical Judgements, and Behaviors. These competencies are included in the program of study so that every graduate has the knowledge, clinical judgment, and behaviors necessary for RN entry into safe, competent, and compassionate nursing care. The DECs serve as a guideline for employers to assist RNs as they transition from the educational environment into nursing practice. As RNs enter the workplace, the DECs serve as the foundation for the development of the RN scope of practice. (10)
Completion of ongoing, informal continuing nursing education offerings and on-the-job trainings in a RN’s area of practice serves to develop, maintain, and expand competency. Because the RN scope of practice is based upon the educational preparation in the RN program of study, there are limits to the expansion of the scope. The Board believes that for a nurse to successfully make a transition from one level of nursing practice to another requires the nurse to complete a formal education program. (10)
The RN Scope of Practice
The professional RN is an advocate for the patient and the patient’s family and promotes safety by practicing within the NPA and the BON Rules and Regulations. The RN provides nursing services that require substantial specialized judgment and skill. The planning and delivery of professional nursing care is based on knowledge and application of biological, physical, and social science principles as acquired by a completed course of study in an approved school of professional nursing. Unless licensed as an advanced practice registered nurse, the RN scope of practice does not include acts of medical diagnosis or the prescription of therapeutic or corrective measures. RNs utilize the nursing process to establish the plan of care in which nursing services are delivered to patients. The level and impact of the nursing process differs between the RN and LVN as well as between the different levels of RN education. (10,11)
Assessment
The comprehensive assessment is the first step and lays the foundation for the nursing process. The comprehensive assessment is the initial and ongoing, extensive collection, analysis, and interpretation of data. Nursing judgment is based on the assessment findings. The RN uses clinical reasoning and knowledge, evidence-based outcomes, and research as the basis for decision-making and comprehensive care.
Based upon the comprehensive assessment, the RN determines the physical and mental health status, needs, and preferences of culturally, ethnically, and socially diverse patients and their families using evidence-based health data and a synthesis of knowledge. Surveillance is an essential step in the comprehensive assessment process. The RN must anticipate and recognize changes in patient conditions and determines when reassessments are needed. (10,11)
Nursing Diagnosis/Problem Identification/Planning
The second step in the nursing process is nursing diagnosis and problem identification. The role of the RN is to synthesize comprehensive assessment data to identify problems, formulate goals/outcomes, and develop plans of care for patients, families, populations, and communities using information from evidence-based practice and published research in collaboration with these groups and the interdisciplinary health care team.
The third step in the nursing process is planning. The RN synthesizes the data collected during the comprehensive assessment to identify problems, make nursing diagnoses, and formulate goals, teaching plans, and outcomes. A nursing plan of care for patients is developed by the RN, who has the overall responsibility to coordinate nursing care for patients. Teaching plans address health promotion, maintenance, restoration, and prevention of risk factors. The RN utilizes evidence-based practice, published research, and information from patients and the interdisciplinary health care team during the planning process. (10,11)
Implementation
Implementing the plan of care is the fourth step in the nursing process. The RN may begin, deliver, assign, or delegate certain interventions within the plan of care for patients within legal, ethical, and regulatory parameters and in consideration of health restoration, disease prevention, wellness, and promotion of healthy lifestyles.
The RN’s duty to patient safety when making assignments to other nurses or when delegating tasks to unlicensed staff is to consider the education, training, skill, competence, and physical and emotional abilities of those to whom the assignments or delegation is made. The RN is responsible for reasonable and prudent decisions regarding assignments and delegation. The RN scope of practice may include the supervision of LVNs or other RNs. Supervision of LVN staff is defined as the process of directing, guiding, and influencing the outcome of an individual’s performance and activity. The RN may have to directly observe and evaluate the nursing care provided depending on the LVN’s skills and competence, patient conditions, and level of urgency in emergent situations. (10,11)
The RN may determine when it is appropriate to delegate tasks to unlicensed personnel and maintains accountability for how the unlicensed personnel performs the tasks. The RN is responsible for supervising the unlicensed personnel when tasks are delegated. The proximity of supervision is dependent upon patient conditions and the skill level of the unlicensed personnel. In addition, teaching and counseling are interwoven throughout the implementation phase of the nursing process. (10,11)
Evaluation and Reassessment
A critical and final step in the nursing process is evaluation. The RN evaluates and reports patient outcomes and responses to therapeutic interventions in comparison to benchmarks from evidence-based practice and research findings and plans any follow-up care and referrals to appropriate resources that may be needed. The evaluation phase is one of the times when the RN reassesses patient conditions and determines if interventions were effective and if any modifications to the plan of care are necessary. (10,11)
Essential Skills Used in the Nursing Process
Communication
Communication is an essential and fundamental component used during the nursing process. The RN must communicate verbally, in writing, or electronically with members of the healthcare team, patients, and their families in all aspects of the nursing care provided to patients. These communications must be appropriately documented in the patient record or nursing care plan. Because RNs plan, coordinate, initiate, and implement a multidisciplinary team’s approach to patient care, collaboration is crucial to the communication process. When patient conditions or situations exceed the RN’s level of competency, the RN must be prepared to seek out other RNs with greater competency or other health care providers with differing knowledge and skillsets and actively cooperate to ensure patient safety. (10,11)
Clinical Reasoning
Clinical reasoning is another integral component in the nursing process. RNs use critical thinking skills to problem-solve and make decisions in response to patients, their families, and the healthcare environment. RNs are accountable and responsible for the quality of nursing care provided and must exercise prudent and professional nursing judgment to ensure the standards of nursing practice are always met. (10,11)
Employment Setting
When an employer hires an RN to perform a job, the RN must ensure that it is safe and legal. Caution must be exercised not to overstep the legal parameters of nursing practice when an employer may not understand the limits of the RN scope of practice and makes an assignment that is not safe. The RN must determine before he or she engages in an activity or assignment whether he or she has the education, training, skill, competency, and physical and emotional ability to safely carry out the activity or assignment. The RN’s duty is to always provide safe, compassionate, and comprehensive nursing care to patients. (10,11)
Summary of Scope of Practice
The RN, with a focus on patient safety, is required to function within the parameters of the legal scope of practice and in accordance with the federal, state, and local laws; rules and regulations; and policies, procedures, and guidelines of the employing health care institution or practice setting. The RN functions under his or her own license and assumes accountability and responsibility for the quality of care provided to patients and their families according to the standards of nursing practice. The RN demonstrates responsibility for continued competence in nursing practice and develops insight through reflection, self-analysis, self-care, and lifelong learning. (10,11)
The table below offers a brief synopsis of how the scope of practice for nurses differs based on educational preparation and level of licensure. These are minimum competencies but also set limits on what the LVN or RN can do at his or her given level of licensure, regardless of experience. (10,11)
Synopsis of Differences in Scope of Practice for Licensed Vocational, Associate, Diploma and Baccalaureate Degree Nurses (4)
| Nursing Practice | LVN Scope of Practice Directed/Supervised Role | ADN or Diploma RN Scope of Practice Independent Role | BSN RN Scope of Practice Independent Role |
| Education |
|
|
|
| Setting |
|
|
|
| Assessment |
|
|
|
| Nursing Diagnosis/ Problem Identification/ Planning |
|
|
|
| Implementation |
|
|
|
Evaluation |
|
|
|
Nursing board Position Statements are not laws, but they provide direction for nurses on issues of concern to the Board relevant to the protection of the public. These Position Statements are reviewed annually for relevance and accuracy to current practice, the Nurse Practice Act, and Board of Nursing rules. Examples of Position Statements include the following: (9)
- Nurses Carrying out Orders from Physician Assistants
- Role of the Licensed Vocational Nurse in the Pronouncement of Death
- LVNs Engaging in IV Therapy, Venipuncture, or PICC Lines
- Educational Mobility
- Nurses with Responsibility for Initiating Physician Standing Orders
- Board Rules Associated with Alleged Patient “Abandonment”
- The Role of LVNs & RNs in Management and/or Administration of Medications via Epidural or Intrathecal Catheter Routes
- The Role of the Nurse in Moderate Sedation
- Performance of Laser Therapy by RN’s or LVNs
- Continuing Education: Limitations for Expanding Scope of Practice
- Delegated Medical Acts
- Use of American Psychiatric Association Diagnoses by LVN, RNs, or APRNs
- Role of LVNs & RNs As School Nurse
- Duty of a Nurse in any Practice Setting
- Board’s Jurisdiction Over a Nurse’s Practice in Any Role and Use of the Nursing Title
- Development of Nursing Education Programs
- Texas Board of Nursing/Board of Pharmacy Joint Position Statement on Medication Errors
- Nurses Carrying Out Orders from Advanced Practice Registered Nurses (APRN)
- Nurses Carrying Out Orders from Pharmacists for Drug Therapy Management
- Registered Nurses in the Management of an Unwitnessed Arrest in a Resident in a Long-Term Care Facility (9)

Self Quiz
Ask yourself...
- What are advantages for nurses to consistently use the nursing process during care and documentation of care of clients?
- How could communication breakdown among employee nurse team members impact a client’s care?
- Are nursing board Position Statements laws?
- Name one example of a nursing board Position Statement.
- What do RNs use to problem-solve and make decisions regarding care of clients?
Principles of Nursing Ethics
Professional Boundaries
15.29 Professional Boundaries including use of social media by nurses (7)
The purpose of this Position Statement is to provide guidance to nurses regarding expectations related to professional boundaries, inclusive of social media, and to provide nurses with guidance to prevent boundary violations. (7)
The Texas Board of Nursing (BON or Board), in keeping with its mission to protect the public health, safety, and welfare, holds nurses accountable for knowing, recognizing, and maintaining professional boundaries of the nurse-patient/client relationship. The term, professional boundaries, is defined as the appropriate limits which should be established by the nurse in the nurse/client relationship due to the nurse’s power and the patient’s vulnerability. Professional boundaries refer to the provision of nursing services within the limits of the nurse/client relationship, which promote the client’s dignity, independence, and best interests and refrain from inappropriate involvement in the client’s personal relationships and/or the obtainment of the nurse’s personal gain at the client’s expense. (7)
The National Council of State Boards of Nursing (NCSBN) defines professional boundaries as the spaces between the nurse’s power and the patient’s vulnerability. The power of the nurse comes from the nurse’s professional position and access to sensitive personal information. The difference in personal information the nurse knows about the patient versus personal information the patient knows about the nurse creates an imbalance in the nurse-patient relationship. Nurses should make every effort to respect the power imbalance and ensure a patient-centered relationship. (7)
Common to the definition of professional boundaries from the Texas Board of Nursing and from the NCSBN is that a nurse abstains from personal gain at the client’s expense and the nurse refrains from inappropriate involvement with the patient or the patient’s family. (7)
Duty of a Nurse in Maintenance of Professional Boundaries
There is a power differential between the nurse and the patient. The patient depends on the knowledge of the nurse and relies on the nurse to advocate for the patient and to ensure actions are taken in the patient’s best interest. The nurse has a duty to protect the patient, including establishing and maintaining professional boundaries in the nurse-patient/client relationship. Under or over-involvement can be harmful to the patient and may interfere with the nurse-patient relationship. Visualizing the two ends of the spectrum may assist the nurse in knowing, recognizing, and maintaining the professional boundaries of nurse-patient relationships. (7)
Patients each have their own unique needs and abilities. The boundary line for any one patient may change over time and may not be the same as the boundary line for another patient. It is up to the nurse to assess the patient and recognize the patient’s needs, adjusting the nursing care accordingly. Every nurse is responsible for knowing, recognizing, and maintaining the professional boundaries of the nurse-client relationship. (7)
Boundary Violations
A violation of professional boundaries is one element of the definition of “conduct subject to reporting [Tex. Occ. Code Sec. 301.401(1)(C)]. A professional boundary violation is also considered unprofessional conduct [22 TAC §217.12 (6)(D)]. Some of the specific categories of professional boundary violations include, but are not limited to, physical, sexual, emotional, or financial boundary violations. (7)
Use of Social Media
The use of social media and other electronic communication is expanding exponentially as the number of social media outlets, platforms, and applications available continues to increase. Nurses play a significant role in the identification, interpretation, and transmission of knowledge and information within healthcare. As technological advances continue to expand connectivity and communication, rapid knowledge exchange and dissemination can pose risks to both patients and nurses. While the Board recognizes that the use of social media can be a valuable tool in healthcare, there are potentially serious consequences if used inappropriately. A nurse’s use of social media may cause the nurse to unintentionally blur the lines between the nurse’s professional and personal life. (7)
Online postings may harm patients if protected health information is disclosed. In addition, social media postings may reflect negatively on individual nurses, the nursing profession, the public’s trust in the nursing profession, or the employer and may jeopardize careers. In a survey by the NCSBN, many of the responding boards reported that they had received complaints about nurses inappropriately using social media sites. The survey results indicated that nurses have been disciplined by boards, fired by employers, and criminally charged for the inappropriate or unprofessional use of social media. (7)
To ensure the mission to protect and promote the welfare of the people of Texas, the Texas Board of Nursing supports both the guidelines and principles of social media use by the NCSBN and American Nurses Association. In accordance with the NCSBN guidelines and Board rules, it is the Board’s position that: (7)
Nurses have an ethical and legal obligation to maintain patient privacy and confidentiality at all times. When using social media, nurses do not identify patients by name or post or publish information that may lead to the identification of a patient. Limiting access to postings through privacy settings is not sufficient to ensure privacy. Nurses must promptly report any identified breach of confidentiality or privacy.
Nurses maintain professional boundaries in the use of electronic media. The nurse has an obligation to establish, communicate and enforce professional boundaries with patients in the online environment. Nurses do not refer to patients in a disparaging manner, even if the patient is not identified or transmit information that may be reasonably anticipated to violate patient rights to confidentiality or privacy or otherwise degrade or embarrass the patient. (7)
Nurses must provide nursing services without discrimination and do not make threatening, harassing, profane, obscene, sexually explicit, racially derogatory, homophobic, or other offensive comments. (7)
Nurses must be aware of and comply with all laws and rules, including employer policies regarding the use of electronic devices, including employer-owned computers, cameras, and the use of personal devices in the workplace. In addition, nurses must ensure appropriate and therapeutic use of all patient-related electronic media, including patient-related images, photos, or videos, in accordance with applicable laws, rules, and institutional policies and procedures. (7)
The use of social media can be of tremendous benefit to nurses and patients alike, for example, the dissemination of public safety announcements. However, nurses must be aware of the potential consequences of disclosing patient-related information via social media. Nurses must always maintain professional standards, boundaries, and compliance with local, state, and federal laws. All nurses have an obligation to protect their patient’s privacy and confidentiality which extends to all environments, including the social media environment. (7)
The following are ways to avoid problems when using social media:
- Never post any healthcare-related images, client information, or even general client information.
- Never use your organization’s name, a client or family member’s name, post content about or speak for your employer unless you are authorized by your organization to follow their specific policy and procedures.
- Never post any comments about a client, even if the client is not named.
- Never post photos or videos of your healthcare organization or clients.
- Never post any comments about your employer or other team members.
- Never use obscenity, profanity, racial slurs, sexually inappropriate comments, homophobic comments, threats, harassing/abusive language, or any other offensive comments. Never post any image that contains the above content.
Prevention of Boundary Violations
The ability of a client to rely on employees as concerned and caring individuals who remain objective in their guidance is one of the tents of a safe, therapeutic relationship. When staff interacts with patients in a personal manner, the relationship may no longer be objectively therapeutic. Accepting gifts, financial transactions, and romantic entanglement could lead to various negative consequences for an organization, employee, or client. Many organizations enforce a policy of non-fraternization between employees and current or former clients. While there are exceptions, the expectation is that employees are not to establish a personal relationship with a current or former client. Organizations do recognize that there are times when peers, friends, family, or neighbors of employees seek treatment. In these circumstances, it is important that the relationship remains of the nature it was prior to admission if in the client’s best interest, and the treatment plan should address the relationship to best meet the therapeutic needs of the client. Employees should also notify a supervisor when an individual with whom he or she has a relationship is admitted for treatment. (7)
Texas Nurses are required to comply with mandatory reporting requirements of Texas Occupations Code Chapter 301 NPA Subchapter I, which include reporting a nurse: (7)
- Who violates the NPA or a board rule and contributed to the death or serious injury of a patient.
- Whose conduct causes a person to suspect that the nurse’s practice is impaired by chemical dependency or drug or alcohol abuse.
- Whose actions constitute abuse, exploitation, fraud, or a violation of professional boundaries.
- Whose actions indicate that the nurse lacks knowledge, skill, judgment, or conscientiousness to such an extent that the nurse’s continued practice of nursing could reasonably be expected to pose a risk of harm to a patient or another person, regardless of whether the conduct consists of a single incident or a pattern of behavior.
Exception is for minor incidents, peer review, or peer assistance if no practice violation as stated in the Nursing Practice Act and Board rules. (7)
Organizations also take many precautions to ensure appropriate employee-client relationships to include:
- Criminal background checks of employees
- Employee, student, and volunteer education regarding therapeutic boundaries and issues and consequences of any violations
- Mandatory, supportive, and confidential reporting of any violation
Employee supervision also includes the identification of early signals that an employee may be crossing therapeutic boundaries and the institution of appropriate interventions. Employees educate clients regarding the importance of maintaining a therapeutic relationship and appropriate boundaries. Organizations work to ensure adequate supervision of staff and appropriate supervision of clients, such as increased observation or same-gender staff working with a client when appropriate.
There must be mandatory reporting by any employee who becomes aware of a boundary violation. The employee should report this immediately to their supervisor, who will evaluate the nature and severity of the claim and initiate an investigation of the situation. The immediate supervisor, in conjunction with Human Resources and Risk Management, will determine whether an accused employee should be put on immediate leave pending investigation results and whether mandatory reporting of the allegations to outside agencies is required. Legal Counsel may also be consulted when necessary. An employer may not suspend or terminate the employment of, or otherwise, discipline, retaliate or discriminate against, a person who reports, in good faith, or who advises a nurse of the nurse’s rights and obligations.

Self Quiz
Ask yourself...
- Why is it important for a nurse to maintain professional and appropriate boundaries with a client?
- Name two examples of how social media may cause a nurse to blur the lines between his/her personal and professional life?
- Is reporting of boundary violations mandatory? If so, name two examples of when a nurse should report.
- How do organizations take precautions to ensure appropriate employee-client relationships?
Unprofessional Conduct – Rule §217.12
The following unprofessional conduct rules are intended to protect clients and the public from incompetent, unethical, or illegal conduct of licensees. The purpose of these rules is to identify behaviors in the practice of nursing that are likely to deceive, defraud, or injure clients or the public. Actual injury to a client need not be established. These behaviors include but are not limited to: (all from 5)
- Unsafe practice – actions or conduct including, but not limited to:
– Carelessly failing, repeatedly failing, or exhibiting an inability to perform vocational, registered, or advanced practice nursing in conformity with the standards of a minimum acceptable level of nursing practice set out in §217.11 of this chapter.
– Failing to conform to generally accepted nursing standards in applicable practice settings.
– Improper management of client records.
– Delegating or assigning nursing functions or a prescribed health function when the delegation or assignment could reasonably be expected to result in unsafe or ineffective client care.
– Accepting the assignment of nursing functions or a prescribed health function when the acceptance of the assignment could be reasonably expected to result in unsafe or ineffective client care.
– Failing to supervise the performance of tasks by any individual working pursuant to the nurse’s delegation or assignment.
– Failure of a clinical nursing instructor to adequately supervise or to assure adequate supervision of student experiences.
- Failure of a chief administrative nurse to follow standards and guidelines required by federal or state law or regulation or by facility policy in providing oversight of the nursing organization and nursing services for which the nurse is administratively responsible.
- Failure to practice within a modified scope of practice or with the required accommodations, as specified by the Board in granting an encumbered license or any stipulated agreement with the Board.
- Conduct that may endanger a client’s life, health, or safety.
- Inability to Practice Safely – a demonstration of actual or potential inability to practice nursing with reasonable skill and safety to clients by reason of illness, use of alcohol, drugs, chemicals, or any other mood-altering substances, or as a result of any mental or physical condition.
- Misconduct – actions or conduct that include, but are not limited to:
– Falsifying reports, client documentation, agency records, or other documents.
– Failing to cooperate with a lawful investigation conducted by the Board.
– Causing or permitting physical, emotional, or verbal abuse or injury or neglect to the client or the public, or failing to report same to the employer, appropriate legal authority and/or licensing Board.
– Violating professional boundaries of the nurse/client relationship including but not limited to physical, sexual, emotional, or financial exploitation of the client or the client’s significant other(s).
– Engaging in sexual conduct with a client, touching a client in a sexual manner, requesting, or offering sexual favors, or language or behavior suggestive of the same.
– Threatening or violent behavior in the workplace.
– Misappropriating, in connection with the practice of nursing, anything of value or benefit, including but not limited to, any property, real or personal of the client, employer, or any other person or entity, or failing to take precautions to prevent such misappropriation.
– Providing information, which was false, deceptive, or misleading in connection with the practice of nursing.
– Failing to answer specific questions or providing false or misleading answers in a licensure or employment matter that could reasonably affect the decision to license, employ, certify, or otherwise utilize a nurse.
– Offering, giving, soliciting, or receiving, or agreeing to receive, directly or indirectly, any fee or other consideration to or from a third party for the referral of a client in connection with the performance of professional services.
- Failure to pay child support payments as required by the Texas Family Code §232.001, et seq.
- Drug diversion – diversion or attempts to divert drugs or controlled substances.
- Dismissal from a board-approved peer assistance program for noncompliance and referral by that program to the Board.
- Other drug-related actions or conduct that include, but are not limited to:
– Use of any controlled substance or any drug, prescribed or unprescribed, or device or alcoholic beverages while on duty or on call and to the extent that such use may impair the nurse’s ability to safely conduct to the public the practice authorized by the nurse’s license.
– Falsification of or making incorrect, inconsistent, or unintelligible entries in any agency, client, or other record pertaining to drugs or controlled substances.
– Failing to follow the policy and procedure in place for the wastage of medications at the facility where the nurse was employed or working at the time of the incident(s).
– A positive drug screen for which there is no lawful prescription.
– Obtaining or attempting to obtain or deliver medication(s) through means of misrepresentation, fraud, forgery, deception and/or subterfuge.
- Unlawful practice – actions or conduct that include, but are not limited to:
– Knowingly aiding, assisting, advising, or allowing an unlicensed person to engage in the unlawful practice of vocational, registered, or advanced practice nursing.
– Violating an order of the Board, or carelessly or repetitively violating a state or federal law relating to the practice of vocational, registered, or advanced practice nursing, or violating a state or federal narcotics or controlled substance law.
– Aiding, assisting, advising, or allowing a nurse under Board Order to violate the conditions set forth in the Order.
– Failing to report violations of the Nursing Practice Act and/or the Board’s rules and regulations.
- Leaving a nursing assignment, including a supervisory assignment, without notifying the appropriate personnel.
There is a Texas State Board of Nursing Disciplinary Matrix that nurses can review to see the process followed when a review of a nurse’s conduct is necessary. The Board will consider public safety, the seriousness of the violation, and any aggravating or mitigating factors. Other factors considered include the presence of multiple violations, prior violations, and costs which could result in a more severe disciplinary action. (8)

Self Quiz
Ask yourself...
- Name two examples of unsafe nursing practice that will result in a nursing board review.
- Is violating boundaries of the employee-client relationship considered misconduct?
- Is failing to report violations of the Nursing Practice Act misconduct?
- Is failing to report violations of the Nursing Board’s rules and regulations misconduct?
Provisions of the Code of Ethics for Nurses
Provision 1
The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person. (1)
Provision 2
The nurse’s primary commitment is to the patient, whether an individual, family, group, community, or population. (1)
Provision 3
The nurse promotes, advocates for, and protects the rights, health, and safety of the patient. (1)
Provision 4
The nurse has authority, accountability, and responsibility for nursing practice, makes decisions, and takes action consistent with the obligation to provide optimal patient care. (1)
Provision 5
The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth. (1)
Provision 6
The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care. (1)
Provision 7
The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy. (1)
Provision 8
The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities. (1)
Provision 9
The profession of nursing, collectively through its professional organizations, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy. (1)

Self Quiz
Ask yourself...
- Who is a nurse primarily committed to?
- Name two examples of how a nurse advocates for a client.
- Name three ways that a nurse protects a client’s rights.
Case Study
Rachel is a 13-year-old adolescent female client admitted to an inpatient behavioral health unit for bipolar disorder, alcohol and marijuana abuse, and borderline personality disorder. The client has a history of sexual promiscuity, lying, and has alleged abuse and rape by history. Rachel approaches the Charge RN at bedtime, saying that an employee and she “have been having sex” many times over the course of two weeks and that she realizes now that “she should have told someone”. The alleged employee is currently on duty.
As Charge RN, how would you respond, and what are your next steps?
Conclusion
When a nurse is named in a negligence or malpractice lawsuit, it can create stress for the client, the employee, and the employer. A nurse maintaining professional, ethical, and jurisprudent conduct will help to ensure standards of practice are consistently followed. Maintaining appropriate boundaries with clients at all times helps maintain a therapeutic employee-client relationship. It is important that nurses understand their state nurse practice act, the scope of practice of nurse licensure, standards of practice, ethics, and professional boundaries in order to maintain professionalism, meet performance standards, and avoid a breach of duty, injury, and litigation.
Resources
Educational Requirements:
Texas Board of Nursing (2010), Differentiated Essential Competencies (DECs) of graduates of Texas Nursing Programs. (12)
Texas Occupations Code, Chapter 301 (12)
Nursing Practice Act (NPA) Section 301.002, Definitions (12)
Rule 217.11 - Standards of Nursing Practice (12)
Scope of Practice Position Statements: (12)
- Position Statement 15.28 The Registered Nurse Scope of Practice Web version for viewing
- Position Statement 15.14 – Duty of a Nurse Web version for viewing
- Position Statement 15.14 – Duty of a Nurse – HHSC/DADS/BON poster
For the complete list of position statements, click here. (12)
Texas Nursing Forensics
Introduction
In the United States, sexual assault was historically considered a judicial problem; however, it is now considered a major public health concern because of the health and psychological effects on individuals. The problem most notably emerged in the public eye in the 1960s with the women’s liberation movement. In recent times the #METOO movement has increased awareness of the problem, and many organizations have surfaced to assist the assaulted. This program will focus on the problem in rural areas in the state of Texas and how nurses working in these emergency departments can best assist sexually assaulted patients.
According to the Rape Abuse and Incest National Network (RAINN) (1), in less than every 80 seconds, a person is sexually assaulted. In 2015 the Texas Statewide Sexual Assault Prevalence Study found that 33.2% of adult Texans or 413,000 individuals reported having been sexually assaulted at some point during their lives. (2)
Assault can be the product of domestic abuse, gang violence, date rape, and incest. Assault can be inflicted on any age or gender and often occurs by someone who is related to or knows the assaulted. Sexual abuse, as described by the American Psychological Association (APA) “is unwanted sexual activity, with perpetrators using force, making threats or taking advantage of victims not able to give consent”. (3). Statistics show that more women and children are sexually assaulted than men, and that girls under 18 years of age are at the highest risk. According to RAINN (1), men and boys, especially college-age, are also at risk with transgender students at the highest risk of this group. Today many organizations deal with this issue and offer hope and assistance to those affected.
Not only does the impact of sexual assault affect the emotional and physical health of victims, but there are also major associated costs. These costs are incurred from:
- Emergency department visits
- Law enforcement time and wages
- Evidence collection and testing
- Court fees, including civil and federal lawsuits
- Loss of wages and health care costs of the affected
In 1996 the national cost of this problem was approximately $450 billion per year. (4) National Institute of Justice. Those numbers have jumped into the trillions of dollars in the last two decades. In Texas alone, the costs exceed $26,000,000 annually. (2)
In many parts of the United States, Sexual Assault Nurse Examiners (SANE), nurses who are expertly trained in performing forensic examinations and collection of evidence, are utilized (5). Since there is a lack of SANE nurses in rural Texas, registered nurses working in these emergency departments must learn the SANE process to perform the forensics exams and evidence collection by completing a 2-hour educational program.

Self Quiz
Ask yourself...
- Why do you think sexual assault has changed from a judicial problem to a health problem?
- How can nurses help to affect a decrease in costs in this health problem?
- What organizations in Texas can you connect with to learn more about sexual assault and how you can impact the problem?
- Where can you find more information on SANE programs?
Nursing’s Role
Sexual assault is an extremely traumatic experience. Those affected can have a wide range of issues, emotionally, spiritually, physically, and psychologically. While we may not address all of these issues in the initial visit to the emergency department, we must consider these concerns while the patient is in our care since we are often the first responders.
Compassion, empathy, and privacy are a hallmark of excellent practice in these situations. Many patients will experience shock and disbelief. “Why me? Will I be okay?” or “it’s no big deal, I’m fine”. (6). There may be “fear of responses from friends, family, colleagues the public and criminal justice providers.” (7) Rape victims may also have concerns about pregnancy, STDs, and HIV/AIDS. These patients may feel their world has turned upside down and fear if others know they may be scorned, told it was deserved, and fear their names could be made public (7). Patients may not want to talk about the assault, as reliving it could bring out unwanted emotions.
Active listening, believing what the patient tells you, validating their feelings, maintaining confidentiality, and honoring their decisions around what to do about the assault are a few of the methods the interviewing nurse should use. Since nurses are taught to treat the whole person rather than the “problem” alone, this skill is vital in caring for this group of patients. Repeating information back to the patient will help to elicit more precise information. It will also help in validating what the patient is telling you so an atmosphere of trust can be obtained.
Working with all personnel in the emergency department is also essential. From the paramedics, law enforcement officers, family, or anyone accompanying the patient to the physicians, social workers, and forensic medical examiners, each professional has a specific skill set and role in the patient’s care. Teamwork among these groups of individuals will provide for the best possible outcomes for the patient. In order to provide excellent care, all gender identities must be taken into consideration, as well as age and sexual orientation. No bias or judgment should ever be displayed to the patient. Customs, beliefs, religious and spiritual needs should also be considered during the visit.
If the patient arrives alone, the nurse should inquire if the patient wants a companion or an advocate to be present. An advocate could be a family member, a friend, a member of the clergy or a social worker. It will always be the patient’s choice. However, care must be taken for the patient to feel comfortable as recalling the events and having a family member or friend who is also emotionally involved, or even the assaulter, may deter the patient from complete openness and honesty. An interpreter should also be arranged if needed with the patient’s consent. If the patient has not alerted the local police, the nurse should inquire if they wish to report the assault and if so, the police should then be called. If available, a sexual assault response team or SART should be immediately contacted. It is of the utmost importance to remember that it is always the patient’s choice and consent in all situations surrounding the case.
Admitting the patient to a private room in a quiet area of the emergency department lessens interruptions from outside sources. When performing the initial assessment and gathering information, documentation must include a very detailed and complete history, including any physical trauma to the person’s body. The history should include any bruises, lacerations, or other visual injuries and how and when they occurred. The nurse should perform the interview slowly, giving the patient time to process and answer each question. The patient may or may not want to identify the person who assaulted them and should not be coerced into doing so.
A complete medical, surgical, and gynecologic history, in the case of a female patient, and any new symptoms occurring after the assault should be asked. Drug allergies, medications, and any alcohol or illegal drugs used at the time of the event are also documented. A compassionate and empathic tone should always be used to allow the patient to feel safe and understand there is no judgment of them from any person in the emergency department. Patients should be given the opportunity and encouraged to grieve and react during this time. They will need to feel comfortable enough to ask and answer questions throughout the interview.
In Texas, it is a law that the nurse obtains written consent from the patient. During the complete physical exam, the nurse will be charged with taking care that any physical evidence of the assault from clothing or body fluids is not disturbed. Also, during this time, suicidality and emotional supports should be assessed. Providing expert treatment for sexually assaulted patients is of utmost importance. When available, a SANE nurse will perform the forensic examination. This examination is vital to collect and preserve physical evidence from the patient while also assessing life and limb injuries. If a SANE nurse is unavailable, as in Texas’s rural areas, a “medical forensic examiner” will perform the examination.
During the physical assessment, the patient should be advised of every step before each part of the exam and be made aware that they have total control of what is happening. It is important that the nurse help the patient understand he or she always has the right to refuse any and all of the steps in the examination. When documenting the case, the nurse should use open-ended questions to elicit the patient’s best and clearest responses. Documentation must be complete and exact, including every stage of the assault with times, dates, and descriptions considering the patient’s emotional state and ability to recall. Using motivational interviewing and repeating back what the patient has stated is very helpful.
In the case of a minor, a parent will give the consent, and if no parent is available or is the assaulter, the child will be turned over to the appropriate child and family services in the state. If the assaulted patient has dementia or is an elder with cognitive issues and is therefore unable to consent, adult protective services should be contacted. (8) There are also rules governing military sexual offenses. Remember when documenting these cases, whether using handwritten or electronic medical records any and all information is subject to HIPPA.

Self Quiz
Ask yourself...
- What skills do you have that could best be used in these situations?
- How would you, as the initial contact, approach an individual who has been sexually assaulted?
- What skills would you need to learn or improve on to work with a person who has been sexually assaulted?
- Currently, do you feel capable of caring for a sexually assaulted patient without judgment and with compassion?
Forensic Law and Collection Process in the State of Texas
The Texas government code 420.031 (9) describes the protocol that must be taken to develop and protect evidence collection in a sexual assault case. Since a major part of Texas is rural, the code was enacted to protect and care for patients and the evidence in those areas where a SANE nurse is not available. In those cases, a medical forensic examiner may perform the exam and evidence collection.
A medical forensic examiner is described as any practitioner Medical Doctor, Registered Nurse, Nurse Practitioner, or Physician’s Assistant who has undergone a minimum of 2 hours of training in forensic evidence collection. The law outlines requirements in the collection and preservation of evidence. In 2019 the code was amended to require written informed consent from the patient or guardian for release of the evidence and must be gained prior to the history and physical. Obtaining consent also carries important psychological implications after a sexual assault since the patient’s right to consent was violated by the assaulter. Sexual assault examination teams should always be involved as early as possible.
In Texas, there is no statute of limitations on reporting sexual abuse of a child. For an adult (over 17 years of age) that statute ends ten years after the crime. However, during the investigation of the offense, if “biological matter” is collected and the matter:
- has not yet been subjected to forensic DNA testing.
- has been subjected to forensic DNA testing and the testing results show that the matter does not match the victim or any other person whose identity is readily ascertained.
- probable cause exists to believe that the defendant has committed the same or a similar sex offense against five more victims” there is no statute of limitations. (9)
Sexual assault evidence can be found in several areas, including the crime scene, the patient’s body, skin, hair, nails and clothing, and other items belonging to the patient (11). There is a specific kit used to collect this evidence. As described by RAINN, the kit is best known as a RAPE or Sexual Assault Evidence Kit (SAEK) and is inclusive of the items listed below:
- Bags and paper sheets to put on the floor and collect clothing or other evidence that may fall off the patient while undressing,
- A comb to collect evidence from hair,
- Forms for documentation,
- Envelopes and containers for the evidence
- Instructions on use of the kit, documenting guidelines
- Blood sampling materials and swabs.” (11)
Types of evidence collected are usually skin samples, scrapings from fingernails, and oral, genital, and anal swabbing internal and external. Directions on how to collect this evidence is included in the kit. The forensic examiner can also use special types of photography to document internal injuries. (11) Personal cameras should never be used. Remember, it is the law that the patient consent to each part of the exam.
As described by RAINN, prior to the forensic exam, it is best if the patient has not changed clothes, combed their hair, brushed their teeth, tried to clean the area, showered, or bathed, or used a restroom. If needing to use the restroom, a urine sample should be collected, educating the patient not to cleanse the perianal area. If they have already showered or bathed and have not arrived after the acute assault, emergency personnel need to educate the patient to keep the clothes they were wearing and any other belongings they had with them at the time of the assault in a paper bag in order to preserve the evidence. (11) If the patient comes to the emergency department up to 7 days after being sexually assaulted, the exam can still be performed. After the 7 days, it is at the forensic examiner’s discretion whether the exam should be performed. Collecting and protecting forensic evidence is a legal, moral, and professional responsibility (12)
Any medical witness who testifies in court is held in the highest regard and as experts in sexual assault. (5) Courts will closely scrutinize the chain of custody, and if broken, it can cause a conflict in the case and question of validity. Cases may be heard in criminal, civil, juvenile, military courts, or grand juries. If a forensics examiner is called to be a “fact” witness, no opinions on the case will be heard. Only the procedures that were performed on the patient will be admitted, and if the testifier is not the professional who performed the examination, they may be questioned regarding SANE protocols. If called upon to be an expert witness, the SANE nurse not only has knowledge of protocols but can educate and give opinions to the court. In either case, the necessity for excellent knowledge of SANE protocols is important. Nurses must be comfortable testifying in court as it is a rigorous and stress-provoking experience. Working with your organization’s lawyers and prosecutors as well as reviewing the case extensively will prepare the nurse to testify in a case. (5)

Self Quiz
Ask yourself...
- How would you obtain a SAEK kit if your emergency department does not have one?
- How would you familiarize yourself with what is contained in the kit?
- How well do you feel you could testify in court?
- Where in your facility can you find support if you had to testify?
Chain of Custody
In order to protect the patient and evidence for the courts, a chain of custody of the evidence must be followed precisely. Failure to comply does not mean the evidence is not admissible in the courts; however, the more complete the evidence, the better chance of conviction of the assaulter. Texas A&M’s nursing program offers a chain of evidence handbook outlining each step in the collection of evidence. The information below highlights the collection process from that handbook (8)
“Precise chain of custody must be maintained and well documented through the entire patient assessment and evidence collection process. Chain of custody documents includes the dates and times of each individual who handles every piece of evidence, from the time it is collected to the legal proceedings.” 2. Evidence must also be labeled with the patient’s name, date of birth, a unique identifier number from the institution, the examiner’s initials, date, and time.
Chain-of-custody documentation must include:
- Receipt of evidence
- Storage of the evidence
- Transfer of the evidence
- Date and time of each transfer
- The printed name and signature of each person in possession of the evidence
- Signatures of all persons transferring or receiving the evidence
- Swab and evidence collection
There should be two swabs used from each site.” (8)
Evidence must be kept in sight of the staff person collecting it at all times. After collected, the evidence must be dried and contained in the SAEK kit and sealed per kit instructions until it can be handed over to the appropriate law enforcement official and opened only by crime lab personnel. Each emergency department should have a locked storage space to provide temporary custody of collected evidence until it can be transferred to the appropriate persons or lab. If a patient is transferred to another facility, the chain of custody again must be documented according to the law.
The law in Texas allows an adult to choose whether to report the assault to law enforcement. If the choice is to not report, evidence will still be collected and preserved for up to 5 years post-assault. In the case of child sexual assault, elder abuse (over 65), or disabled persons, all medical personnel must report the case to law enforcement as mandatory reporters. Texas caregivers are also required to give patients an information sheet describing where to find appropriate services for the sexually assaulted. This document can be found on the Texas consumer protection website.

Self Quiz
Ask yourself...
- Where can you find more information on the Texas Code of law on sexual abuse?
- Why is it so important to maintain the chain of custody?
- If an assault patient decides not to report the case to the police, how would you handle that situation?
Physical and Emotional Issues Post Assault
After a sexual assault, patients can experience anxiety and depression, PTSD and turn to alcohol and/or substance abuse. There may be feelings of fear, denial, guilt, shame, loss of self, loss of control, and anger. (8) Their world has been turned upside down, and they feel life has stopped, and they cannot move forward. They may feel ashamed and wonder if, in some way, they were responsible. They may not feel safe in their own space and may lack trust.
In domestic cases, the patient may be concerned about their attacker. They may worry that their attacker will be prosecuted and sent away. Daily life can be disrupted to the point of self-isolation and loss of the patient’s job, family, and social life. A patient may become disabled to the point of homelessness and poverty. Many will feel the attack is transparent and that others can tell they have been assaulted just by looking at them. Flashbacks can occur at any time, and they may experience nightmares of being chased or attacked. They may also have constant thoughts of the abuse, causing insomnia and intense anxiety.
Sexually assaulted patients are more likely to contemplate and attempt suicide than those of other assaults. These issues can extend into long periods of time, with unknown triggers bringing flashbacks or repeated negative feelings. Patients need to be educated to understand that all of their feelings are normal to the trauma and understand that these feelings are temporary. Each person heals in different ways and in different timeframes. Ongoing support and therapy will assist the patient in recovery as well as self-help and group programs. There are many online, telephone, and in-person programs for victims as well as organizations to assist with ongoing issues. For example, the RAINN program can be helpful in advocating for patients and guiding them on their journey to recovery.
Many psychologists and therapists deal explicitly with sexual assault patients. The attorney general of the state of Texas website has information and resources for all crime victims. Having a trained sexual assault counselor at the emergency visit time can be of great assistance with the initial contact and subsequent referrals to professionals. Compassionate, empathic, and supportive care by emergency nurses at the initial contact can positively impact the patient’s road to a safe and healthy recovery.
Physical injuries must also be considered using clinical assessment, radiology, MRIs, and CT scans when necessary. Laboratory collection for STDs (sexually transmitted diseases), pregnancy in females, possible HIV, and other illness exposures are also a consideration during the physical exam and history taking. Follow-up care for these injuries with subsequent laboratory tests and appointments made with appropriate specialists should be made.
Ideally, the nurse could schedule a telephone call with the patient in 2-3 days to assess how they are doing and for continued support and referrals. At that time, the patient may have more questions or concerns that the nurse can help with and provide for follow-up care and resources. A list of educational programs and therapists who specialize in sexual assault and support groups should be supplied to the patient at the time of the visit and subsequent phone calls. There is no handbook on how to recover from trauma; it is an individual journey that is experienced solely by each person; however, there are many resources to assist a sexually assaulted patient at the time of the event and long after.

Self Quiz
Ask yourself...
- What skills would you need to care for the initial emotions of shock and disbelief of a sexually assaulted patient?
- What questions might you ask a patient in a follow-up phone call?
- Where would you find resources to assist patients that have been sexually assaulted?
Conclusion
Sexual assault has become a major and costly health problem in the United States. The state of Texas has implemented a code of laws to identify, protect and collect evidence from patients who have experienced this crisis. The utilization of SANE nurses is common in major metropolitan area hospitals, but many rural areas in that state are not equipped with the program. To properly care for these patients and collect and protect evidence appropriately, Texas has mandated education for those emergency department nurses not served by SANE personnel.
It is imperative that emergency department nurses become educated in the use of SAEK kits for evidence collection and chain of evidence protocols. The utilization of the SANE method allows for standardized care that is safe and protective of the patient and the patient’s rights. It protects evidence for investigation while helping to keep costs down.
End of Life Care for Geriatric Patients
What is End of Life Care?
End of life nursing care encompasses a wide range of aspects of care, to include symptom management, appropriate pain management, ensuring patient and family education and support during the death and dying process, providing culturally sensitive care, and ensuring the decision-making process remains ethical (6). Nurses are an integral part of the end of life process and should be sure to be an active advocate for their patients and families.
End of Life Care vs. Palliative Care
End of life care and palliative care are two terms that are used interchangeably but are two very different things. Palliative care refers to pain and symptom management during “any time in the trajectory of serious illness or injury and does not replace curative interventions” (8). This means that anyone experiencing a serious illness or injury can receive palliative care to manage symptoms and does not necessarily mean that they are beginning the dying process. Palliative care can be delivered as either a separate service or the primary care team and can be given in a variety of settings to include intensive care, inpatient wards, outpatient clinics, and long-term care or rehabilitation facilities. In contrast, end of life care (also known as hospice care) refers to patient care before and during the dying process. It may be initiated before, during or after curative treatment and is meant to focus on a patient’s comfort rather than a cure (8). End of life care can be provided in the comfort of the patient’s home, in a long-term care facility, or in a hospital.
End of Life Care Considerations
End of life care should be given to anyone who is “near the end of life and have stopped treatment to cure or control their disease” (13). It can also be considered for those who are undergoing a curative treatment.
Talking frankly about end of life care planning is important and should be done often in collaboration with patients and their families. Nurses should be active in this planning phase, ensuring that the patient and all involved family members understand the death and dying process, all available treatment options that have been presented by the health care team, and all the different methods available to control pain and symptoms. Talking about end of life options early is imperative – by broaching the subject before pain and symptom management become an issue, the nurse can ensure that the patient is an active participant in creating their care plan and final wishes.
Types of End of Life Care
End of life care planning can include a few different things:
Hospice Care
As was mentioned above, hospice care focuses on pain and symptom management during a chronic illness that will ultimately cause the patient to die. Also known as “comfort care,” hospice can be initiated in several instances:
- During a curative treatment
- If a patient wishes not to continue with curative treatment
- The curative treatment has failed
- The patient wishes not to pursue curative treatment
- After withdrawal of lifesaving interventions (ventilatory support, vasopressors, etc.)
Do Not Resuscitate (DNR)/Do Not Intubate (DNI)
A patient has the right to refuse resuscitation or intubation and mechanical ventilation, in the event that they would need it, if they are of sound mind and are able to make their own medical decisions. A Do Not Resuscitate (DNR) order is written by a medical doctor and instructs the health care team not to initiate cardiopulmonary resuscitation (CPR) if the patient experiences a cardiac or respiratory arrest. The order is written only after discussion with the patient. If the patient is not able to make medical decisions, a doctor may discuss options with a designated healthcare proxy. A DNR order does not cover any other lifesaving interventions. A Do Not Intubate (DNI) order is also written by a doctor and states that a patient does not wish to have an artificial airway placed should they experience respiratory arrest. It is possible for a patient to be a DNI but still wish to have CPR in the case of cardiac arrest (9).
Once a DNR/DNI order is in place, if it is at the patient’s request, the family cannot override it. If a patient has requested a DNR/DNI order but then changes their mind, they have the right to revoke it at any time. A DNR/DNI order must be respected, it is a legal, binding document. As such, verbal DNR/DNI requests from family members cannot be honored – the original signed order must be present for care providers to cease resuscitation attempts.
Advance Directive
An advance healthcare directive, also known as a living will, is a legal document that specifies what a person’s desires are regarding treatments and lifesaving interventions in the event that they become unconscious or are dying (9). A living will can include instructions on:
- The use of ventilators or other artificial respiratory support
- Initiation of CPR in the event of cardiac arrest
- The use of vasoactive medications
- Dialysis
- Organ or tissue donation
The advance directive may also name a health care proxy can make decisions for the patient if they become incapacitated.
In order to facilitate advance directive planning, nurses may wish to use a document called “5 Wishes.” 5 Wishes is a legal advance directive document that is written in lay language and helps patients to choose their end of life care and document it appropriately. This document is widely available in hospitals and other care facilities.
The Role of the Nurse in End of Life Planning
According to the position statement on end of life care from the American Nurses’ Association, nurses “are often ideally positioned to contribute to conversations about end of life care and decisions, including maintaining a focus on patients’ preferences, and to establish mechanisms to respect the patient’s autonomy” (7). Similarly, a statement entitled “The Right to Self Determination” from the Code of Ethics for Nurses with Interpretive Statements also emphasizes the nurse’s role in end of life planning and care:
“The importance of carefully considered decisions regarding resuscitation status, withholding and with-drawing life-sustaining therapies, forgoing nutrition and hydration, palliative care, and advance directives is widely recognized. Nurses assist patients as necessary with these decisions. Nurses should promote advance care planning conversations and must be knowledgeable about the benefits and limits of various advance directive documents. The nurse should provide interventions to relieve pain and other symptoms in the dying process consistent with palliative care standards and may not act with the sole intent of ending a patient’s life” (7).
What these statements say is that nurses have ethical roles and responsibilities that are fundamental to nursing practice. Nurses should ensure that both patients and family members understand the options and treatments that have been presented to them and should ensure that the patient’s autonomy is being respected throughout all aspects of their care. Nurses are primarily patient advocates, and this is especially crucial during the end of life stage. Nurse advocacy during this time can encompass anything from symptom and pain management, culturally sensitive care provision, and ethical decision making (6).
Talking to Patients and Families
Talking to a patient and their family about end of life care can be a huge challenge for nurses. In addition to managing patients’ and families’ emotions, nurses must manage their own emotions and approach the subject with professionalism as well as empathy.
Often, during the end of life planning phase, patients will go through the five stages of grief, as outlined in the book “On Death and Dying” by Elizabeth Kubler-Ross. The five stages of grief include (6):
1. Denial
Usually a temporary defense, patients may say that they are fine, or that this is some mistake.
2. Anger
Once the patient is no longer in denial, anger is often the next stage. It may be difficult to care for the patient during this stage, as they may misplace their angry feelings on their caregivers.
3. Bargaining
At this stage, the patient seeks ways to postpone death – often in the form of promising to reform a lifestyle in exchange for more life.
4. Depression
This stage may involve the refusal of treatments or visitors, and the disconnection from people, love, and affection.
5. Acceptance
The final stage, which is not reached by all patients. In this stage, the patient has come to terms with their mortality and has accepted that death will happen.
It is important for the nurse to understand these five stages, as most patients will be experiencing one or more of the stages during the end of life process.
Here are some helpful techniques for nurses to use when talking to patients about hospice or end of life planning, according to the American Academy of Family Physicians (10):
Make sure you have time.
While this may seem impossible while on a shift when you have other patients, it is imperative that a nurse allow enough time to have this difficult conversation. This is not a conversation that can be rushed – rushing through the conversation may make a nurse miss crucial details that the patient has shared.
Turn off your phone.
Minimizing distractions during these difficult conversations will ensure that the nurse can get ample information from this patient and family interaction.
Listen to the patient.
Above all, listen to what the patient is saying. Begin the conversation by asking what the patient and their doctor have already discussed. Be sure that the plan of care has been reviewed with the doctor prior to this conversation, then have the patient repeat their plan of care as they understand it. If there are major differences in the plan of care and what the patient says, this may warrant further conversation with the health care team to clarify and identify knowledge gaps.
Learn what the patient’s goals are.
Active listening is crucial during the conversation phase of end of life care planning. Once the nurse has determined that the patient understands the options that have been presented, it is vital to ask them what their goals are for palliative and comfort care. Understanding a patient’s goals can help identify what resources will be best suited for their individual needs.
Conversations surrounding end of life care should happen as soon as possible. Do not wait until the patient is no longer able to participate in the discussion. Encourage the presence of family members, but be sure to respect the patient’s wishes regarding who is involved in the planning process. Other members of the healthcare team that should be included in the planning process include social workers, patient navigators (if applicable in that setting), and any primary and specialist physicians involved in the patient’s care.
Caring for an End of Life Patient
Transitioning to End of Life Care
There may come a point during a patient’s hospital stay where it becomes evident that curative or life-supporting measures are no longer effective, thus necessitating the transition from curative treatment to comfort/end of life care. Of course, it is preferable that comfort care be initiated during the curative treatment – this makes the transition to end of life care somewhat easier, since the conversation and planning were ideally initiated before treatment began, and with the collaboration of the healthcare team, family, and patient.
Social Considerations
When preparing a patient and family for the end of life process, a nurse should be sure to consider several social perspectives of both the family and the patient:
Patient and family education.
This is crucial to ensuring that the end of life process goes smoothly for both the patient and any involved family members. It is imperative to assess the patient’s level of understanding of their diagnosis and all treatment plans. If a knowledge gap is identified, consider calling a meeting of the healthcare team to review the plan of care. The nurse should be present at as many planning meetings and patient conversations as possible. This way, the information is getting passed firsthand and nothing is lost in translation.
Physical location.
What are the patient’s wishes for where they want to be when they die? If the patient wishes to leave the hospital, every effort should be made to accommodate their wishes, should their clinical status allow it. At this point, social workers should be involved to coordinate home hospice care or transfer to an appropriate hospice facility.
Advance directives.
If the patient has an advance directive in place, what are their wishes? If the patient can participate in discussions surrounding end of life care, their autonomy should be respected. If the patient wishes to create an advance directive, the nurse should be sure to confirm the patient’s and family’s understanding of available options.
Clinical Considerations
Medically ineffective interventions.
This can also be called “futility of care.” According to the American Medical Association’s Code of Medical Ethics (11), these interventions may be requested by family members but are deemed inappropriate by the physician. According to the AMA, the following steps should be taken by the physician when dealing with a futility of care situation:
- “Discuss with the patient the individual’s goals for care, including desired quality of life, and seek to clarify misunderstandings. Include the patient’s surrogate in the conversation, if possible, even when the patient retains decision-making capacity.
- Reassure the patient (and/or surrogate) that medically appropriate interventions, including appropriate symptom management, will be provided unless the patient declines particular interventions (or the surrogate does so on behalf of a patient who lacks capacity).
- Negotiate a mutually agreed-on plan of care consistent with the patient’s goals and with sound clinical judgment.
- Seek assistance from an ethics committee or other appropriate institutional resource if the patient (or surrogate) continues to request care that the physician judges not to be medically appropriate, respecting the patient’s right to appeal when review does not support the request.
- Seek to transfer care to another physician or another institution willing to provide the desired care in the rare event that disagreement cannot be resolved through available mechanisms, in keeping with ethics guidance. If transfer is not possible, the physician is under no ethical obligation to offer the intervention.” (11)
The above steps are not limited to physicians. While nurses cannot make ultimate treatment decisions for the patient, they can ensure that the patient and family understand what the physician has explained. Furthermore, the nurse can act as an advocate for the patient. This kind of advocacy ensures that the patient’s wishes are being respected and that the care they are receiving is ethical.
How to Prepare a Family for End of Life Care
When the dying process starts, it is important that the family members present understand what is happening. The following are common, physical signs of the end of life:
- Increased sleeping
- Loss of appetite
- Labored breathing
- Decreased urine output
- Confusion
- Hallucinations
- Decreased heart rate
- Irregular breathing patterns (Cheyne Stokes respirations)
When you’re not a medical professional who has experienced the dying process with a patient, it can be jarring – especially when it’s your family member. Put yourself in the family members’ shoes and explain what is happening. Knowledge can be comforting for most but may not be in every case. Talk to the family members and assess how much they know and how much they would like to know. Be empathetic but do not dance around the subject. Use terms such as “die” instead of “pass away.” Using alternative terms for death and dying may leave it open to interpretation, and in some cases may give family members or patients false hope.
Family Support
Along with assessing the patient’s needs, the nurse should also frequently assess the needs of the family. Providing emotional support to the family member of a dying person is incredibly important, both during the dying process and afterwards (12). Be sure to involve social work if you identify any potential need for continued support for the family, i.e., support groups, social assistance, etc.
Conclusion
Nurses are an integral part of the end of life process, both in the planning and active phases. Among the biggest responsibilities for the nurse during this challenging time is the assessment of understanding of the treatment plan and goals, as well as ensuring that the patient’s autonomy and dignity are always respected. The healthcare team should work together as a whole to ensure that the dying process is as comfortable as possible for the patient and their family.
Alzheimer’s Nursing Care
Introduction
Alzheimer’s disease is a destructive, progressive, and irreversible brain disorder that slowly destroys memory and thinking. Alzheimer’s is the most common cause of dementia in older adults (1). For most people who have Alzheimer’s disease, symptoms first appear in their mid 60’s (1). Studies suggest more than 5.5 million Americans, most 65 or older, may have dementia caused by Alzheimer’s (1). It is currently listed as the sixth leading cause of death in the United States. It is important to understand the signs and symptoms of Alzheimer’s dementia and how to manage the care of a patient, family member, or friend suffering from the disease.
Dementia is the loss of cognitive functioning-thinking, remembering, and reasoning- and behavioral abilities to such extent that it interferes with activities of daily living (1). The severity of dementia ranges from mild to severe. In its mildest stage, it begins with forgetfulness, with its most severe stage consists of complete dependence on others for general activities of daily living (1).
History of Alzheimer’s
Alzheimer’s disease is named after Dr. Alois Alzheimer. In the early 1900’s, Dr. Alzheimer noticed changes in the brain tissue of a patient who had died of an unknown mental illness. The patient’s symptoms included memory loss, language problems, and unpredictable behavior. After her death, her brain was examined, and was noted to have abnormal clumps known as amyloid plaques and tangled bundled fibers, known as neurofibrillary or tau tangles (1). These plaques and tangles within the brain are considered some of the main features of Alzheimer’s disease. Another feature includes connections of neurons in the brain. Neurons are responsible for the transmissions of messages between different parts of the brain and from the brain to other parts of the body (1).
Scientists are continuing to study the complex brain changes involved with the disease of Alzheimer’s. It seems that the changes in the brain could begin ten years or more before cognitive problems start to surface. During this stage of the disease, the people affected seem to be symptom-free; however, toxin changes occur within the brain (1). Initial damage in the brain occurs within the hippocampus and entorhinal cortex, which are the parts of the brain that are necessary in memory formation. As the disease progresses, additional aspects of the brain become affected, and overall brain tissue shrinks significantly (1).
Signs, Symptoms, & Diagnosis
Memory problems are typically among the first signs of cognitive impairment related to Alzheimer’s disease. Some people with memory problems have a condition called Mild Cognitive Impairment (MCI) (4). In this condition, people have more memory problems than usual for their age; however, their symptoms do not interfere with their daily lives. Older people with MCI are at increased risk of developing Alzheimer’s disease. The first symptoms of Alzheimer’s may vary from person to person. Many people display a decline in non-memory related aspects of cognition such as word-finding, visual issues, impaired judgment, or reasoning (4).
Providers use several methods and tools to determine the diagnosis of Alzheimer’s Dementia. To diagnose, they may conduct tests of memory, problem-solving, attention, counting, and language. They may perform brain scans, including CVT. MRI or PET to rule out other causes for symptoms. Various tests may be repeated to give doctors information about how memory and cognitive functions change over time. They can help diagnose other causes of memory problems such as stroke, tumor, Parkinson’s disease, and vascular dementia. Alzheimer’s disease can be diagnosed only after death by linking clinical measures with an examination of brain tissue in an autopsy (4).

Self Quiz
Ask yourself...
- Have you experienced a patient in your practice with dementia or Alzheimer’s disease? What did their symptoms look like?
- What are some common diagnostic tools that healthcare providers use in the diagnosis of this disease?
- What is the definitive diagnosis of Alzheimer’s disease?
Stages of Disease
Mild Alzheimer’s
As the disease progresses, people experience significant memory loss along with other cognitive problems. Most people are diagnosed in this stage (1).
- Wandering/getting lost
- Trouble handling money or paying bills
- Repeating questions
- Taking longer to complete basic daily tasks
- Personality/behavioral changes (1)
Moderate Alzheimer’s
In this stage, damage occurs in the area of the brain that controls language, reasoning, sensor processing, and conscious thought (1).
- Memory and confusion worsen
- Problems recognizing family and friends
- Unable to learn new things
- Trouble with multi-step tasks such as getting dressed
- Trouble coping with situations
- Hallucinations/delusions/paranoia (1)
Severe Alzheimer’s
- Plaques and tangles spread throughout the brain and brain tissue shrinks by a significant amount
- Cannot communicate
- Completely dependent on others for care
- Bedridden – most often as the body shuts down

Self Quiz
Ask yourself...
- What are some of the signs and symptoms that differentiate each stage of Alzheimer’s disease?
- A person is in what stage of Alzheimer’s disease when they struggle recognizing family members and friends?
Prevention
As a person ages, many worry about developing Alzheimer’s disease and dementia. Especially if they have had a family member who suffered from the disease, they may worry about genetic risk. Although there have been many studies on the prevention of the disease, and many are still ongoing, nothing has been proven to prevent or delay dementia caused by Alzheimer’s disease (2).
A review led by experts from the National Academies of Sciences, Engineering, and Medicine, found encouraging yet inconclusive evidence for three types of interventions related to ways to prevent or delay Alzheimer’s Dementia or age-related cognitive decline (2):
- Increased physical activity
- Blood pressure control
- Cognitive training
Treatment of the Disease
Alzheimer’s disease is complex and is continuously being studied. Current treatment approaches focus on helping people maintain their mental function, manage behavioral symptoms, and low the symptoms of the disease. The FDA has approved several prescription drugs to treat those diagnosed with Alzheimer’s (3). Treating symptoms of Alzheimer’s can provide patients diagnosed with comfort, dignity, and independence for a greater amount of time, simultaneously assisting their caregivers. The approved medications are most beneficial in the early or middle stages of the disease (3).
Cholinesterase inhibitors are prescribed for mild to moderate Alzheimer’s disease; they may help to reduce symptoms. Medications include Rzadyne®, Exelon ®, and Aricept ® (3). Scientists do not fully understand how cholinesterase inhibitors work to treat the disease; however, research indicates that they prevent acetylcholine breakdown. Acetylcholine is a brain chemical believed to help memory and thinking (3).
For those suffering from moderate to severe Alzheimer’s disease, a medication known as Namenda®, which is an N-methyl D-asparate (NMDA) antagonist, is prescribed. This drug helps to decrease symptoms, allowing some people to maintain certain essential daily functions slightly longer than they would without medication (3). For example, this medication could help a person in the later stage of the disease maintain their ability to use the bathroom independently for several more months, benefiting the patient and the caregiver (3). This drug works by regulating glutamate, which is an important chemical in the brain. When it is produced in large amounts, glutamate may lead to brain cell death. Because NMDA antagonists work differently from cholinesterase inhibitors, these rugs can be prescribed in combination (3).

Self Quiz
Ask yourself...
- Is there a cure for this disease?
- What are some of the treatment forms that have been used for the management of Alzheimer’s disease?
- Can medications be used in conjunction with one another for the treatment of the disease?
Medications to be Used with Caution
Some medications such as sleep aids, anxiety medications, anticonvulsants, and antipsychotics should only be taken by a patient diagnosed with Alzheimer’s after the prescriber has explained the risk and side-effects of the medications (3).
Sleep aids
Used to help people get to sleep and stay asleep. People with Alzheimer’s should not take these drugs regularly because they could make the person more confused and at a higher risk for falls.
Anti-anxiety
Used to treat agitation and can cause sleepiness, dizziness, falls, and confusion (3).
Antipsychotics
Used to treat paranoia, hallucinations, agitation, and aggression. Side effects can include the risk of death in older people with dementia. They would only be given when the provider agrees the symptoms are severe enough to justify the risk (3).
Caregiving
Coping with Agitation and Aggression
People with Alzheimer’s disease may become agitated or aggressive as the disease progresses. Agitation causes restlessness and causes someone to be unable to settle down. It may also cause pacing, sleeplessness, or aggression (5). As a caregiver, it is important to remember that agitation and aggression are usually happening for reasons such as pain, depression, stress, lack of sleep, constipation, soiled underwear, a sudden change in routine, loneliness, and the interaction of medications (5). Look for the signs of aggression and agitation. It is helpful to be able to prevent the problems before they happen.
Ways to cope with agitation and aggression (5):
- Reassure the person. Speak calmly. Listen to concerns and frustrations.
- Allow the person to keep as much control as possible.
- Build in quiet times along with activities.
- Keep a routine.
- Try gently touching, soothing music, reading, or walks.
- Reduce noise and clutter.
- Distract with snacks, objects, or activities.
Common Medical Problems
In addition to the symptoms of Alzheimer’s disease, a person with Alzheimer’s may have other medical problems over time. These problems can cause confusion and behavior changes. The person may be unable to communicate with you as to what is wrong. As a caregiver, it is important to watch for various signs of illness and know when to seek medical attention for the person being cared for.
Fever
Fever could be a sign of potential infection, dehydration, heatstroke, or constipation (4).
Flu and Pneumonia
These are easily transmissible. Patients 65 years or older should get the flu and Pneumonia shot each year. Flu and Pneumonia may cause fever, chills, aches, vomiting, coughing, or trouble breathing (4).
Falls
As the disease progresses, the person may have trouble with balance and ambulation. They may also have changes in depth perception. To reduce the chance of falls, clean up clutter, remove throw rugs use armchairs, and use good lighting inside (4).
Dehydration
It is important to remember to ensure the person gets enough fluid. Signs of dehydration include dry mouth, dizziness, hallucinations, and rapid heart rate (4).
Wandering
Many people with Alzheimer’s disease wander away from their homes or caregiver. As the caregiver, it is important to know how to limit wandering and prevent the person from becoming lost (5).
Steps to follow before a person wanders (5)
- Make sure the person carries a form of ID or wears a medical bracelet.
- Consider enrolling the person in the Medic Alert® + Alzheimer’s Association Safe Return Program®
- Alert neighbors and local police that the person tends to wander and ask them to alert you immediately if they are seen alone.
- Place labels on garments to aid in identification.
Tips to Prevent Wandering (5)
- Keep doors locked. Consider a key or deadbolt.
- Use loosely fitting doorknob covers or safety devices.
- Place STOP, DO NOT ENTER, or CLOSED signs on doors.
- Divert the attention of the person away from using the door.
- Install a door chime that will alert when the door is opened.
- Keep shoes, keys, suitcases, coats, and hats out of sight.
- Do not leave a person who has a history of wandering unattended.

Self Quiz
Ask yourself...
- What are basic implementations you can make as a caregiver to make handling confusion and aggression easier in a patient with Alzheimer’s?
- What are some of the types of medical problems that people with Alzheimer’s may face and how can they be monitored for prevention?
Conclusion
Alzheimer’s is a sad, debilitating, progressive disease that robs patients of their life and dignity. As research continues on the causes, treatment, and prevention of the disease, it is important for healthcare workers and caregivers to know the signs and symptoms of a patient with Alzheimer’s disease and potential coping mechanisms and management strategies of the disease. More information on the disease is available through several various resources, including:
Family Caregiver Alliance
800-445-8106
NIA Alzheimer’s and related Dementias Education and Referral Center
800-438-4380
Nursing Care for Pediatric Patients by Stage of Development
Overview
Pediatric nurses carry a heavy responsibility for caring not only for this vulnerable, highly diversified population with complicated and intermingled medical needs but also understanding the importance of their emotional needs. Their emotional needs must become the top priority.
As nurses we are tasked with advocating and providing for the best interests of this sometimes-fragile population. We accomplish this by decreasing the stress and fear reactions that might occur if we do not strategize before we provide care to a child.
Although regression is expected with hospitalized children of all ages, it is the nurse’s responsibility to foster growth and acclimation within the healthcare setting. Children have stated that their worst fears during hospitalization are those related to nursing interventions such as needle sticks during IV insertion or injections (1).
As a former special education school nurse consultant for the emotionally impaired population, I cannot stress the significance of recognizing children’s emotional needs. If we take the time to address these needs prior to any hands-on procedure or even touching the child not only will our job be easier but also, we will have respected the child’s personal space thereby earning his/her trust.
This course will address many aspects of developmentally appropriate interventions with the pediatric population in a layout that is easy to comprehend and utilize in your practice. Children are resilient but we must give them a sense of control to build trust with healthcare providers.
The primary guiding principles are to involve families in their care as the basis of creating a solid relationship with the child and facilitating success in their treatment. The secondary guiding principle with children is we must help them become aware of what they feel before we ask them to control their behavior (2). Some children may not be equipped to express their feelings depending on their age.
They may not have the vocabulary to express those fears, anxieties, anger, happiness, and other feelings. We must guide them to express these feelings if not with words, then with activities, otherwise those feelings are likely to result in negative behavior. This course will give you up-to-date ideas, suggestions, and activities to improve your care to your pediatric population.
Current Practice
According to the Center for Disease Control (CDC), in 2017 hospitalized pediatric patients in the United States comprised 6.6% of the total hospitalized patients across all ages with a total of 73,529 pediatric patients (3). Those pediatric patients admitted are complex with comorbidities in many cases.
Currently nurses face increased patient caseloads in the hospital, homecare, and clinic settings and consequently their time is at a premium. The suggestions for interventions in this course will assist the nurse to provide care that is timely and diminish emotional meltdowns by understanding the child throughout his/her developmental stage.
The way a nurse approaches his/her patients can do a great deal in encouraging a frightened or wary child. Research has shown children tend to be extremely resilient when well supported (2). Children who have access to protective factors are better able to overcome adversity and traumatic events.
These protective factors are personal qualities such as personality; family connections; coping skills; feelings of control and self-confidence (4). Through adversity children can learn how to process life based on their own experiences, how they have dealt with those experiences in the past, and responses from others such as parents, nurses, and other healthcare providers. In short, children use these events to reflect back in a positive way for future stressful experiences.
A pediatric nurse deals not only with the child but also with all the anxieties and demands of the parents. In addition, a study by Tubbs-Cooley et al. (2019) found the intense intellectual pressures and time constraints of nurses are factors in the quality of care as much as patient volume and acuity.
Nurses experience intense stress to complete their vital tasks with patients and this is another factor in their abilities to deliver quality care. Hospital administrators, nurse managers and nurses themselves must address this level of stress and the time constraints to help facilitate quality of care. Children are equipped with abilities to detect hidden stress, and this reflects on how they perceive and react to a given situation.
Family Responses to Illness and/or the Hospitalized Child
It is the nurses’ responsibility to promote a sense of security in pediatric patients. In fact, it is the most important item on our to-do list in the healthcare environment of pediatric patients. Feeling secure depends on a sense of physical and psychological safety.
Parents are the most vital key to promoting this safety in the pediatric patient. Parent’s presence at the bedside is the best way to decrease anxiety and increase this sense of security in children. Nurses must do everything in their power to decrease parental stress and anxiety and that will directly impact the child’s positive coping abilities.
In order to help families adapt to the hospitalization of the child the nurse should:
- Build trust with the family by communicating frequently with them including siblings. This includes education in simple, concrete facts that encourages parents to ask questions. The nurse should ask questions that are open ended to the child, parents, and siblings.
- Understand that parent’s presence in their child’s hospitalization is an extension of the child in order for the child to make sense of what is happening to him/her.
- Encourage parents to stay in touch with siblings at home if parents are staying at the hospital.
- Establish a relationship with the sibling and explain the medical condition of his/her sibling in simple terms. Also, include the sibling in therapy with the patient so the sibling feels he/she is helping his/her sick sibling.
- Instill a sense of hope in parents by carefully choosing words that elicit hope.
- Focus on the positives in every situation.
- Encourage parents to visit their child anytime, stay overnight, and/or call the nurse for an update. Nurses need to assess how much parents would like to be involved and support their choice. The primary goal should be no separation of parent and child in children under 5 years of age (6).
- Identify key family members and decision makers in the child’s care.
- Teach parents how to talk to their child about the medical procedures, equipment, status, and health concerns. Prepare parents ahead of time for tough conversations with children to lessen both the parent’s and the child’s anxiety level.
- Teach parents how to talk calmly, how to touch to calm the child, and the power of eye contact during procedures (7). Parents have a key role in lessening anxiety through coping skills. Children can sense parent’s emotional upheaval so working to lessen parent’s emotionality is crucial to helping children cope.
- Parents and nurses need to respond to an anxious child with empathy, compassion, and acknowledgement.
Here are some examples of therapeutic communication with a child:
| Avoid Saying: | Say Instead: |
| “Don’t worry.” | “Can you tell me more about your worries?” |
| “It’s no big deal.” | “I can see why you are feeling anxious, let’s think of something positive.” |
| “You’ll be fine.” | “I am here for you.” |
| “There’s nothing to be afraid of.” | “Let’s talk about this.” |
| “You just need to sleep more.” | “Let’s mediate together.” |
| “I’ll do it.” | “I know you are anxious right now, but I am here for you and know you can do it.” |
| “It’s all in your head.” | “Let’s talk about what’s worrying you while taking a walk.” |
| “This will only take a few minutes.” | “This will be really quick.” |
“I need to give you a shot.” (Children sometimes think shot means being shot with a gun.) | “I need to give you some medicine.” |
“I’m going to take your temperature.” (Young children may think you are going to take something from them.) | “I want to find out how warm you are.” |
Adapted from Hurley (2018) and Fastaff (2015)

Self Quiz
Ask yourself...
- Think about your interactions with pediatric patients. Could you re-phrase your conversations to be more developmentally appropriate? If so, how?
- How can nurses help patients and families adapt to acute illness and hospitalizations?
Developmental Considerations for Appropriate Nursing Interventions
Children face a loss of control, limits on their mobility, powerlessness, pain, and discomfort, to name a few emotions and negative consequences occurring while ill. It is the nurse’s responsibility to help children cope with medical procedures and their illness. The best way to facilitate this is through an atmosphere of trust. Trust is best created and fostered through strategies that are researched to be effective.
There are strategies that occur across developmental stages, and these will be addressed first before discussing specific strategies based on the developmental age groups. These age groups will be divided into infant, toddler, preschool, school age, and adolescence in this course. These groups will be explored below for the best nursing interventions using evidence-based practice. Therapeutic play will be addressed in the section following this one.
General Interventions across the Developmental Spectrum
There are some interventions and principles that hold true for children of all ages. Pediatric nurses should strive to incorporate these principles into their practice regardless of the age of the developmental stage of the child.
- Children grasp information best when it is appropriate to their cognitive level of development.
- Offer choices to every child when performing even routine tasks such as obtaining his/her blood pressure. This will promote a sense of control in the child. Asking “what arm would you like me to use to check your blood pressure?”
- Create a daily schedule so that the child is aware of what to expect throughout his/her day.
- Use humor and laughter to lighten up the air with children.
- Use time-out coupons, for example three per procedure that the child can use to halt the procedure for 2 minutes (9). This gives control to the child to better cope with the procedure.
- A pre-surgical tour of the hospital can lessen anxiety and promote cooperation.
Children need a regular schedule in the hospital that mirrors home life as much as possible, but that is also consistent from day to day in the hospital setting. Research has shown that without a regular schedule for children of all ages, a child can feel confused and insecure adding to emotional upheaval, stress, and adaptability (9).
- Nurses should stoop down to the child’s level physically. Eye to eye contact is important to develop a trusting relationship. The use of a short stool works well to get at their eye level.
- Introduce yourself and ask the child personal questions such as “What is your favorite toy?” or “Who is your favorite cartoon character?”
- Nurses should smile at their pediatric patients. Children of all ages appreciate this approach from babies to adolescents. Who doesn’t like a friendly, calm approach?
- Regardless of the age of the child, use his/her name. It soothes children and parents alike. It shows respect for individuality and lessens anxiety in children and parents. Never refer to a child by his/her diagnosis.
Children of all ages from toddlers through adolescence love to help. Through their role in their own care, it can alleviate stress and build trust. For example, you could ask the child to hold your otoscope until you need it. Teach them the tools of the trade. At the same time, you are educating about a possible career choice for one of them.
- Say simply, “I need your help to stay very still. Can you do that?” This activates the child to engage in your activity with helpfulness.
- Consider using a therapeutic dog in the hospital setting as a distraction and calming technique when appropriate (9). Animal assisted therapy has shown to improve the level of anxiety in parents and children. Check with your facility for approval of canine therapy. Or get permission for the child’s dog to visit in the playroom.
- Give children the same time and respect you would give to adult patients (10). This includes decision-making even when they are not able to make decisions on their own. This will enhance their sense of control over their own health.
- Secrecy and dishonesty increase a child’s sense of anxiety and fear and undermines trust with the nurse (10).
- Nurses should coach children to ask more questions and thereby increase satisfaction with their healthcare providers and more compliance with their disease processes (10).
- Never talk down to a child for example in a singsong voice. This is demeaning to him/her.
- Encourage parents to bring in posters, photographs, and other items from home to personalize the bedside. This may help the child to feel more comfortable in the hospital setting.
- Choose roommates for children, if possible, to promote socialization and foster growth in children. Sometimes nurses can advocate for children with similar disease processes or hobbies to room together in the hospital. This promotes a sense of community facilitating recovery and belonging.
- Remind children that their illness is not punishment. Explore this confusion in your pediatric patients. Sometimes children do not have the words to express their fears that they did something wrong to cause their illness or hospitalization.
- Use words and sentence length that matches the child’s level of understanding. A common way to measure this is the number of words in a child’s sentence should equal his/her age plus one (6).
- Use crayons and paper freely. First demonstrate by drawing yourself and encourage child’s expression.
- Give children time to feel comfortable with you. Speak to the parents first.
- Help children understand they can face their fears. Promote courage by stating, “I know you’re scared and I’m here to help you.”
- Give hope and courage to children through praise by stating how “brave” and/or “good” they are.
- Communicate with puppets, dolls, or stuffed animals first before asking questions directly of a young child.
- If a child is ticklish when you are examining his/her abdomen, place the child’s hand down first on his own abdomen and place your hand on top of his. Then slowly deviate from his hand to examine the abdomen.
- Parents should not be asked to restrain their child. This interferes with the trust relationship the child has with his/her parent (6)
- Allow children to pick a toy out of the toy box to play with during the procedure and then afterwards they can pick a gift out of the box and return the toy.
- Involve the medical social worker to assist in therapy with pediatric patients.
- Tell children it is okay to cry, do not shame them for expressing this emotion.
- Stress the positive benefits of procedures for example, “After this bandage change your sore will heal quicker.”

Self Quiz
Ask yourself...
- What are some themes you notice about the general interventions?
- Think about an experience you had with a pediatric patient that did not go well.
- Could any of these interventions have helped you improve the interaction? If so, how?
The Importance of Caring, Consistency, and Humility
Children of all ages must feel a sense of love from their caregivers. Children are barometers of emotions in those people surrounding them. These emotions can influence negative behavior in hospitalized children. This is a basic tenet but vitally important to working effectively and compassionately with the pediatric population. Children are more likely to push past anxiety and have a sense of safety if surrounded by genuine caring from nurses. Love can best be demonstrated in those quiet moments shared with children, holding, stroking their arm, and/or sharing some fun activity. Children are naturally resilient but need basic emotions of love and trust to foster this resiliency. Sometimes one successful episode is all a child needs to feel that they can complete a procedure or tackle the impossible.
How do we show kindness, yet firmness? How do we show empathy and respect? These personality traits flow from our inner core but can be learned. Humility allows us to offer choices both to parents and children. We MUST keep this in mind when working with the pediatric population because this will give both parents and children a sense of control. Many negative emotions in a child flow from a loss of a sense of control.
When working with children, this author was always very clear to the child about her expectation that the child would only be able to stay in the health room for 15 minutes, but he/she could choose whatever activity would help him/her regroup and get back to the classroom. The following strategies were offered: a short nap, reading a short book to the child, a small snack, hot compress, cold compress, or relaxation exercises. The author was always successful with this approach because the child felt affirmed, respected, and in control which also created an atmosphere of trust.
Labeling Feelings
Helping children to understand their feelings and label them is an instrumental step in helping them to gain control of the situation and their emotions. Rachel Wagner in her book Flip It reiterates the root to all behavior is feelings (2). She states we must help them identify these feelings before we ask them to control them.
Using feeling charts, (see Appendix A) we can assist our patients to talk about what they are feeling by giving them the words for these emotions, such as anger, frustration, happiness, sadness, confusion, or disappointment, and others.
Then explaining that these feelings are usually temporary, normal, and it’s okay to feel them. Competency = less anxiety (2).
Let’s Talk About Resiliency
Nurses need to assess a family’s resilience that is described as the family’s ability to handle stress and challenges (12). Nurses can help families learn new skills and reinforce confidence in family members to deal with the stress of illness or injury in the child. Sources of support to build resilience in the family are church, family coping mechanisms, flexibility, and social support (12). Nurses can help families see their strengths and transfer competence from their past stresses in life to this event.
There are strategies to strengthen resiliency in children and by doing so children are less anxious, better behaved, and more in control. An important key reminder about resiliency is that we are not born with it, we develop it over time with each success, each positive opportunity, and even small words can grow it. Children do not need parents (or nurses) to solve their problems. Resiliency is enhanced when children solve their own problems. Children need to experience discomfort to learn that they are capable of adapting, learning, and solving. This builds competence. (12)
How do you build resiliency in kids? According to Katie Hurley (12), nurses should:
- Resist fixing problems and instead ask the child how they would fix that problem. Give control back to the child, showing the nurse believes in the child’s problem-solving abilities.
- Encourage deep breathing to give children something to do to regain control of their emotions.
- Embrace mistakes as missteps instead of total failures. Teach that mistakes are a learning process and that nothing ventured is nothing gained. We must encourage children to be adventure takers. We must accentuate the positive instead of the negative. We know that resiliency and optimism go hand in hand.
- Find a way for the child to get fresh air outside or engage in a physical activity if possible. (12)
Developmental Strategies with Infants (0-12 months)
We must remember that infants are learning to develop trust in their first year of life. They use all their senses to develop this trust, such as vision, hearing, taste, smell, and touch.
To care for infants in the healthcare setting the nurse should (11):
- Swaddle, hold, pat and provide other gentle physical contacts with infants.
- Use a soft voice and calm approach. Sudden, loud movements frighten them.
- Sing songs or play music to soothe infants.
- Distract the infant during procedures with a rattle or eye-catching object.
- Care for the same infant day after day to promote consistency and decrease the likelihood of stranger anxiety that is common in infants from 6 to 18 months. They are more at ease with a consistent caregiver (9).
- Examine children who are in the stranger anxiety stage by placing them on their parent’s lap and sit opposite to examine them.
- Provide a favorite toy or blanket to establish trust and consistency in the hospital setting. Infants enjoy peek-a-boo around 9 months of age.
- Offer the infant a pacifier, bottle or have mother breastfeed after a painful procedure.
- Reduce excessive stimuli and promote a quiet environment.
- Provide non-nutritive sucking with sucrose during the procedure since this has shown to calm infants (6).

Self Quiz
Ask yourself...
- How can you incorporate the interventions above into your practice when caring for infant patients?
- Which specific interventions have you previously noted to be effective?
Developmental Strategies with Toddlers (1-3 years)
Toddlers are learning much about their environment through exploration and trying to make good choices. Slowly they are learning self-control (9).
To care for toddlers in the healthcare setting the nurse should (9):
- Allow the toddler to sit on the parent’s lap during the procedure or exam.
- Give the toddler a choice such as “Would you like me to listen to your heart first or look at your ears?”
- Refrain from asking the toddler permission to examine him/her because the answer is likely going to be no. Instead, state calmly and firmly what area you are examining next.
- Use distraction such as the parent blowing bubbles or reading to the child during the procedure.
- Prepare the toddler no more than one day ahead of time for the procedure otherwise it can increase anxiety at this age level.
- Ask the child to point to a body part that you are going to examine.
- Show the child the equipment you will use.
- Praise the child using his/her first name for cooperating.
- Allow the toddler to dress self, use potty-chair, and self-feed.
- Name objects with simple explanations.
- Perform treatments in a separate room rather than toddler’s bedroom so his/her bed is a safe haven.
- Allow the toddler to choose a sticker after the procedure.
- Provide a nightlight in the child’s room.
- Give the toddler a choice by saying, “Once I have listened to your heart, you can choose to ride in the cart or walk to the playroom” to decrease resistance from the child.
- Comfort the toddler after a painful procedure by rocking, singing, offering a snack, or holding him/her.

Self Quiz
Ask yourself...
- How can you incorporate the interventions above into your practice when caring for toddler-aged patients?
- Which specific interventions have you previously noted to be effective?
Developmental Strategies with Preschool Children (3-6 years)
Preschoolers have a very active imagination and are very concrete in their thinking. They see everything from their own point of view.
To care for preschoolers in the healthcare setting the nurse should:
- Allow the child to touch or play with equipment you will use.
- Have the preschooler sit on the parent’s lap.
- Give the child choices in your approach to him/her.
- Make up a story about what you are examining or doing such as, “I’m seeing how strong your muscles are” when checking his/her blood pressure (6).
- Use drawings to help explain procedures and allow the child to draw both before and after the procedure to process the information.
- Expect cooperation by using positive statements such as, “Open your mouth.”
- Read books to the child to help him/her process what is happening.
- Use the doll or stuffed animal to practice what is happening to him/her.
- Be alert to the comfort level of the child with male or female nurses and try to accommodate the child if possible.

Self Quiz
Ask yourself...
- How can you incorporate the interventions above into your practice when caring for preschool-aged patients?
- Which specific interventions have you previously noted to be effective?
Developmental Strategies with School Age Children (6-12 years)
School age children want explanations for everything and are usually satisfied with this approach. They want to examine and understand how the equipment works. They have lots of ‘why’ questions. They have a heightened concern about their body and anything that might mean injury or pain to their body. This concern extends to their possessions (6).
To care for school age children in the healthcare setting the nurse should:
- Answer all their questions and demonstrate the equipment. Your patience with this age group will usually pay off.
- Allow the child to express his/her concerns and provide reassurance.
- Focus on positive behaviors and reinforce these behaviors.
- Encourage the child to resume schoolwork as quickly as feasible.
- Be alert to manipulation by the child to avoid a treatment or procedure. Sometimes this age group is prone to bargaining to delay procedures, so the nurse should be flexible but aware of this possible occurrence.
- Knock on the door before entering the room.
- Encourage the child’s friends to visit or call the patient.
- Allow the child to choose his/her reward after the procedure.
- Teach techniques like counting, breathing or visualization to manage difficult situations.
- Use small talk as a means of distraction during the procedure.

Self Quiz
Ask yourself...
- How can you incorporate the interventions above into your practice when caring for school age patients?
- Which specific interventions have you previously noted to be effective?
Developmental Strategies with Adolescent Children (12-18 years)
This age group fluctuates between child and adult thinking and behavior (6).
To care for adolescent children in the healthcare setting the nurse should:
- Allow for regressive behavior and expect it.
- Respect their need for privacy.
- Encourage socialization with peers from within and outside the hospital.
- Allow wearing of street clothes in the hospital setting, if possible
- Allow the child to use electronic equipment such as cell phone, I-pad, and/or computer.
- Offer written and verbal complete explanations of the disease and necessary procedures.
- Introduce the teen to other teens with the same health problem.
- Be sure snacks are available since this group tends to require more calories throughout the day.
- Be alert to manipulation by the child to avoid a treatment or procedure. Sometimes this age group is prone to bargaining to delay procedures, so the nurse should be flexible but aware of this possible occurrence.
- Promote competence and independence in the child and should not focus on the negative. The nurse must build up the child’s spirit.
- Encourage the child to express his/her feelings about his/her experiences in the healthcare setting.

Self Quiz
Ask yourself...
- How can you incorporate the interventions above into your practice when caring for Adolescent patients?
- Which specific interventions have you previously noted to be effective?
Use of Play – Therapeutic Play
Children use play to make sense of their world, to categorize the collective whole of their being with their interactions, dreams, missteps, and joyful attitudes. As nurses, we must facilitate this play through our contact with our youngest patients. Play is very individualized, each child deciding his/her favorite play activity. Therapeutic play decreases negativity, provides motor activity outlet, and helps the child cope. Play provides the child with an active role and control of the situation and distracts from procedures that cause stress (1).
Here are some examples of therapeutic play:
- The child using the IV catheter on his/her doll or stuffed animal. Allowing the child to play with the equipment for several days prior to the procedure assists in processing the procedure successfully.
- Stories can be read to the child, or the child can make up his/her own story about the healthcare event.
- Puppets are especially useful for children to act out what they are experiencing in the hospital setting. Nurses can also have the puppets ask personal questions of the child, and it is more likely the child will answer them.
Expressive therapy (13) works well with children oftentimes because they are hands-on learners and express their emotions the same way. Here are some examples of expressive therapies that can help children address fear, anxiety, stress, and pain:
- Art therapy
- Drama therapy
- Play therapy
- Music therapy
- Poetry therapy
- Sand play therapy
Specific Play Activities for Specific Procedures (6):
- Increasing fluid intake can be accomplished by cutting gelatin into fun shapes; using small medicine cups and decorating them; color water with food coloring; make a poster and give rewards when drinking a prescribed amount.
- Deep breathing can be encouraged through blowing bubbles; blowing a pinwheel or a party blower; suck paper from one container to another using a straw.
- Range of motion activities can be simulated with activities such as:
- throwing bean bags into a basket
- hanging balloons and having the child kick them
- playing Twister or Simon Says
- playing kickball with a foam ball
- providing clay for fine motor exercises
- painting or drawing on large sheets of paper on the floor
- playing beauty shop to comb or set hair
- Soaks can be imitated by playing with toys in water; washing his/her dolls; picking up marbles in the bath water.
- Injections can be simulated by letting the child play with the syringes with his/her doll; use syringes to decorate cookies with frosting; allow the child to have a collection of different sized syringes to manipulate.
- Giving the child something to push like a stroller or wheelchair and holding a parade can encourage ambulation.
- Children in traction can have their environment expanded by turning the bed into a pirate ship or airplane with decorations; or moving the bed to the playroom.

Self Quiz
Ask yourself...
- Therapeutic play can be a powerful tool for building trust with pediatric patients.
- Have you witnessed a caregiver utilizing therapeutic play? If so, what was your experience?
- How can you incorporate therapeutic play into your practice?
Cultural Considerations
It is imperative that nurses consider the cultural influences of the children they care for in the healthcare setting. Cultural competence includes understanding the values, beliefs, and customs of ethnic groups and how these influence health decisions by that family. All behavior must be judged based on the context of the culture in which it occurs (6). Sometimes children of a minority do not trust that nurses of a majority culture respect them or understand them. This can cause fear and stress in that child and contribute to loneliness and helplessness.
Here are some useful tips to facilitate appropriate interventions (6):
- Ask open-ended questions about cultural needs and health habits.
- Facilitate communication with an interpreter or language line telephone.
- Some ethnic cultures see eye-to-eye contact as aggressive and rude.
- Although ethnic generalizations are known, there are great variations among individuals regarding how they practice within that culture.
- Culture can influence a child’s self-esteem.
- In non-English speaking patients, pain may not get reported because some ethnic people believe that pain means the disease has worsened (2).
Reducing Pain and Discomfort
Any measures to reduce pain and discomfort are the nurse’s responsibility. Nurses must assess both parents and the child for the level of security, fear, and resistance to the procedure. In addition, differentiating between fear and pain is vital to the correct approach by the nurse (1).
Nurses must support children through parental participation and communication (1). Untreated pain in infants and young children may lead to increased pain perception and chronic pain in adolescents and adults (14).
Pain research has found that children who show more active behavior during the procedure such as crying and flailing oftentimes rate these procedures as less painful than children who cope passively (7).
For this reason, we want to always encourage children and parents that it is normal to cry when something is painful. Children should never be shamed or made to feel guilty for crying or screaming.
In order to lessen pain and discomfort the nurse should:
- Include parents in pain control techniques and teach them their role in pain control for their child. Parents are the most important part of pain management. This role is very child-parent specific and includes coping styles of both the parents and the child (7).
- Consider using a device called “Buzzy” to decrease the sensation of pain during IV insertion or venipuncture (15). This device uses a combination of cold and vibration to replace pain with movement and temperature. Research has shown this device to be effective in decreasing pain and discomfort during some procedures (15).
- Provide an outlet through serious gaming for these children. Serious gaming is defined as video games that require active participation by the child through problem solving that has shown to be highly effective as a distractor during painful procedures (16).
- Be open and honest to children in their care. It is better to say, “Sometimes this feels like pushing or pinching and sometimes it doesn’t bother people. You tell me how it feels” instead of, “This is probably going to hurt.” (7)
- Provide distraction for children to decrease their pain experience, examples include listening to the radio or music; the child singing, deep breathing, blowing bubbles to blow the pain away, yelling as loud or soft as it hurts, visiting with friends or watching TV (7).
- Teach relaxation techniques to the child and parents such as gently swaying a child, rocking, or having him/her take a deep breath then relaxing his/her body on exhalation.
- Teach guided imagery to children and parents, examples include asking the child to verbalize relaxing experiences, or have the child pre-tape his/her story of a relaxing event and listen to it during the painful procedure.
- Encourage positive self-talk with the child. For example, having the child say, “I’m going to feel better soon” or “I know I can do this.”
- Use topical anesthetics on any age child to decrease the pain sensation during IV insertion or venipuncture procedures.
In order to lessen pain and discomfort based on age specific strategies the nurse should (9):
Infants:
Encourage holding, cuddling, allowing infants to suck a pacifier, use of sucrose while sucking, and massaging.
Toddlers:
Encourage reading them stories, massages, blowing bubbles, touching, holding, rocking, listening to music, and coloring.
Preschoolers:
Encourage playing, reading stories, listening to music, child pretending to be a superhero, watching TV or a video, and engaging in arts/crafts.
School age children:
Encourage the child to breathe rhythmically, use guided imagery, talk about fun experiences, play games, listen to TV, radio, or music, and engage in arts/crafts.
Adolescents:
Encourage the child to breath rhythmically, use muscle relaxation, use guided imagery, listen to music, watch TV, have visitors, play games, and arts/crafts.

Self Quiz
Ask yourself...
- Painful experiences can be traumatic for pediatric patients.
- How can you use the above interventions in your practice to reduce the perceptions of pain?
Pediatric Patients with Special Healthcare Needs
As a former special education school health consultant for children in grades kindergarten through 12th grade, this author became proficient at reading students’ needs or discerning when she could not determine their needs and had to rely on other cues. This pediatric population encompasses many complex health issues that may be chronic and lifelong. Beneath all the tubes, devices, special needs equipment, there is a child who is like many children without special needs. They are longing to be seen, to be heard, and to be accepted as they are.
Some suggestions for nurses when interacting with this population are (17):
- To leave any labels at the door and interact with this population as individuals with distinct needs similar to the pediatric population at large.
- Even though a child may have a cognitive diagnosis he/she still shares dreams, hopes, and feelings. These children desire to be seen as individuals who relish conversations with people and interactions. Talk in a normal tone and give them eye contact.
- A child’s loud verbalization does not necessarily mean pain. Get to know these individuals on a personal level. Oftentimes this verbalization could be laughter. Trust in your own senses to determine the difference.
- Respect these children’s bodies regardless of ability. Explain to this child what you are doing before doing it.
- Even though a child with special needs might not interact or talk; provide care, respect, and compassion as you would any other patient.
- Provide comfort as you would any patient, even though these children express themselves differently. They need love, kindness, and patience.
- Show advocacy for each child you care for regardless of ability, diagnosis, or IQ. Involve special needs children in the conversation; even though they do not participate verbally, they understand what is happening.
- Use the checklist developed for non-communicating children to assess the pain level of these special needs children (see non-communicating children’s pain checklist at http://www.community-networks.ca/wp-content/uploads/2015/07/PainChklst_BreauNCCPC-R2004.pdf) (6).
- Treat each child with the special care and a patient approach that they so deserve and require.
- Communication is vital with the child and his/her family members.
- Nurses must not place judgments on patients but keep an open mind and an open heart to guide patients towards their best healthcare outcome.
- Nurses have expressed concern with having adequate time to care for the special needs pediatric patient in a holistic manner (18). Nurses desire to engage in a thorough way with these patients and their families but time constraints limit over-involvement and sometimes lead to frustration and guilt on the nurses’ part. They describe it as an art to balance the time factor with the multiple needs of these patients, and the other patients on the nurses’ caseload.
Summary
The pediatric population requires nurses who embrace the cohesive bond between parents and child. The nurse must work well with both to enhance the best care possible for the family. Advocacy takes on many forms as a pediatric nurse; the parent, the child, and the family unit must all be promoted and supported.
Nurses make the difference, and their care is multiplied through each patient and each hospitalization. Pediatric nurses through dedication and mutual problem solving with families show responsiveness to children’s experiences, age, and development to meet the child in his/her world.
Opioid Abuse
What are Opiates?
Opiates are powerful substances which are commonly used to alleviate both acute and chronic pain. The history of opiate use / abuse goes back many thousands of years. The first recorded reference is from 3,400 B.C. when opium was cultivated in southwest Asia. There were even wars fought over the previous flow in the mid 1800s (1). The most famous historical event related to opium were the advent of “opium dens.” These were underground “dens” where opium was bought, sold, and used (1). Much like today, the addictive properties of opium overcame many individuals and caused great harm to the world and communities. Indeed, the opiate epidemic of the 2000’s is not the first in modern history, though it is much different and more severe than previous epidemics.
Today opiates are used for both acute and chronic pain. The ability to quickly, reliably, and (when used appropriately) safely reduce pain is what makes the drug class so valuable. Many common drugs are opiate derivatives or synthetics including morphine, codeine, oxycodone, heroin, hydromorphone, and fentanyl.
In the United States Opiates are considered controlled substances and most of them are classified as schedule II (with heroin classified as schedule I) (2). Opiates will always have a place in medicine and treatment of pain and are incredibly useful, however, the current opiate epidemic in America makes clear the potential consequences of opiate abuse.
Preventing Abuse, Misuse, and Harm
Every day 130 Americans die of opiate overdose (3). Additionally, there are 4.3 million Americans each month who engage in the non-medical (non-prescribed or illicit) use of opiates (5). However, it is key to remember that opiate-related deaths are not the only negative consequences. There are many overdoses which do not end in death, and on the other end of the spectrum many negative affects do not cause death. Addiction can cause loss of job, damage to relationships, psychologic distress, homelessness, and many more negative side-effects.
So how do healthcare professionals help reduce the impact of opiate addiction and misuse? The approach must be multi-modal, aimed at primary, secondary, and tertiary prevention.
- Primary prevention includes appropriate opiate prescribing, risk stratification with patients, and preventing opiate addiction.
- Secondary prevention is aimed at mitigating the effects of opiate addiction. This includes rehabilitation and cessation of opiates in addicted individuals, ideally in favor of non-opiate treatment options.
- Tertiary prevention is the reduction in harm from opiate addiction and overdose. This includes resuscitation of overdose patients and helping patients recover from the effects of opiate addiction.
Appropriate Prescribing
The Centers for Disease Control and Prevention (CDC) offers excellent guidance on how to appropriate prescribe opiates, though it will continue to require a great deal of knowledge and effort from individual prescribers and managers of chronic pain. For the purposes of this article, we will focus on the CDC recommendations. Below we will discuss the 12 key points of opiate management, per the CDC.
Opioids Are Not First-Line Therapy
“Nonpharmacologic therapy and nonopioid pharmacologic therapy are preferred for chronic pain. Clinicians should consider opioid therapy only if expected benefits for both pain and function are anticipated to outweigh risks to the patient. If opioids are used, they should be combined with nonpharmacologic therapy and nonopioid pharmacologic therapy, as appropriate.” (5)
Author’s Input
Many patients experience pain. Indeed, it is one of the most common complaints in primary care offices. When dealing with chronic pain, we should consider ALL non-opiate therapies for patients prior to prescribing opiates. This can include physical therapy, meditation, exercise / movement, treatment of underlying depression and/or psychiatric issues, meditation, modification of aggravating factors, and many more interventions. In some cases, none of these alone or combination will be enough to provide satisfactory relief, but we must utilize non-opiate and non-pharmacological solutions as much as possible to reduce opioid abuse, and dose (if opiates are necessary).
Establish Goals for Pain and Function
“Before starting opioid therapy for chronic pain, clinicians should establish treatment goals with all patients, including realistic goals for pain and function, and should consider how opioid therapy will be discontinued if benefits do not outweigh risks. Clinicians should continue opioid therapy only if there is clinically meaningful improvement in pain and function that outweighs risks to patient safety “(5).
Author’s Input
Many patients erroneously believe that cessation of pain is the goal of therapy. This is not based in fact nor is it reasonable, as many patients (even with opiate therapy) will not have complete remission of pain. The goal of the clinician should be to work with the patient to provide the minimal risk intervention that will provide acceptable pain control.
Discuss Risks and Benefits
“Before starting and periodically during opioid therapy, clinicians should discuss with patients known risks and realistic benefits of opioid therapy and patient and clinician responsibilities for managing therapy” (5).
Author’s Input
A prescription for an opiate should never be written to a patient without a through discussion of the risks and benefits. The clinician must first be convinced that the risk to benefit favors prescribing an opiate. Then, they must discuss their rationale with the patient. An individual assessment regarding the risks should be provided to each and every patient.
Prescribe Immediate-Release Opioids First
“When starting opioid therapy for chronic pain, clinicians should prescribe immediate-release opioids instead of extended-release/ long-acting (ER/LA) opioids” (5).
Author’s Input
Extended-release opioids have been associated with higher rates of overdose and higher potential for Opioid abuse. Immediate-release opioids should be utilized first, whenever possible.
Clinicians Should Prescribe the Lowest Effective Dosage
“Clinicians should use caution when prescribing opioids at any dosage, should carefully reassess evidence of individual benefits and risks when considering increasing dosage to ≥50 morphine milligram equivalents (MME)/day, and should avoid increasing dosage to ≥90 MME/day or carefully justify a decision to titrate dosage to ≥90 MME/day.”
Author’s Input
The clinician must keep in mind that the “minimum required dose” may change over time. As a patient implements more non-pharmacologic interventions the required dose may decrease. Conversely, there can be some degree of tachyphylaxis with opiates and the required dose may also increase. Dose titration requires careful clinician judgement.
Prescribe Short Durations for Acute Pain
“Long-term opioid use often begins with treatment of acute pain. When opioids are used for acute pain, clinicians should prescribe the lowest effective dose of immediate-release opioids and should prescribe no greater quantity than needed for the expected duration of pain severe enough to require opioids. Three days or less will often be sufficient; more than seven days will rarely be needed” (5).
Author’s Input
It is well established that chronic opioid therapy is not the most effective therapy for pain management. Clinicians should consider adjuncts for ongoing or chronic pain patients.
Evaluate Benefits and Harms Frequently
“Clinicians should evaluate benefits and harms with patients within 1 to 4 weeks of starting opioid therapy for chronic pain or of dose escalation. Clinicians should evaluate benefits and harms of continued therapy with patients every 3 months or more frequently. If benefits do not outweigh harms of continued opioid therapy, clinicians should optimize other therapies and work with patients to taper opioids to lower dosages or to taper and discontinue opioids” (5).
Author’s Input
It is important that clinicians consider changing circumstances. A patient’s health status or life circumstances may change such that opiate therapy benefits no longer outweigh the harm, or vice-versa.
Use Strategies to Mitigate Risk
“Before starting and periodically during continuation of opioid therapy, clinicians should evaluate risk factors for opioid-related harms. Clinicians should incorporate into the management plan strategies to mitigate risk, including considering offering naloxone when factors that increase risk for opioid overdose, such as history of overdose, history of substance use disorder, higher opioid dosages (≥50 MME/day)” (5).
Author’s Input
Naloxone therapy should be considered for all patients who are at high risk of Opioid overdose.
Review Prescription Drug Monitoring Program Data
“Clinicians should review the patient’s history of controlled substance prescriptions using state prescription drug monitoring program (PDMP) data to determine whether the patient is receiving opioid dosages or dangerous combinations that put him or her at high risk for overdose. Clinicians should review PDMP data when starting opioid therapy for chronic pain and periodically during opioid therapy for chronic pain, ranging from every prescription to every 3 months” (5).
Author’s Input
Each state has robust data regarding prescription medication; utilizing this data can help reduce opioid misappropriation and concurrent prescriptions (doctor shopping).
Use Urine Drug Testing
“When prescribing opioids for chronic pain, clinicians should use urine drug testing before starting opioid therapy and consider urine drug testing at least annually to assess for prescribed medications as well as other controlled prescription drugs and illicit drugs,” (5).
Author’s Input
The author recommends that clinicians take great care in this area. Indeed, drug testing can help identify those who are already abusing other substances, but it can also harm the trusting relationship developed between a patient and clinician. The patient should be re-assured that the testing is performed for their own good and out of concern for their own health, rather than punitively or because the clinician “mistrusts” them, as these may be the default thoughts of many patients.
Avoid Concurrent Opioid and Benzodiazepine Prescribing
“Clinicians should avoid prescribing opioid pain medication and benzodiazepines concurrently ‘whenever possible’ “(5).
Author’s Input
The highest risk of overdose of opioid abuse is commonly seen when opiates and benzodiazepine (or any combination of sedating medications) are prescribed concurrently, especially in conjunction with alcohol. For this reason, clinicians should strongly consider avoiding such risks and only prescribing this combination when absolutely necessary.
Offer Treatment for Opioid Abuse Disorder (OAD)
“Clinicians should offer or arrange evidence-based treatment (usually medication-assisted treatment with buprenorphine or methadone in combination with behavioral therapies) for patients with opioid abuse disorder” (5).
Author’s Input
In acute cares settings, clinicians often view OAD as a secondary illness and it is frequently left unaddressed. However, there are now effective treatments for OAD. Given the significant morbidity, mortality, and associated quality of life issues, patients with OAD should be offered treatment, even if it not the primary reason for treatment.
Risk Factors for Opiate Harm or Misuse
The risk to benefit has been discussed many times previously and is often referenced by the CDC. The benefits of opiate therapy are typically obvious (reduced pain, increased quality of life, etc.), but the risks are less often discussed. So how do nurses know who is at higher risk of the negative effects of opiates?
According to the CDC, the major risk factors are:
- Illegal drug use; prescription drug use for non-medical reasons.
- History of substance use disorder or overdose.
- Mental health conditions (e.g., depression, anxiety).
- Sleep-disordered breathing. • Concurrent benzodiazepine use (6).
Mortality from opiates is highest in those who are middle-aged, have psychiatric conditions, and/or have previously abused substances (7). It is important that clinicians utilize this information when consider risk and benefits associated with opiate therapy.
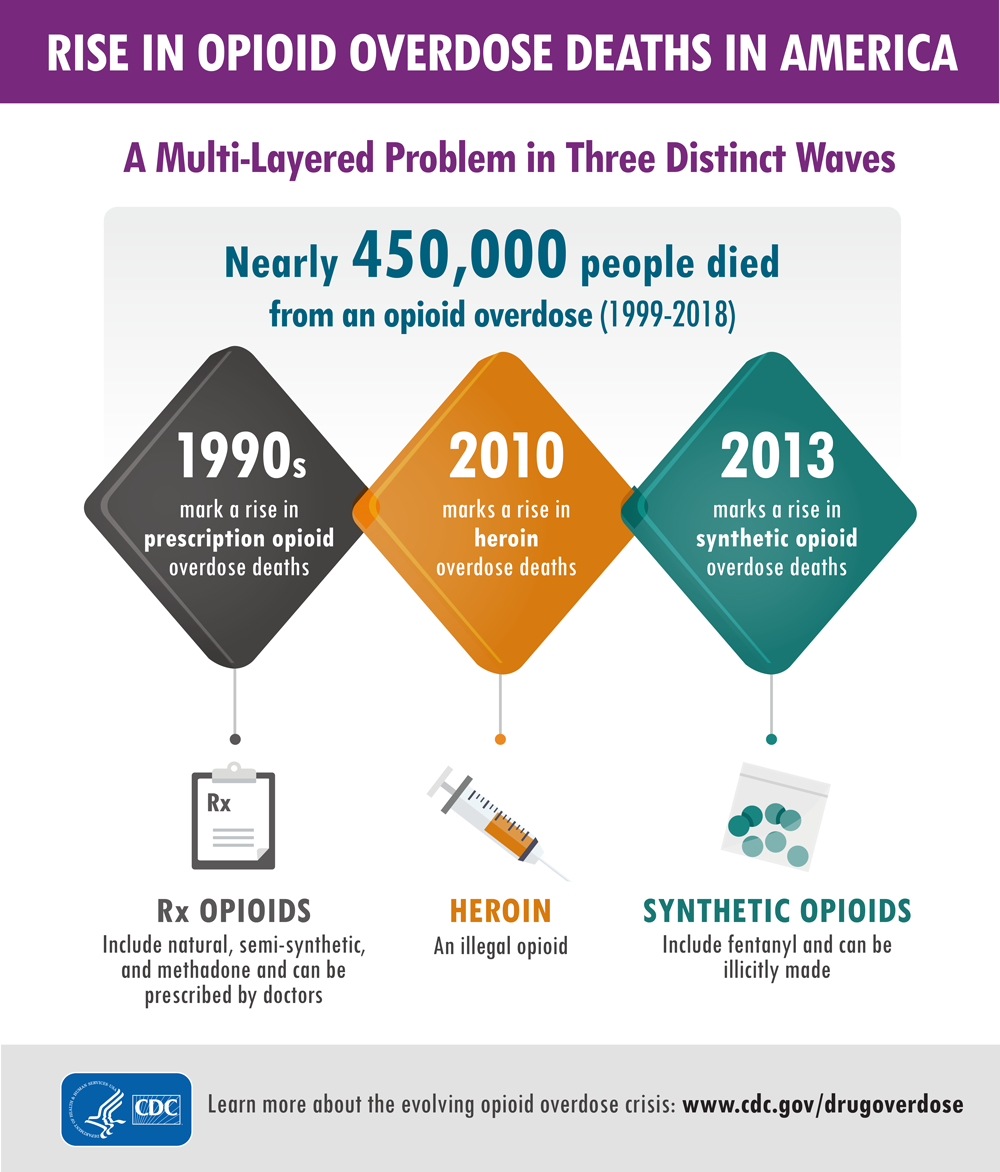
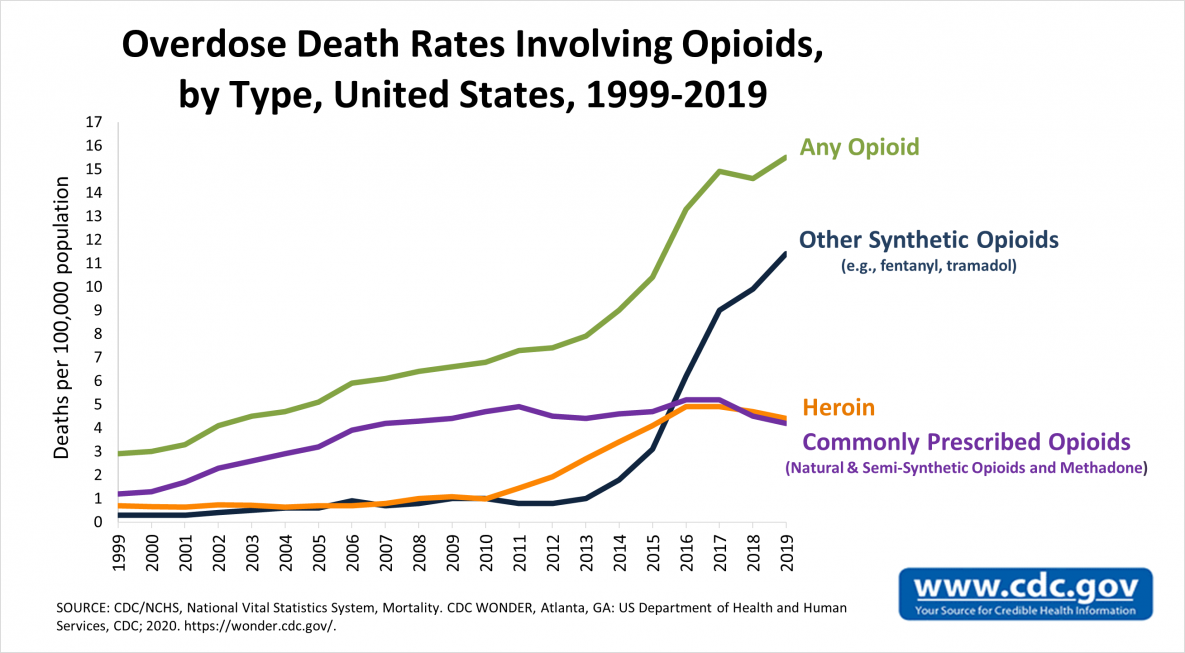
Signs of Abuse, Diversion, and Addiction
Clinicians should remain vigilant for signs of opiate use disorder, as it can occur in any patient (even those not prescribed opiates). Opiate use disorder is characterized in the DSM-5 as a desire to utilize opiates despite social and professional consequences (12). It includes dependence and addiction, with addiction being on the severe end of the spectrum (12). Opiate use disorder can be diagnosed when at least two of the following are observed in a 12-month period:
- Opioids are often taken in larger amounts or over a longer period than was intended.
- There is a persistent desire or unsuccessful efforts to cut down or control opioid use.
- A great deal of time is spent in activities necessary to obtain the opioid, use the opioid, or recover from its effects.
- Craving, or a strong desire or urge to use opioids.
- Recurrent opioid use resulting in a failure to fulfill major role obligations at work, school, or home.
- Continued opioid use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of opioids.
- Important social, occupational, or recreational activities are given up or reduced because of opioid use.
- Recurrent opioid use in situations in which it is physically hazardous.
- Continued opioid use despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance.
- Exhibits tolerance (discussed in the next section).
- Exhibits withdrawal (discussed in the next section) (centers for disease control, reference 13).
Urine drug screening can be useful in patients with suspected opiate abuse disorder as it may identify concurrently abused substances. If a patient is found to have opiate abuse disorder the “risk” side of the “risk-to-benefit” equation is now shifted, and the continued use should be carefully weighed against the potential for negative effects, including addiction. Addiction is defined as continued use despite adverse events or consequences (12).
For those prescribed opiates, clinicians should have candid conversations about the risks of continued use for those with OAD. The CDC offers some creative examples of how to discuss the condition with patients, which nurses may find helpful in their interactions (these are only examples, and the wording depends on the patient’s specific scenario and needs):
“Trouble controlling the use of opioid medication makes it unsafe, and long-term risk over time is substantial.”
“The medicine has become a problem in itself. You have developed a known complication of therapy that we should not ignore.”
“Continuing the current medication is not a reasonable option due to the risks, but there are options for treating what we call opioid use disorder, also known as OUD.”
“It seems as if you are running out of your medication more quickly than anticipated.”
“Sometimes people become too comfortable with the medications and start to take them for reasons other than pain.”
“You meet the criteria for opioid use disorder, also known as OUD. It’s helpful to put a name on it because it opens up a variety of approaches to help with your specific circumstance.” (All derived from source 13).
So, once we identify a patient with OAD, what do we do? At this point, as above, a candid conversation with the patient must occur. A treatment plan should be formulated, which would include a careful consideration for discontinuing for the opiate (if possible). This provides an excellent transition into our next section, opiate alternatives.
Opiate Alternatives
Opiate alternatives can be broadly classified as pharmacologic and non-pharmacologic. We will first discuss pharmacologic alternatives.
Pharmacologic:
Acetaminophen
Commonly known as Tylenol ™ is over the counter and has a very favorable safety profile when used correctly. Acetaminophen is considered first-line therapy in any pain management regimen (9).
NSAIDs (Nonsteroidal anti-inflammatory drugs)
NSAIDs can be immensely powerful in pain management, as many pain conditions are related to inflammation. However, patient tolerance can be an issue with chronic NSAID exposure. Indeed, many clinicians shy away from NSAIDS due to the perceived risk profile (9).
Tricyclic Antidepressants
TCAs provide significant pain relief to many patients, as they have the unique ability to change the perceptions of pain (5). However, tricyclics have many side-effects of their own and thus have been phased out in lieu of newer antidepressants. This in the pain realm they should be considered for certain patients, particularly those with concurrent untreated depression.
SSRI Antidepressants
SSRIs are typically tolerated better than tricyclics (9) but again are not recommend for first-line analgesia. They are typically reserved for those with concurrent psychiatric illness which may benefit from the overall effect of the drug, and on a case-by-case basis for selected patients.
Muscle Relaxants
Medications such as gabapentin can be extremely useful especially in pain originating from musculoskeletal causes. However, the mechanism of action is poorly understood (9) and side effects can be troublesome. In one study approximately 25% of patients taking muscle relaxants for chronic pain discontinued the agents due to adverse effects.
Topicals
Many topical agents now exist, including NSAIDS (9). Topicals are typically considered analgesic-sparing rather than standalone treatment (9). The American College of Rheumatology has excellent and detailed guidance on how to utilize topicals, which deserves a course of its own.
Corticosteroids
Corticosteroids have very potent anti-inflammatory effects (9) and have a proven role in pain management. Short-term therapy is typically favored over long-term therapy due to the potential issues of long-term systemic therapy (osteoporosis, immunosuppression, risk of serious or fatal infections, weight gain, muscle weakness, diabetes, Cushing’s syndrome, hypertension, glaucoma, and cataracts). Though some serious adverse events can occur with short-term therapy (psychosis, anxiety, avascular necrosis, etc.) (9). corticosteroids can be beneficial for patients with acute pain. Perhaps the best use of these agents is in targeted (injectable) delivery.
Non-Pharmacologic:
These therapies will be discussed less in-depth, as they typically require referrals for treatment. However, it is important that nurses are aware of the of the existence of these therapies and can make appropriate referrals and recommendations. Physical therapy consults are invaluable as they often utilize many of the tools below and are more knowledge about non-pharmacologic therapies in general.
- psychological interventions (including distraction, stress management, hypnosis, and other cognitive-behavioral interventions)
- acupuncture and acupressure
- transcutaneous electrical nerve stimulation
- physical therapies (including massage, heat/cold, physiotherapy, osteopathy, and chiropractic) (10)
Conclusion
Nurses should view the non-pharmacologic therapies as “tools” available to help patients dealing with acute and chronic pain. Though opiate therapy is a valuable tool as well, its potential negative effects are often under-considered, and the rate of opiate prescription currently is excessive (10).
When evaluating patients with pain, nurses should work with patients and providers to ensure that the patient is on an optimal pain regimen, which ideally should include both pharmacologic and non-pharmacologic therapies. Seeking referral and consultation from relevant professionals can also be powerful in pain management (physical therapists, chiropractors, psychiatrists, etc.).
Vaping Induced Lung Injuries
Vaping Trends: The Appeal and the Rise in Popularity
What started as a product designed for cigarette smokers wanting to wean off the habit while still allowing them to have the physical ritual of smoking, vaping has now become a cultural phenomenon. Minimal odor, sleek packaging, and few, if any, regulations about when and where people can vape created an appeal even to those who had never used nicotine before and the market quickly turned its attention to gaining new customers through the addition of flavors, additives like THC, and devices that look like flash drives.
The use of electronic cigarettes involves a battery-operated device and a cartridge of nicotine-containing liquid. The liquid is heated into an aerosol which is then inhaled (or vaped). The devices are most popular among adolescents, with 27.5% of high schoolers having used e-cigarettes in the last 30 days in a 2019 survey (1). Adults are using them too, with as many as 2.8% of US adults regularly vaping in 2019, many of whom had never even been cigarette smokers (1).
One of the main reasons vaping has become so popular so quickly is because of the common misconception that it is a low-risk alternative to cigarette smoking, with many companies claiming fewer toxins and not including complete ingredient lists. While e-cigarettes do contain fewer chemicals than traditional cigarettes, they are by no means a “healthy” alternative and contain their own slew of ingredients, including heavy metals such as nickel and lead, glycerin, carcinogens, and nicotine, which is a highly addictive substance (8). The nicotine level in the cartridges is also extremely high, with a typical “pod,” or cartridge, containing the same amount of nicotine as a package of cigarettes (6). This is enough to make even casual users quickly addicted. The FDA has cracked down on these loopholes in recent years, now requiring warning labels and attempting to regulate the production of flavors, but the popularity of vaping has already exploded and the effort to reverse the trend is an uphill battle.

Self Quiz
Ask yourself...
- What prior knowledge did you have about vaping and its posed dangers?
- What vaping induced lung injuries were you aware of?
- What are some misconceptions surrounding vaping, as well as vaping induced lung injuries, that have led to increased popularity?
Health Risks
EVALI (e-cigarette or vaping induced lung injury).
Not surprisingly, the increase in vaping has been followed by a rise in health issues for the users. Most notably among emerging illnesses (and in the media recently) is lung damage referred to as e-cigarette/vaping associated lung injury, or EVALI (2).
A recent Morbidity and Mortality Weekly Report classifies EVALI as a diagnosis of exclusion as there is currently no specific testing for the illness, but it is one that should be considered early in the presentation of symptoms to not delay treatment (3). Most patients affected presented with cough, chest pain, and dyspnea, with many others having fever, chills, weight loss, vomiting, or diarrhea. At least 30% of patients presented with an oxygen saturation of less than 95%. Tachypnea was not frequently noted, but tachycardia was common. Xray revealed abnormal lung findings in 82% of patients and CT of the lungs was abnormal in 96% (3). This emerging issue is placing significant burden on the healthcare system, as most of these patients require inpatient management with steroids and supplemental oxygen, at least for the first 24-48 hours.
When this diagnosis resulted in several deaths in mid to late 2019, it was met with panic in the media and general public as healthcare professionals scrambled to find what exactly about vaping was causing the decrease in lung function. Emerging evidence now strongly suggests that the injury to the respiratory tract is caused by Vitamin E acetate, an additive in many e-cigarette pods (3). Fluid collected from symptomatic patients’ lungs was found to contain Vitamin E acetate in most cases and buildup over time is believed to be responsible for this lung injury (3). It is too early to rule out damage from other additives (like the glycerin used for flavoring) and researchers note that while these components are safe for oral consumption and often found in food, the effects of inhalation have not been studied and frequent exposure to the lungs should not be considered safe (4).
For now, though, Vitamin E acetate is considered the main culprit and is most commonly found in cartridges containing THC, particularly those made informally by people at home rather than those purchased from a manufacturer (3).
While all vaping should be avoided, for those who do use e-cigarettes it is safest to avoid cartridges containing THC and home-made cartridges.
Other Health Concerns
In addition to the potentially lethal complications of EVALI, routine nicotine use of any kind can have serious health implications, and e-cigarettes are no different. Cardiovascular health is affected, with increased heart rate and blood pressure within minutes of nicotine use. Risk of heart attack, stroke, chronic cough, compromised immune system, and impaired oxygenation, all are increased. Nicotine’s effects on a young, developing brain are well documented as well, with attention problems, impulse control issues, and an increased addiction response all posing serious risks to teens who vape regularly (6). Substance use of any kind is closely tied to mental illnesses such as anxiety and depression as well as ongoing struggles with addiction and substance abuse throughout adulthood (6).
The risk of cancer is also not solely tied to traditional cigarettes, with many substances found in e-cigarettes believed to be carcinogenic. A 2018 study tested urine and saliva samples from vaping teens and found the levels of carcinogens present to be significant and concerning (7). In general, the belief that vaping is a low-risk alternative to cigarettes is grossly erroneous.

Self Quiz
Ask yourself...
- Based on the presented evidence, what is the cause of EVALI?
- What are the overall effects of nicotine on the body?
What Can Healthcare Providers Do?
Screen for Vaping Use
One of the best ways to prevent vaping related health issues is to ensure that patients do not start vaping in the first place. Pediatric providers or those working with children and teens 11 years and older are in a particularly advantageous position to start the conversations early and often. Ask questions about what they know about vaping, if they have any friends who vape, and if they themselves have tried vaping. Try to maintain a non-judgmental attitude and allow them to lead the conversation. Provide education to patients and their parents about the dangers and health risks of vaping. Talk about the strengths of the student (academics, sports, arts) and discuss how a nicotine addiction or disciplinary action for vaping at school could negatively impact these enjoyable activities. For any patients who are already vaping, create a plan for cessation (discussed below). Adult patients and established cigarette smokers should also be screened for vaping and health risks discussed (2).
Early Detection of Vaping Related Lung Injury
Screening for vaping is not only important at routine wellness visits, but also for acutely ill patients in the outpatient, inpatient, and emergency room settings. Any patient presenting with cough, chest pain, or other respiratory symptoms should be questioned about current or recent vaping habits, including the use of THC pods. Chest x-ray should be strongly considered in the workup for anyone with respiratory symptoms and a history of vaping, particularly those with a pulse oximetry <95%. Flu and pneumonia should be considered in the differential diagnosis, as vaping increases the risk of both illnesses. In patients hospitalized or treated outpatient for a suspected EVALI, close follow up for the first few weeks is recommended (2).
Cessation
For patients with or without acute lung injury related illness, vaping cessation should be counseled. For adults, many employers will offer smoking-cessation incentive programs which have been shown to be effective. Encourage your patients to ask their employer if this is offered and if they qualify. There are multiple nicotine products designed to help wean slowly from nicotine with the ultimate goal of cessation such as gum, patches, and lozenges. Either gain familiarity with prescribing these yourself or find a local provider who you can refer your patients to for these products (5). Psychotherapy or counseling can be beneficial for patients trying to break an addiction and there are typically addiction counselors available at mental health facilities. There is a Substance Abuse and Mental Health Services Treatment Locator tool that can be found at FindTreatment.samhsa.gov or patients can call 1-800-662-HELP (4357) to find the nearest resources (1). Finally, if you have patients using vaping as a method of stopping cigarette smoking, you should counsel that this is not a long-term solution and has no current supportive evidence as an effective smoking cessation tool. The risks of vaping far outweigh any perceived benefits and vaping should not be counseled as a method of smoking cessation.

Self Quiz
Ask yourself...
- What tools can providers give vapers to help with cessation?
Case Study
Austin is a 19-year-old male presenting to the ED with 6 days of coughing, fever, lethargy, decreased appetite, and (in the last 2 days) increasing chest pain, particularly with deep inspiration.
He is a student at the local university with a history of ADHD for which he takes 20mg of Adderall XR daily. No other pertinent medical history and no other medications. He reports drinking socially on the weekends.
Vital signs are as follows: Temp: 100.9, HR: 147, BP: 134/85, RR: 20, SPO2: 87%. Physical exam reveals pallor, diaphoresis, diminished air exchange in all lung fields with crackles in the bases. Deep inspiration results in coughing fits with no improvement or clearance of crackles and rhonchi. He is most comfortable in the tripod position, but overall is restless. CBC with differential is normal, flu swab is negative. Chest x-ray reveals bilateral infiltrates.
The nurse notices a Juul device in the clear plastic bag of the patient’s belongings and when asked, he admits to vaping ¾-1 cartridge per day for 2 years. He also states he will use a THC cartridge 2-3 times per week with friends.
He is diagnosed with EVALI and admitted for treatment with corticosteroids and supplemental oxygen. He is discharged in stable condition after 2 days with scheduled follow up in 1 week. He is counseled on vaping cessation, particularly of THC cartridges, and makes a full recovery over the next 2 months.
Conclusion
Vaping is a fairly new trend and health risks are still emerging as the number of people using e-cigarettes grows. Staying abreast of trends in vaping and the growing information about symptoms, treatment, and causes of EVALI are important responsibilities of healthcare providers. Early detection of vaping related illnesses is key to best treatment outcomes and screening for vaping should become a routine part of all healthcare exams, both preventive and acute.
LGBTQ Cultural Competence
Introduction
Lesbian, gay, bisexual, transgender, and questioning (LGBTQ) individuals represent a rapidly growing segment of the U.S. population [1]. This rapid growth brings with it risk for stigmatization [1]. Implicit physician biases may result in LGBTQ patients receiving a lower standard of care or restricted access to services as compared to the general population [2]. Even when institutions and providers make commitments to equitable care explicit, implicit biases operating outside of conscious awareness may undermine that commitment. There is an urgent need to ensure that health care providers are prepared to identify and address their own implicit biases to ensure they do not contribute to the health care disparities experienced by LGBTQ and other vulnerable populations. Only by addressing their own implicit biases will health care providers be able to provide patient care in accordance with LGBTQ cultural competence.
LGBTQ individuals face significant disparities in physical and mental health outcomes [3]. Compared to their heterosexual counterparts, LGBTQ patients have higher rates of anal cancer [4], asthma, cardiovascular disease [5,6,7,8], obesity [6], substance abuse [8,9,10], cigarette smoking [11], and suicide [12]. Sexual minority women report fewer lifetime Pap tests [13,14,15], transgender youth have less access to health care [16], and LGBTQ individuals are more likely to delay or avoid necessary medical care [17] compared to heterosexual individuals. These disparities are due, in part, to lower health care utilization by LGBTQ individuals [3, 18,19,20]. Perceived discrimination from health care providers and denial of health care altogether are common experiences among LGBTQ patients and have been identified as contributing factors to health disparities [21,22,23,24]. Disparities in health care access and outcomes experienced by LGBTQ patients are compounded by vulnerabilities linked to racial identity [25,26,27] and geographic location [28].
Biases among health care professions students and providers toward LGBTQ patients are common [29, 30] despite commitments to patient care equality. These biases, also known as negative stereotypes, may be either explicit or implicit [31]. These biases contribute to a lack of LGBTQ cultural competence in patient care. A large study of heterosexual, first-year medical students demonstrated that about half of students reported having negative attitudes towards lesbian and gay people (i.e., explicit bias) and over 80% exhibited more negative evaluations of lesbian and gay people compared to heterosexual people that were outside of their conscious awareness (i.e., implicit bias) [29]. Research in social-cognitive psychology on intergroup processes defines explicit biases as attitudes and beliefs that are consciously accessible and controlled; they are typically assessed via self-report measures and are limited by an individual’s awareness of their attitudes, motivation to reveal these attitudes, and ability to accurately report these attitudes [32, 33]. In contrast, the term implicit bias refers to attitudes and beliefs that are unconscious (i.e., outside of conscious awareness) and automatic [34, 35]. Implicit bias can be assessed with the Implicit Association Test (IAT) [36], which measures the strength of association between concepts [37].
Health care provider biases are correlated with poorer access to services, quality of care, and health outcomes [31, 38,39,40]. Explicit biases held by health professionals towards racial/ethnic minorities, women, and older adults are known to affect clinical assessments, medical treatment, and quality of care [41]. Importantly, implicit bias measures are more strongly associated with real-world behaviors than explicit bias measures [42] and are linked to intergroup discrimination [43]. Health care provider’s implicit biases towards vulnerable patient groups may persist despite an absence of negative explicit attitudes [44], resulting in preconceived notions about patient adherence, poor doctor-patient communication, and micro-aggressions, all of which can interfere with optimal care. With less time and limited information processing capacity, provider’s decisions are increasingly governed by stereotypes and implicit biases [45]. Medical student and provider biases may contribute to health disparities in vulnerable populations by negatively impacting communication with patients and decisions about patient care [33, 35]. Taken together, these findings suggest that medical students and healthcare providers are likely to underestimate or to be unaware of their implicit biases towards LGBTQ patients, particularly when they are rushed or fatigued, which could impact their behavior and judgments in ways that contribute to health disparities experienced by LGBTQ populations. By learning about and addressing their implicit biases, health care providers can work towards demonstrating LGBTQ cultural competence and providing optimal care (Introduction section courtesy of Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P.- reference 45).

Self Quiz
Ask yourself...
- What are some cultural misconceptions regarding the LGBTQ community and providing medical care?
- How can you demonstrate LGBTQ cultural competence in everyday practice?
Terminology
Understanding the standard terminology utilized is pivotal to treating and interacting with LGBTQ patients. Below are listed some of the common terms and how they should be referenced.
Ally – A person not identifying as LGBTQ, but who promotes equality and support of LGBTQ peoples in a variety of ways.
Androgynous – Identifying as neither masculine nor feminine.
Bisexual – A person who is emotionally, romantically, or sexually attracted to more than one sex, gender, or gender identity.
Cisgender – A person who identifies with their gender which as assigned at birth. For example, a person assigned female gender at birth who identifies as female.
Gay – A person who is emotionally, romantically and/or sexually attracted to those of the same gender.
Gender-fluid – A person who identifies as a fluid or unfixed gender identity.
Lesbian – A woman who is emotionally, sexually, and/or romantically attracted to other women.
LGBTQ – Acronym for “lesbian, gay, bisexual, transgender, and queer.”
Non-binary – Adjective describing person(s) who do not identify exclusively as man nor woman.
Pansexual – A person who has the potential for romantic, emotional, and/or sexual attraction to people of any gender.
Queer – Often used interchangeably with “LGBTQ,” or to express fluid identities or orientations.
Sexual orientation – An inherent or enduring emotional, romantic, or sexual attraction to other people.
Transgender –Umbrella term for people whose gender identity and/or expression is different from cultural expectations based on the sex they were assigned at birth. It does not imply any specific sexual orientation and transgender persons may identify as straight, gay, lesbian, bisexual, etc.
*Definitions largely derived from (46).

Self Quiz
Ask yourself...
- Which of the above definitions have you heard used interchangeably?
Best Practices
Below we will list and discuss the best practices for ensuring a positive, equitable healthcare experience for LGBTQ persons, according to the Joint Commission (this is not a comprehensive list, just highlights).
Create a welcoming environment that is inclusive of LGBT patients and demonstrates LGBTQ cultural competence.
- Prominently display the hospital nondiscrimination policy and/or patient bill of rights.
- Waiting rooms and common areas should be inclusive of LGBTQ patients and families.
- Unisex or single-stall restrooms should be available.
- Ensure that visitation policies are fair and do not discriminate (even inadvertently) against LGBTQ patients and families.
- Foster an environment that supports and nurtures all patients and families.
Avoid assumptions about sexual orientation and gender identity.
- Refrain from making assumptions about a person’s sexual orientation and/or gender identity.
- Be cognizant of bias, stereotypes, and other communication barriers.
- Recognize that self-identification and behaviors do not always align.
Facilitate disclosure of sexual orientation and gender identity but be aware that disclosure is an individual process.
- Honor and respect patient’s decisions to provide or not provide sexual and/or gender information.
- All forms should contain inclusive, gender-neutral language that allows patients to self-identify.
- Use neutral and inclusive language when communicating with patients.
- Listen to and respect patients’ choice of language when they describe their own sexual orientation.
- Conduct confidential patient satisfaction surveys that include questions regarding sexual orientation and gender identity.
*Information largely derived from Joint Commission field guide, reference 47.
For more information on best-practices in the workforce, visit the Joint Commission website by clicking here.

Self Quiz
Ask yourself...
- Have you ever misused a pronoun, or overheard a co-worker misuse a pronoun in practice? How can you make sure this doesn’t happen again?
Establishing Relationships with LGBTQ Patients
When interacting with patients, one should not assume gender or sexuality. Addressing a patient who identifies as a female as a male can cause grave harm to the relationship. Instead, nurses should use open-ended questions. For example, rather than saying “Hi sir, what brings you to the hospital,” a nurse might say, “Welcome, what brings you to the hospital today (48)?”
If a nurse uses the incorrect pronoun, the best practice is to apologize and ask the patient what pronoun and name they prefer. For example, a nurse may say, “I apologize for assuming your gender. How would you like to be addressed? (48).
In conversation, the nurse should use the name and/or pronoun the patient prefers without drawing special attention to the subject (48). For example, if a male patient prefers to be identified as his partner’s wife, you should follow suit.
The core of relationship-building with LGBTQ patients is no different than any other patient, fundamentally. If nurses have a basic understanding of best practices and a healthy dose of respect and compassion for LGBTQ patients, a positive relationship is likely to develop.

Self Quiz
Ask yourself...
- Do you have any biases which may affect the care you provide to LGBTQ patients?
- Have you worked for someone who did NOT demonstrate LGBTQ cultural competence? In what ways could they improve their practice?
Health Disparities of LGBTQ Patients
LGBT Americans are at higher risk of substance use, sexually transmitted diseases, cancer, cardiovascular disease, obesity, bullying, isolation, anxiety, depression, and suicide when compared to the general population (49). LGBT youth are frequently bullied at schools (49). In fact, early victimization and subsequent emotional distress accounted for 50% of the disparities between LGBT youth (49). In other words, LGBT Americans are discriminated against and disadvantaged from a very young age.
When home life also reflects a lack of LGBTQ cultural competence, more problems arise. A major cause of LGBT distress is family rejection. Disclosure of gender identity or sexuality can cause very significant interpersonal conflicts among family and friends of LGBT persons (49). This explains some hesitancy and should help nurses understand the importance of respecting privacy, while giving options to patients about disclosing sexuality and gender.

Self Quiz
Ask yourself...
- Are there any circumstances in which your current hospital’s policies could discriminate against LGBTQ families?
- If so, how would you begin to work with leadership to change those policies, so they reflect LGBTQ cultural competence?
Providing an Inclusive and Accepting Care Environment
LGBTQ patients often experience difficulty in finding healthcare environments in which they feel accepted and understood (48). Past negative experiences, lack of knowledge among healthcare providers, and limited access to healthcare in general may become major barriers for LGBTQ persons when seeking care (48).
The core tenant of providing an inclusive environment is understanding the needs of LGBTQ patients and working diligently to create an environment which does not disadvantage or discourage them from seeking care.
Policies and procedures at institutions should be designed to reflect a non-discriminatory environment. For example, many hospital policies dictate that only legal family spouses or partners can visit in specific circumstances. Policies such as this are inherently discriminatory toward LGBTQ patients, as they may not have legal spousal status due to social, legal, or personal reasons.

Self Quiz
Ask yourself...
- Have you ever had an experience where a colleague made a derogatory remark about a patient, based on sexual orientation or gender status? If this happened to you, how would you handle that situation differently?
Exercises on LGBTQ Cultural Competence
To help solidify your learning, please complete the following exercises at your own pace. The answers/guidance for each are provided below.
Scenario 1
A patient enters your emergency department, and you assume the patient identifies as a female. You introduce yourself and say, “Ma’am, how can we help you? What brings you in today?”
The patient appears dismayed but answers the question. The nurse is confused and does not understand why the patient appears distressed. What is the best course of action?
Answer: The nurse should apologize to the patient and ask the patient how they would like to be addressed. Then, the nurse should update the patient’s records to reflect such, to reduce further confusion.
If the nurse does not address the issue, the patient may feel uncomfortable and develop a negative association with healthcare, which can lead to disparities in the future.
Scenario 2
A patient in your ICU has had a deterioration while his husband was in the room. After a family meeting, a member of the healthcare team makes a derogatory remark about the patient’s sexuality. What is the next best action for the nurse?
Answer: Pre-conceived phobias and stigmatizations can cause significant distress to LGBTQ patients, even if not stated directly to them. These types of remarks are abusive and should not be tolerated. The nurse should confront the co-worker (if safe) and consider reporting the comments to the Human Resources department.
Scenario 3
A LGBTQ patient is being admitted and prefers not to disclose their sexuality. However, the nurse is unable to proceed with the admission process without this information. What could be done to rectify this system-level issue?
Answer: The nurse should work with administration to ensure that all charting and paperwork allows individuals to self-report sexuality and/or gender if they want. However, healthcare systems should not force patients to “come out” unless it is absolutely medically necessary.

Self Quiz
Ask yourself...
- What information from this course can you take to your facility to encourage a positive change of LGBTQ patients, and create an environment for LGBTQ cultural competence?
Conclusion
LGBTQ cultural competence must be ingrained in our healthcare systems in order to foster excellent relationships between members of the LGBTQ community and medical staff. Hospitals and healthcare systems have a great deal of work to do in becoming LGBTQ-friendly. The efforts must continue until LGBTQ patients and families do not feel disadvantaged, anxious, or frustrated when interacting with healthcare systems. As the patient’s ultimate advocate, nurses are at the front-line and should advocate for patients both individually and from a policy perspective. Nurses should work with and spearhead efforts to ensure that healthcare policies reflect best-practice and do not discriminate against LGBTQ patients in any way.
Coronavirus: Nursing Considerations
Introduction
The outbreak of the Coronavirus and its slow spread into the United States have caused panic throughout the world over the course of a year. This has caused stress, panic, worry, isolation, and death, leading to many structural breakdowns within the healthcare system, government, and families throughout the world and, more specifically, the United States.
As a healthcare provider, it is imperative to stay informed and up to date on the latest trends, evidence-based practice, and protocols relating to the COVID-19 pandemic as it continues to evolve. As healthcare providers, we are burnt out—mentally, physically, and emotionally—however, it is still our duty to remain steady, and deliver high-quality care to every patient, every time.
What is the Coronavirus? Specifically, what is SARS-COV-2?
Coronaviruses are a group of viruses that have been known to cause moderate to severe respiratory symptoms that may mimic influenza. These symptoms include cough, runny nose, sore throat, body aches, and pneumonia.
Coronaviruses have been affecting humans for several years, but there has not been an outbreak of epidemic proportions since the SARS epidemic of 2003. Coronaviruses are aptly named for the crown-like appearance the virus takes on when examined under a microscope (“corona” is Latin for “crown”) (1). Coronaviruses can range from asymptomatic, to causing symptoms of the common cold, to more severe disease such as severe acute respiratory syndrome (SARS).
In late December of 2019, several cases of unknown origin were reported out of China, which in early January 2020 were announced to have been caused by a novel coronavirus. This virus was later deemed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Despite attempts to contain the disease within its country of origin, the virus has now spread globally, and COVID-19 was declared a pandemic by the World Health Organization in March of 2020.
Signs and Symptoms
The coronavirus disease affects each person differently. Many patients will experience mild disease, while others may develop more severe respiratory symptoms that require hospitalization. Patients present to the emergency department with a variety of symptoms. Nurses have the responsibility to appropriately triage patients, based on severity of the illness, to assist in the efficiency of managing a higher influx of patients, while simultaneously preventing the viral spread of the infection to those patients who have not yet been exposed to COVID-19.
The prevention of an overwhelmed healthcare system includes highly skilled clinical assessment in conjunction with various laboratory and imaging testing, including chest x-ray, blood analysis, and testing for the identification of SARS-CoV-2.
Symptoms include:
- Fever
- Cough
- Shortness of breath
- Headache
- Sore throat
- Nausea/vomiting
- Runny nose
- Myalgia
- Abdominal Pain

Self Quiz
Ask yourself...
- Have you, a friend, family member or patient been diagnosed with COVID-19?
- How did your signs and symptoms compare or differ to each other’s and to the “general” symptoms listed?
Preventative Actions
There are several ways to contribute to the prevention of the spread of COVID-19, including per the Centers for Disease Control and Prevention (CDC, 10):
- Avoid touching eyes, nose, and mouth.
- Avoid close contact with people who are sick.
- Stay at home when you are sick.
- Cover your cough or sneeze with a tissue, then dispose of it properly.
- Use a face covering when physical distancing.
- Clean and disinfect frequently touched objects and surfaces.
- Perform hand hygiene with soap and water or use alcohol-based sanitizer.
What is Considered Close Contact?
Understanding the distinction of close contact is important in the context of triaging and discharging patients; not all exposures are considered close contact.
Please see the criteria below for determining a high-risk exposure (10):
- Patient was within 6 feet of a person with confirmed COVID-19 for a total of 15+ min within a 24-hour period.
- Patient has cared for someone at home who is sick with COVID-19.
- Patient has shared food or drinking utensils with a person with confirmed COVID-19.
- Patient had direct physical contact with a person with confirmed COVID-19 (hugging or kissing).
If someone who has tested positive within the last three months for COVID-19 and recovered has been in close contact with a patient who has suspected or been diagnosed with COVID-19, they do not have to re-test unless they develop new symptoms.
*Those awaiting test results should self-quarantine.
Quarantine vs. Isolation. What is the Difference?
Quarantine refers to keeping someone who has been exposed away from others to prevent potential spread.
Isolation refers to keeping those actively infected away from other individuals to reduce spread. This keeps someone infected with the virus away from others, even in their home (10).
Current Guidelines for Quarantine and Isolation
Who Should Quarantine?
Patients should quarantine at home if they have been in close contact with someone who has tested positive for COVID-19, excluding those who have had COVID-19 in the past 3 months (10).
Ideally, patients should stay home and monitor for symptoms for 14 days after their last exposure to a close contact. Recognizing that this can be difficult, the CDC allows options for reducing quarantine time (see below).
If possible, instruct patients to stay away from those at high risk of severe illness from COVID-19.
Options to Reduce Quarantine
These guidelines have been released by the CDC, giving the authority to reduce quarantine to the local health departments (10). The theory behind reducing quarantine is that it will increase compliance and minimize the burden on society, while balancing a reduction in virus spread. However, it is important that patients understand the importance of proper quarantine.
Patients who are exposed and do not develop symptoms may end quarantine 10 days after exposure if no test is administered.
Patients who are exposed and do not develop symptoms may end quarantine 7 days after exposure and after receiving a negative test (test must occur on or after day 5).
*If patients develop symptoms during quarantine, even with a negative test, they should be considered COVID-19 positive.

Self Quiz
Ask yourself...
- Have you heard the terms “quarantine” and “isolation” being used interchangeably?
- Have you been told similar or different protocols in managing your personal or family’s COVID diagnoses?
Options for Testing
There are several different tests available for COVID-19. They can be used for diagnosing acute infection, to guide contract tracing, and in some cases to determine if a patient has previously been infected by the SARS-CoV-2 virus. It is important for nurses to understand the limits of testing.
Testing for active infection (symptomatic or asymptomatic) is an important strategy for controlling the spread of the virus. It is important to know when it is appropriate to test a patient.
In general, testing should be considered for the following:
- People with symptoms of COVID-19
- People who have close contact with someone who is COVID-19 positive.
- People who are asked or referred by their healthcare provider or local health department.
*Patients with recent COVID-19 disease (past 3 months) do not require testing for subsequent exposures unless symptoms are present.
**Based on CDC data (3).
Viral Test
Viral tests are diagnostic and use samples from the respiratory system, such as nasal or oral swabs, to determine the presence of infection with SARS-CoV-2.
- This type of test tells you if a patient is currently infected with the disease.
- Recommended to diagnose acute infection in symptomatic and asymptomatic patients.
There are currently two types of authorized SARS-CoV-2 viral diagnostic tests that use different technological principles: molecular and antigen. Each of these detects a different part of the SARS-CoV-2 particle.
Antibody Test
- This type of test can show you if a patient was previously exposed or infected with SARS-CoV-2 and carries the antibodies.
- Detects the presence of IgG or IgM against SARS CoV-2.
- Not authorized by the Food and Drug Administration (FDA) to diagnose SARS-CoV-2 infection.
- Used to support a clinical assessment of persons who present in the later stages of illness when used in conjunction with viral testing (2, 3, 4).

Self Quiz
Ask yourself...
- If you tested positive for COVID-19 two months ago, but were exposed to a positive patient, within 6 feet without a mask on, is the current recommendation
to get a COVID test?
Pharmacologic Treatment
For pharmacological treatment, it is important to understand that we are in our infancy of understanding SARS-COV2-2 and COVID-19 infection. Though there are a plethora of low-quality studies demonstrating benefit for some agents, most experts feel that we should wait for more conclusive data before utilizing agents on a large scale.
Remdesivir is currently the only drug approved by the FDA for the treatment of COVID-19. It is recommended for non-intubated hospitalized patients requiring supplemental oxygen.
Dexamethasone is the only recommended treatment in patients requiring increasing amounts of supplemental oxygen and in intubated patients.
Diagnosis and Management
Imaging can be useful in the diagnosis and prognosis of COVID-19 but is not required for a clinical diagnosis. Early in the disease, imaging may not correlate with the severity of the disease.
Because COVID-19 usually manifests itself as pneumonia, radiological imaging has a profound role in assisting the diagnosis of the disease, management, and follow up. In the early stages of the disease process, the results can be un-impressive and assumed as negative findings (5). In the advanced stages, radiological findings typically reveal patchy ground-glass opiates, with infiltrates favoring the bases and periphery of the lung fields. The infiltrates are typically bilateral, and pleural effusions can be present (6). Lung inflammation may progress to the level of fibrosis in respiratory failure (5).
Patients with COVID-19 experiencing hypoxia should receive supplemental oxygen with a target oxygen saturation of 92% to 96% (18). Patients requiring oxygen fall into the category of moderate-critical illness of COVID-19. Severe illness in COVID-19 patients typically occurs one week after symptom onset. The most common symptoms presenting in these patients are dyspnea accompanied by hypoxemia (9). These patients with severe disease usually require supplemental oxygen and should be monitored closely for respiratory status because these patients may be at risk for progressing to critical illness with acute respiratory distress syndrome (ARDS).
COVID-19 Vaccines
Currently, three vaccines are authorized and recommended to prevent COVID-19 in the United States
- Pfizer/BioNTech’s COVID-19 vaccine (mRNA)
- Moderna’s COVID-19 vaccine (mRNA)
- Janssen Covid-19 vaccine (adenoviral vector)
Many people have questions related to the new COVID vaccines. As healthcare providers, you play a critical role in helping patients to understand the vaccine and the varying risks and benefits.
- All vaccines are recommended for intramuscular injection into the deltoid.
- The mRNA vaccines are recommended for two doses one month apart.
- The adenoviral vector vaccine is recommended as a single dose administration.
Effects of Long COVID
Although it may feel like COVID-19 has been around for quite a long time, the reality is that our understanding of the disease is just getting underway. As the pandemic continues to progress, there is a growing recognition that people are experiencing the long-term repercussions of the SARS-CoV-2 virus, which may persist for months or even years.
Contrary to widespread belief, health status is not protective against developing Long COVID. Current data shows that young, healthy patients experience Long COVID at similar rates to those with advanced age and poor health status. Even those with mild to moderate illness not hospitalized are showing delayed or long-term symptoms (7).
We are slowly learning more about how COVID-19 is chronically affecting patients. The long-term effects are not limited to the lungs and have been reported to affect all organ systems. The most common symptom reported is crippling fatigue. You can find a list of the common Long COVID symptoms in the chart below (7).
COVID-19 Variants
All viruses mutate over time—some mutate more than others. A new strain occurs when there is a mutation in the genes of the virus. There have been three new strains of the virus seen throughout the world to date since September of 2020. The mutations in the new strains are affecting spike proteins, which are on the surface of the SARS-CoV-2 virus, which gives it its “spiny” appearance. These proteins allow for the virus to attach to human cells and invade the body, leading to illness (8).
One of the main concerns is whether any of the variants could affect treatment and prevention. Mutations may allow the coronaviruses to escape the antibodies in currently available therapies and those induced by vaccines. There is new evidence from laboratory studies that some immune responses driven by current vaccines could be less effective against some of the new strains. It is not yet known if those who have already received the COVID-19 vaccine could get sick with the new variants (8).

Self Quiz
Ask yourself...
- What are the three different types of COVID-19 vaccines approved by the Food and Drug Administration for COVID prevention?
- Have you, a family member, or patient experienced lasting symptoms of COVID-19 or other symptoms that can be categorized as a long-term effect of COVID-19?
Conclusion
As time continues, and we as a country and world try to manage our day to day lives with the current and aftereffects of the pandemic, it is imperative that nurses be up to date and armed with the latest knowledge of the virus in order to manage and care for their patients efficiently and effectively. Improving patient outcomes and saving lives of patients experiencing current or long-term effects of the SARS-CoV-2 virus.
Effective Communication in Nursing
Introduction
Communication in nursing is key, and the ability to communicate effectively can be our lifeline. We depend on ourselves and others to be fluent and effective in the art of communication in order to perform our role as nurses successfully. When any link in our communication chain fails, we immediately see poor outcomes, wastage of resources, reductions in patient and staff satisfaction as well as a decline in the quality of patient care (1).
Types of Communication
In order to master effective communication in nursing, it is important to understand the various types of communication, their definitions, and the impact they can make.
Non-Verbal
This form of communication relies solely on the utilization of body language, including body and facial mannerisms, and completely lacks spoken words or sounds (2). We perform and identify non-verbal communication in nursing daily without giving it a second thought. We may see a newborn sucking on their hands, providing us a non-verbal cue that they are hungry. When assessing a patient holding their abdomen, we would look to initially target that area because they have communicated (non-verbally) that this is where they are experiencing discomfort. Smiling when the next shift nurse is walking in the door communicates to them that you are happy to see them, and that it’s about time for you to go home!
Since we perform non-verbal communication so often, it can become an incredibly powerful tool or an extremely negative one. This form of communication in nursing can be used positively to show our patients and co-workers that we have compassion, and we are engaged. Negative forms can make patients uncomfortable with sharing their medical history and result in a lower quality of patient care. Additionally, it can lead to dysfunctional teamwork among staff.
Verbal
Verbal communication occurs when we use words or sounds to discuss concepts with others (2). This form of communication in nursing has the conception to be a very easy notion, but it can create unfavorable consequences when used ineffectively. In order to produce clear verbal messages, we should always speak concisely and with confidence. As health care professionals, we have our own language, and understanding when to incorporate our medical jargon into conversations versus when to not is crucial in providing care. When communicating among co-workers, our medical knowledge can display professionalism and it is evident that they can follow along. However, when speaking with patients and their families, this may not always be the case and we must be able to effectively gauge our audience and ensure that they have a clear understanding of what we are teaching or explaining; this is an extremely valuable tool.
Written
This form of communication can be either a formal or informal transcription of words that are intended to serve as a direct communication form (2). Written communication in nursing is used daily and incorporates one of our most important duties, documentation. Throughout our nursing practice, we have learned the importance and necessity of our documentation; it can be useful for legal protection or provide critical data to other health care professionals. Written communication can also be accessed through the policies and procedures we employ to perform various tasks. Having sound, written communication, and interpretation skills is vital to the overall success of our nursing career.

Self Quiz
Ask yourself...
- What type of communication is being interpreted while watching a patient walk to the bathroom?
- Upon admission of a female patient for a fall, you are performing normal intake questions and a physical assessment. The patient is quiet and uses minimal verbal communication and looks down at the floor while you are in the room. What communication types are you interpreting?
Receiving Communication
The most common communication perception is usually directed to producing communication through non-verbal, verbal, or written forms. While the production of communication is important, the reception of it potentially holds even greater value. In nursing, ensuring our communication is received correctly affects every clinical, orientation, or job experience we have encountered thus far.
Think about it…
- Taking notes in class or during a shift.
- When a preceptor or instructor educates you on a brand-new skill or piece of equipment.
- Teaching your patient, family, or student about a new diagnosis.
- Watching your patient breathe for rate, depth, and effort.
We must provide and receive communication in nursing through verbal, non-verbal, or written forms successfully. If communication fails, we will experience extremely negative effects throughout our entire nursing system.
Hearing & Listening
Hearing describes the process or act of perceiving sounds or spoken words (2). We hear sounds upon auscultation, varying frequencies of alarms, and patient concerns when they are voiced. Hearing all these sounds are heavily dependent on how they are used. To achieve successful implementation of these sounds, we must also listen to these sounds and words. To listen, we must hear and then interpret these sounds carefully (2). We interpret these sounds and words by asking additional questions, performing additional assessments, or paraphrasing the information presented.

Self Quiz
Ask yourself...
- What is the best way to ensure a patient was actively listening while performing patient education?
- Which type of scenario requires active listening skills?
a. Putting blood tubing into a pump.
b. Watching an EKG monitor.
c. Performing a pain assessment. - What techniques show others you are actively listening?
a. Reading a document while being talked to.
b. Making eye contact.
c. Making noises while someone is talking.
Communication Transmission Threads
Communication in nursing occurs multiple times a day between a wide range of communication threads. The type of communication through non-verbal, verbal, and written communication produced and received, must be effectively performed. Success and implementation are heavily dependent on the communication between the nurse and the communication thread.
Nurse-Nurse
Communication among nurses is continuous throughout a shift while working within a team environment. Whether it is us passing our documentation on to another nurse for review or vice versa, there is consistent communicative flow of all variants (non-verbal, verbal, and written) between the team in order to provide care for patients.
Nurse-Ancillary Staff
Your team members will vary depending on your nursing career setting, but some items will remain consistently important despite wherever you are. We must provide clear verbal communication when delegating or reporting critical information from the nurse to ancillary staff participating in patient, client, or resident care.
Charge Nurse-Team
When stepping into a charge nurse role, there will always be unexpected tasks, staff conflicts, or emergent situations. In this position, you will be taking all the communication skills you have acquired and putting them into practice at an all-time high. As the charge nurse, you will be viewed as a leader, meaning that you are a role model for your fellow team members. Now, in addition to producing and receiving communication effectively, you will now be identifying poor communication and assisting with its correction.
Nurse-Patient
The nurse-to-patient communication thread is one of the ultimate and most important exchanges in the nursing profession. Patients need us, so we must be able to keep consistent and effective communication flow with them because any assessment, report, and administration of medication is contingent upon it.
Nurse-Family
The thread between the nurse and the patient’s family can be the foundation for your nurse-to-patient communication and its effectiveness. The family could be the responsible party or guardian for your patient and could potentially serve as your sole historian for patient information if the patient is unable to communicate at the time of data collection. Ensuring that the family is aware of and understands discharge instructions can further help them to recognize any potential signs or symptoms that could result in calling a physician or visiting the emergency room in the future.

Self Quiz
Ask yourself...
- Which of the following is a beneficial way to ensure effective communication throughout multiple threads?
a. One to one conversation.
b. Reviewing a policy.
c. Bedside report.
Barriers & Improvements to Communication
Barriers of communication in nursing happen frequently and are sometimes out of our control. These barriers include:
Language barriers
Utilizing available resources for language barriers through interpreter staff members or interpretation devices can ensure effective communication pathways between two individuals.
Cultural differences
Identification of cultural differences during admission and cultural awareness will allow for effective communication management throughout each culture you are presented with.
Patient acuity, staffing levels, time constraints
Patient acuity, staffing levels, and time constraints can be improved by utilizing staff huddles and working together with administration in order to overcome conflicts.
Emergent situations
Emergent situations that arise during your shift can be relieved through adequate knowledge of the policies and procedures and by performing debriefs after the situation resolves. Debriefings hold valuable insight into reflections of the emergent situations we face as nurses, especially on communication performance.
In each thread and form of communication in nursing, we must remember the following items to receive information. While producing communication, we must always be clear, concise, and accurate with the correct corresponding tone when expressed to others. When we are receiving the information, we must ensure we are understanding, investigating, and acting according to the communication presented to us. Utilizing various communication platforms, including emails, boards, and group messaging apps, can help to assist in ensuring education is received.
Benefits of Effective Communication in Nursing
When we achieve effective and therapeutic communication between both our team and patients, it will create opportunities for enhancements throughout our practice. Fostering a unity of teamwork with co-workers will increase satisfaction and reduce burnout rates. Reduced health care costs through reduced readmissions or emergency room visits will be established by successful patient education and understanding. Our quality of patient care will be heavily influenced by the nursing communication threads created through their care.
Nursing Documentation 101
Introduction
“I just love charting,” said no nurse, ever. If you ask most people why they want a career in healthcare, their response is that they wanted to help people. They did not want to spend hours in front of a computer clicking boxes. This time-consuming task of documenting in the medical record, or charting, is dull, repetitive, and sometimes disconcerting. It takes time away from being able to provide care for the patient. Yet documentation in the medical record is truly a vital part of patient care.
Nursing documentation fills a significant portion of the medical record. Nurses need make sure what they are adding is accurate and complies with the guidelines set by their facility and the state board. This principle is the same, even though there are differences to be aware of now that the electronic medical record has become the standard.
The Who, What, When, Where, Why, and How
Who:
There are approximately 2.9 million working RNs in the United States, with about 1.6 million working in hospitals (1). Nurses on a med-surg unit typically spend about one-third of their total working hours documenting (2). Considering a nurse on a med-surg floor spends about 2.5 hours per shift charting, that roughly translates into 7 billion hours spent charting each year. And that is only for the nurses!
Every discipline of the healthcare team contributes to the patient’s medical record. These different clinicians may not have the opportunity to report off to one another, and they must refer to the medical record to gather the information they need in order to care for the patient. Even kitchen staff responsible for preparing meals for patients must be able to see the dietary order for the patient. The following are a few examples of the clinicians who contribute to or review the patient’s medical record:
- Medical Team: physicians, nurse practitioners, physician assistants, surgeons, specialists, residents
- Nurses and LPNs
- Medical Assistants, CNAs, patient care assistants or technicians
- Specialty technicians: radiology, anesthesia
- Therapists: physical, speech, occupational, respiratory
- Pharmacists
- Dieticians
- Case managers or social workers
- Coding and billing specialists
- Researchers
What:
The primary purpose of the medical record is to communicate data about the patient and care provided between different members of the healthcare team. The bulk of the medical record is a collection of assessment data obtained from the patient. Details concerning assessments and results from lab tests or radiology comprise a large portion of the data. Assessment data is usually collected on a flow sheet system. Progress notes are written by the medical team or therapists help to guide the intended plan of care for the patient. This is considered narrative charting. The medical record also includes orders for prescribed medications and treatments from the medical team. The following are typical components found in a patient’s medical record.
- Patient demographics: name, age, gender, contact information, language, insurance information.
- Past medical history: surgeries, chronic conditions, family history, allergies, home prescriptions.
- History and Physical (H&P): this can contain information about admitting diagnosis or chief complaint and narrative of the story leading to admission.
- Flowsheet of assessment data: vital signs, head-to-toe assessment, intake and output record
- Laboratory test results.
- Diagnostic test results: from radiology or procedures.
- Clinical notes: progress notes from the medical team, procedure notes, notes from consulting clinicians, education provided, discharge planning.
- Treatment Orders.
- Medication Administration Record (MAR).
When:
The medical record should document every interaction the patient had with a member of the healthcare team. An encounter is created upon admission and everything occurring during a particular admission becomes part of the medical record. Phone calls made to patients and/or families may also become a part of the medical record.
Where:
Medical records are stored in various ways depending on their format and the facility. Paper records from small outpatient offices may be kept onsite. Records are now largely kept electronically. This is referred to as the electronic medical record (EMR) or electronic health record (EHR) and consists of Protected Health Information (PHI). They will be stored on a secure server, typically only accessible by authorized personnel.
Why:
The medical record is essential for several reasons. The primary reason for the medical record is that it allows members of the healthcare team the ability to review and analyze data in order to deliver appropriate care. It allows clinicians to keep track of all the care that has already been completed for the patient. It also provides the patient with a record of the treatment they received for as part of their lifetime medical history. The medical record is used for coding and creating a bill for the services the patient received. Medical records may also be used for process review and research. Ultimately, it is also a legal document and may be used in a court of law as applicable.
How:
Medical records are in the final stages of evolution from a paper chart to an electronic medical record system (EMR). By 2017, 96% of acute care hospitals and over 80% of physician offices possessed certified health IT (3). This migration of medical records from paper to electronic format was made possible with advances in technology in the last 30 years. The EMR allows members of the healthcare team to access the medical record instantaneously and improves continuity of care. Utilization of the EMR ultimately reduces costs in healthcare (4) and increases efficiency.
While EMR does have some drawbacks, the benefits that it provides are substantial enough that the government has encouraged its adaptation. The Health Information Technology for Economic and Clinical Health (HITECH) Act was enacted in 2009. This program provided tens of billions of dollars in financial incentives for healthcare facilities to adopt an EMR system (5,6).
Privacy and Security
Since 1996, HIPAA, The Healthcare Information Portability and Accountability Act, has been the governing legislation that provides for the privacy protection of medical records. Compliance with HIPAA mandates that anyone who interacts with patients receives training that will ensure that they will maintain privacy for the patient. Part of the HIPAA legislation also allows the patient to request their medical records.
The patient also has the right to request to amend their medical record. Patient permission must be given prior to a third party’s access to their medical record (7). HIPAA legislation was introduced at the advent of EMR technology. A provision of HIPAA provided a framework to ensure privacy of electronic health records (8). However, breaches in security by hackers or cyberterrorists remains a potential threat.
Benefits of EMR:
- Immediate data accessibility and communication of patient status.
– Clinicians can view records remotely, analyze the findings, and place orders immediately for faster patient treatment.
– Multiple clinicians can view the chart at one time.
– Records can be viewed from previous admission and/or outpatients visits easily.
– Records can be instantly shared between facilities (in instances of shared systems)
- Reduction in errors.
– Errors due to misinterpretation of handwriting are eliminated.
– Allows for increased safety checks. The EMR can be set to flag missing components of information, tasks that were not yet completed or are overdue, recognize duplicates, and present warnings if documentation has not yet been validated or “signed.”
– Scanning medications is possible with EMR systems to reduce the risk of medication administration errors.
- Assists with appropriate billing by capturing charges of services provided to the patient.
- The EMR can provide reminders for necessity of certain preventative health screenings or vaccines.
- Automatic “signature” of data is completed simply by the user logging in with a unique ID and password. All entries are date and time stamped. If a correction is made, the original data can be accessed.
- Accessing patient EMR is tracked and can be audited to protect patient privacy from unnecessary viewing.
Downsides of EMR:
- It is expensive to convert records system to an electronic system.
– The initial cost of the EMR software is very expensive.
– More workhours must be paid for staff training and coverage of patients during initial implementation of the program.
– Maintaining appropriate encryption and cybersecurity technology against viruses and hacking are also a costly component.
- Computer systems can be temporarily inaccessible, for example when updates and reboots are required. Paper charting is still necessary in the interim.
- Template charting has limitations (9)
– Templates may not exist for a specific problem and does not accurately reflect the patient’s condition. Atypical patients may have multiple problems or extensive interventions that must be documented in detail.
– Templates may also encourage cloned or copied documentation. It creates unnecessary redundancy and at times inaccurate information in the EHR. Some EHR systems are designed to facilitate cloning with such popular features as:
– “Make me the author” to assume the content of another person’s entry,
– “Demo recall” of “Duplicate Results” to copy forward vital signs or assessment data.
– “Smart phrases” pulls in specific identical data elements.
– Automated insertion of previous or outdated information through EHR tools, when not modified to be patient-specific and pertinent to the visit, may raise significant quality of care and compliance concerns.

Self Quiz
Ask yourself...
- Think about your current charting system.
- How does your medical record system facilitate accurate charting?
- Do you believe that your system is efficient?
- What are some issues with your system that make it difficult to accurately and timely chart nursing care?
The Legal Requirements
If it wasn’t documented, it wasn’t done. Every healthcare practitioner has had this mantra ingrained in them from the very beginning of their career. Nurses are trained to document defensively, that is, if they are taught at all.
In a 2014 study, only 20% of new graduate nurses had received electronic medical record training as a part of their nursing school curriculum (6). It is not uncommon for clinicians to have the tendency to view the medical record as a defense tool against potential legal problems, rather than its more significant role as a communication tool for patient care.
Regardless, accurate and complete documentation is an essential. Your career, and more importantly, patient care, depends on it.

Self Quiz
Ask yourself...
- Did you receive proper training on documentation in your nursing program?
- How can programs be improved to better prepare nurses?
When Documentation Becomes Your Defense
In the dreaded event of a legal problem, medical record will be scrutinized to every detail. It is usually the primary source of evidence for the case. A malpractice lawsuit requires four elements to be proven (10):
- That a medical professional assumed a duty to provide care for the patient.
- The clinician failed to provide appropriate care within their scope of practice for the patient.
- The failure in appropriate care caused an injury to the patient.
- The injury resulted in damage to the patient.
Potential legal problems that may arise include the following (11):
- Administrative liability – Professional licensure discipline, discharge (firing) from position.
- Civil Liability – Malpractice lawsuit, failure to provide necessary care.
- Criminal liability – Misdemeanor or felony charges for cases of gross negligence.
The Cost
Fortunately, medical malpractice claims have begun to drop since 2001. In 2004, the medical practitioners involved, the defendants, won the case 83% of the time. The legal fees can still amount to $18,000 if the case is dropped, to as much as $93,000 even when the case is won (12,13).
In 2018, there were 8,718 malpractice cases that resulted in payments to injured patients (14). Of those events, 310 reports of malpractice suits that resulted in payments related to nursing care.
However, 180 of those, about 60% of those had payments to the injured patient that were over $50,000 (14). However, there were nearly 15,000 adverse action reports filed against nurses, which was more than the number combined filed against physicians, NPs, and PAs combined.
The majority of medical malpractice cases primarily target the physician and the facility. However, anyone who made an entry into the patient’s medical record may be required to participate in legal proceedings.
Most common malpractice claims against nurses include failure to (15):
- Follow standard of care.
– Follow safety protocols.
– Perform procedures according to guidelines.
- Use equipment properly.
– Use or operate equipment within the manufacture’s details.
- Failure to correctly document.
– Communication with the provider.
– The care you completed.
- Follow assess and monitor.
– Report a change in status of the physician.
– Assess a patient with change in status.
- Communicate pertinent data.
– Provide appropriate discharge education and information.
– Communicate properly and completely between shifts.

Self Quiz
Ask yourself...
- Think about the last difficult shift you had. Did you properly document?
- How would you prioritize documentation differently after reading this module?
What is Required for Nursing Documentation?
Necessary medical record documentation can vary significantly depending on the care area. For example, the documentation a circulating nurse in the operating room completes will be very different from what is documented on an emergency room patient. While the basic principles of documentation stay constant, the nurse needs to be familiar with the documentation requirements for that area based on requirements of the state board of nursing, the facility, and the unit.
There are standard requirements for medical record documentation that are applicable in all patient care settings, and in both paper and EMR systems. These standards include the following (16):
- Accurate: Clinicians must be careful to proofread documentation to make sure it is free from errors. A small typo can have serious repercussions, as it is more likely to be misinterpreted by others.
- Relevant, concise, organized, and complete: It is important to keep the information concise and relevant so that other care providers can quickly find the pertinent information that they need. Assessment data should be entered in a systematic way. Complete documentation ensures all of the unit policies for documentation are addressed.
- Free of bias: Clinicians should only include information that is pertinent to the care of the patient and remain free from personal bias. Direction quotations should be utilized with proper context.
- Factual: Clinicians should not exaggerate or minimize findings. Charting is to be completed after completing a task, not before. Do not speculate data. Observations need to include exact times and measurements. Avoid approximations. Make sure to chart on the correct patient.
- Timely: What occurred during the shift should be documented during the shift. Documentation should be done as soon as possible after task completing. If something needs to be added in after the shift was completed, it should be denoted as a late entry with a reason as to why. Your facility likely has strict requirements regarding late entries.
- Legible/decipherable and clearly written: Paper documentation must be clearly legible. Writing must clearly convey meaning.
- Standardized: Clinicians must use appropriate medical terminology and approved acronyms and abbreviations.
- Labeled and Auditable: Paper documentation must be signed with credentials and must include date and time of the entry. When charting in the EMR, all entries and corrections are recorded, and time stamped. Password sharing or having another clinician assist in documenting under incorrect username is fraudulent.

Self Quiz
Ask yourself...
- Do you currently incorporate all of the above principles in your documentation?
- If not, how can you change your practice to improve your documentation?
Examples of Good and Bad Charting
The following will show some examples of these principles in action. These are based on the scenario of a patient admitted in the Emergency Department for chest pain.
| Example of good documentation | Example of poor documentation |
Accuracy | Patient stated she took 800mg of Tylenol at 4pm, an hour after she began to feel chest pain. | Patient reports she took pain med for chest pain. |
Relevant | Patient stated she has never experienced chest pain prior to this event and does not have a history of cardiac problems. | Patient was a competitive athlete 20 years ago and used to be in great shape. Patient thinks she is still pretty healthy. |
Concise | Vital signs taken, telemetry monitor applied, lab samples collected, and PIV started per the chest pain protocol. | Patient was triaged and immediately brought to exam room. In accordance with the chest pain protocol, vital signs were taken first. Then the patient had a telemetry monitor applied. Next, the patient had blood samples drawn through the inserted PIV catheter. |
Organized | Pt reports no allergies. Prescriptions include hormone replacement therapy. Past medical history includes hysterectomy and foot surgery from a few years ago. Patient family history includes cardiovascular disease on her father’s side of the family. Pt denies smoking, illicit drug use, but does drink 3 times a week. Pt reports feeling fine until 1 hour after lunch when chest pain began. | Patient was feeling fine until one hour after lunch, when she started to feel chest pain. Patient has no history of cardiac problems. However, there is family history of cardiovascular disease on the father’s side. Patient had a hysterectomy and foot surgery a few years ago. Patient denies smoking and illicit drug use. Patient does take hormone replacement therapy prescription. Patient does not have any allergies. Patient reports drinking alcohol x3/week. |
Complete | Patient complaining of 8/10 chest pain, described as “stabbing.” Pain has been experiencing this pain for three hours. She has taken Tylenol, but nothing is able to alleviate the pain. | Pt is complaining of chest pain. |
Free of Bias | Education provided per chest pain protocol. Patient was instructed to call 911 immediately if experiencing chest pain in the future. Patient verbalized understanding. | Patient was given needed education about chest pain since she clearly didn’t understand that chest pain cannot wait 3 hours and she need to call 911 right away because she can die of a heart attack. |
Factual | Patient reports last meal was around 1300 which consisted of spicy foods. Her chest pain onset was 30 minutes after. She waited an additional three hours before seeking emergency care. | Patient presented to ER after lunch. |
Legible and Decipherable | Patient was instructed to call for assistance with ambulation and how to utilize call light. | Patient cannot safely walk by she self. Call light assistance. Bathroom walk with me. |
Standardized | Morphine Sulphate 2mg IV push, once PRN for 8/10 pain per chest pain protocol. | MSO4 2.0 mg, IV push, x1. |
Timely | Documentation is completed in real-time, all documentation completed before transferring patient to telemetry. | Nurse documents three days later due to high volume of patients. |
Common Documentation Errors
- Falsification of a record. This can happen from charting an action was never done, or from charting information before the action was completed.
- Fraudulent charting is the act of knowingly making a false record. Criminal charges of forgery can result if the misrepresentation was done for personal gain. An example of this would be a nurse documenting administration of controlled substance but was instead diverting the medication.
- Inappropriate use of cloning features. Information “copied and pasted” from a different patient’s record or that was completed by another provider. Data copied from previous shift assessments that isn’t updated to reflect current status is also a false record (9).
- Fail to document communication. Notification of the medical team of a change in patient status or critical lab values should always been included. Clarification or confirmation of orders should also be documented (17). Include notification of other providers who assisted with patient are. This includes failure to document transfer of care to another nurse.
- Failing to document a reason why something wasn’t done. If a patient doesn’t receive a prescribed medication, the reason why the medication wasn’t given needs to be described. If you communicate with the provider, this should also be included.

Self Quiz
Ask yourself...
- Have you ever failed to document or failed to document a critical portion of care?
- If you could alter your documentation, how would you better document in this situation?
Conclusion
Including all of the necessary information into each patient’s medical record is a daunting task. The nurse must make sure that they have included all of the relevant and accurate information that is required by their facility guidelines. It must usually be done in a loud environment and is frequently interrupted by actually having to provide care to the patients.
It is not only a tedious chore, but it also tends to cause a lot of apprehension. There is usually a worry of “did I chart enough?” or “did I chart everything I needed to?” This is due to the defensive practices and attitudes healthcare workers have adapted to protect against malpractice lawsuits. In this way, charting is a lot like paying taxes. No one likes it, but it still has to be done.
Perhaps a way to develop a healthy perspective toward charting is to change the focus back to its original purpose: to communicate care about the patient. The purpose of charting is to relay to the other healthcare team members what is going on with the patient. With this objective in mind, the nurse will inevitably cover all the necessary details. It may also be a bit more satisfying to know that even though they are in front of the computer, they are still doing something important for the patient.
References + Disclaimer
Texas Nursing Jurisprudence and Ethics
- American Nurses Association. (2015). Code of ethics with interpretative statements. Silver Spring, MD: Author. Available from URL:
- http://www.nursingworld.org/MainMenuCategories/EthicsStandards/CodeofEthicsforNurses/Code-of1.
- Texas Administrative Code, RULE §216.3 Continuing Competency Requirements. Available from URL: https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=T&app=9&p_dir=N&p_rloc=193277&p_tloc=&p_ploc=1&pg=85&p_tac=&ti=22&pt=11&ch=216&rl=3
- Texas Administrative Code, RULE §217.1 Nursing Jurisprudence Exam (NJE). Available from URL: https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=T&app=9&p_dir=P&p_rloc=123209&p_tloc=&p_ploc=1&pg=111&p_tac=&ti=22&pt=11&ch=216&rl=3
- Texas Administrative Code, RULE §217.11 Standards of Nursing Practice. Available from URL: https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=T&app=9&p_dir=N&p_rloc=113468&p_tloc=&p_ploc=1&pg=103&p_tac=&ti=22&pt=11&ch=216&rl=3
(Adopted: 07/2011) (Revised: 01/2013; 01/2016; 01/2018; 01/2019; 01/2020) (Reviewed: 01/2012; 01/2014; 01/2015; 01/2017) - Texas Administrative Code, RULE §217.12 Unprofessional Conduct. Available from URL: https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=T&app=9&p_dir=N&p_rloc=133132&p_tloc=&p_ploc=1&pg=104&p_tac=&ti=22&pt=11&ch=216&rl=3
- Texas Board of Nursing, Nursing Board Position Statements. Available from URL: https://www.bon.texas.gov/practice_bon_position_statements_content.asp#15.28
- Texas Board of Nursing, Professional Boundaries Including the Use of Social Media by Nurses. Available from URL: https://www.bon.texas.gov/practice_bon_position_statements_content.asp#15.28
- Texas Board of Nursing, Rule §213.33(b)-Texas Board of Nursing Disciplinary Matrix. Available from URL: https://www.bon.texas.gov/pdfs/disciplinaryaction_pdfs/discp-matrix.pdf
- Texas Board of Nursing, Texas Board of Nursing Position Statement. Available from URL: https://www.bon.texas.gov/pdfs/practice_dept_pdfs/position_statements_pdfs/15.28mar20.pdf
- Texas Board of Nursing, Texas Board of Nursing – Practice – Registered Nurse Scope of Practice. Available from URL: https://www.bon.texas.gov/practice_scope_of_practice_rn.asp.
- Texas Board of Nursing, The Registered Nurse Scope of Practice. Available from URL: https://www.bon.texas.gov/practice_bon_position_statements_content.asp#15.28
- Texas Board of Nursing Website, Available from URL: www.bon.texas.gov
Texas Nursing Forensics
- (2003) Institute on Domestic Violence and sexual assault. The University of Texas at Austin. A Health survey of Texans: A focus on Sexual Assault. Retrieved from: https://sites.utexas.edu/idvsa/?s=focus+on+sexual+assault
- (2015) The University of Texas. Stephen Hicks school of Social Work. HEALTH AND WELL-BEING: Texas Statewide Sexual Assault Prevalence Study Final Report. Retrieved from: https://sites.utexas.edu/idvsa/files/2019/03/TX-SA-Prevalence-Study-Final-Report.pdf
- (2015) National Alliance to End Sexual Violence. The Costs and Consequences of Sexual Violence and Cost-Effective Solutions. Retrieved from: https://endsexulavilolence.org/where_we_stand/costs-consequences-and-solutions
- (2021) Miller, Ted R; Cohen, Mark A; Wiersema, Brian; Victim Costs and Consequences: A New Look. National Institutes of Justice Retrieved from: https://www.ojp.gov/pdffiles/victcost.pdf
- Office of Justice Programs. Office of Victims of Crime. SANE Program Development and Operation Guide. Retrieved from: https://www.ovcttac.gov/saneguide/introduction/what-is-a-sane?
- Prescott Valley, Arizona official government site. Retrieved from: https://www.pvaz.net/DocumentCenter/View/8943/Common-Feelings-of-Survivors-of-Sexual-Assault
- RAINN articles: What is a SANE/SART? Retrieved from: https://www.rainn.org/articles/what-sanesart
- Texas A&M, College of Nursing, et al. Texas Attorney General Sexual Assault Prevention and Crisis Services Program. TEXAS EVIDENCE COLLECTION PROTOCOL Retrieved from: https://nursing.tamu.edu/documents/txecp-final-08212019.pdf
- Texas Legislature Online. Evidence Collection Protocol Kits. Retrieved from: https://statutes.capitol.texas.gov/Docs/GV/htm/GV.420.htm
- (2021) RAINN state database, Texas. Understanding Statute of Limitations of Sex Crimes. Retrieved from: https://apps.rainn.org/policy/policy-crime-definitions.cfm?state=Texas&group=7
- RAINN. Stat Pearls. What is a Sexual Assault Forensic Exam? Retrieved from: https://rainn.org/articles/rape-kit 3/2/2021
- (2020) Slate, Melissa, RN, BA, MA, Forensic Evidence Collection for Nurses. Retrieved from: https://Rn.org/courses/coursematerial-173.pdf
- (2018) Emergency Nurses Association. Position Statement: Forensic Evidence in the Emergency Care Setting. Retrieved from: https://www.ena.org/docs/default-source/resource-library/practice-resources/position-statements/forensic-evidence-collection-in-the-emergency-care-setting.pdf?sfvrsn=a1f89eba_6
- RAINN articles. Copyright 2021. StatPearls Publishing, LLC Bookshelf ID: NBK448154, PMID: 28846356. What is a sexual assault Forensic Exam? Retrieved from: https://rainn.org/articles/rape-kit
- Attorney General of Texas. Resources for Crime Victims. Retrieved from: https://www.texasattorneygeneral.gov/crime-victims/services-crime-victims/resources-crime-victims
End of Life Care for Geriatric Patients
- HTTPS://www.ajmc.com/contributor/sophia-bernazzani/2016/03/guide-to-end-of-life-care-options
- https://www.mayoclinic.org/healthy-lifestyle/end-of-life/basics/endoflife-care/hlv-20049403
- https://bjgp.org/content/63/615/e657.short
- https://search.proquest.com/openview/1d8060f340f99043a9ebf343b06d498f/1?pq-origsite=gscholar&cbl=33078
- https://journals.sagepub.com/doi/full/10.1177/0269216314526272
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3241064/
- https://www.nursingworld.org/~4af078/globalassets/docs/ana/ethics/endoflife-positionstatement.pdf
- https://www.aacn.org/clinical-resources/palliative-end-of-life
- https://medlineplus.gov/ency/patientinstructions/000473.htm
- https://www.aafp.org/fpm/2008/0300/p18.html
- https://www.ama-assn.org/delivering-care/ethics/medically-ineffective-interventions
- https://insights.ovid.com/article/01256961-200710000-00013
- https://www.cancer.gov/publications/dictionaries/cancer-terms/def/end-of-life-care
Alzheimer’s Nursing Care
- Alzheimer’s disease fact sheet. (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet
- Preventing Alzheimer’s disease: What do we know? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/preventing-alzheimers-disease-what-do-we-know
- How is Alzheimer’s disease treated? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/how-alzheimers-disease-treated
- Behavior changes and communication in Alzheimer’s. (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/topics/behavior-changes-and-communication-alzheimers
- How is Alzheimer’s disease diagnosed? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/how-alzheimers-disease-diagnosed
Nursing Care for Pediatric Patients by Stage of Development
- Karlsson, K., Rydstrom, I., Enskar, K., & Englund, A.D. (2014). Nurses’ perspectives on supporting children during needle-related medical procedures. International Journal of Qualitative Studies on Health and Well Being, 9.doi:10.3402/qhw.v9.23063
- Wagner, R. (2019). Flip It. Devereux Advanced Behavioral Health. https://centerforresilientchildren.org/
- U.S. Department of Health and Human Services. (2017). National Center for Health Statistic summary health statistics: National Health interview survey. Centers for Disease Control and Prevention. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NH/SHS/2017_SHS_Table_P- 10.pdf
- Fostering Resilience. (n.d.). The 7 Cs: The Essential Building Block of Resilience. http://www.fosteringresilience.com
- Tubbs-Cooley, H.L., Mara, C.A., Carle, A.C., Mark, B.A., & Pickler, R.H. (2019). Association of nurse workload with missed nursing care in the neonatal intensive care unit. Journal of American Medical Association Pediatrics, 173(1), 44–51. doi:10.1001/jamapediatrics.2018.3619
- Hockenberry, M. J., Rodgers, C. C., & Wilson, D. (2017). Wong’s essentials of pediatric nursing, (10th ed.). St. Louis, Missouri: Elsevier Mosby.
- Hasenfuss, E. (2003). Collaboration of nursing and child life: A palette of professional practice. Journal of Pediatric Nursing, 18(5), 359-365. https://doi.org/10.1016/S0882-5963(03)00158-1
- Hurley, K. (2018). 10 things never to say to your anxious child. https://www.psycom.net/child-anxiety
- Ball, J.W., Bindler, R.C., Cowen, K.J., & Shaw, M. R. (2016). Principles of pediatric nursing: Caring for children, (7th ed.). Hoboken, NJ: Pearson Education.
- Hudson, N., Spriggs, M., & Gillam, L. (2019). Telling the truth to young children: Ethical reasons for information disclosure in paediatrics. Journal of Paediatrics and Child Health, 55, 13-17. doi: 10.1111/jpc.14209
- Fastaff. (2015). Pediatric nurse: A crash course in talking to kids. https://www.fastaff.com/blog/pediatric-nurse-crash-course-talking-kids
- Hurley, K. (2018). Resilience in children: Strategies to strengthen your kids. https://www.psycom.net/build-resilience-children
- Filion, J. (2016). 3 types of pediatric therapy to consider. https://www.gebauer.com
- Thrane, S.E., Wanless, S., Cohen, S. M., & Danford, C. A. (2016). The assessment and non-pharmacologic treatment of procedural pain from infancy to school age through a developmental lens: A synthesis of evidence with recommendations (review). Journal of Pediatric Nursing, 31(1), e23-e32. doi:10.1016/j.pedn.2015.09.002
- Moadad, N., Kozman, K., Shahine, R., Ohanian, S., & Badr, L.K. (2016). Distraction using the Buzzy for children during an IV insertion. Journal of Pediatric Nursing, 31(1), 64-72. doi:10.1016/j.pedn.2015.07.010
- Nilsson, S., Enskar, K., Hallqvist, C., & Kokinsky, E. (2013). Active and passive distraction in children undergoing wound dressings. Journal of Pediatric Nursing, 28 (2), 158-166. doi.10.1016/j.pedn.2012.06.003
- Coleman, C.L. & Ahmann, E. (2016). Family matters. Empowered by nurses. Pediatric Nursing 42(4), 193-196.
- Ford, K., & Turner, D. (2008). Stories seldom told: Paediatric nurses’ experiences of caring for hospitalized children with special needs and their families. Journal of Advanced Nursing, 288-295.
- https://doi.org/10.1046/j.1365-2648.2001.01678.x
Opioid Abuse
- https://www.deamuseum.org/ccp/opium/history.html
- https://americanaddictioncenters.org/opiates/controlled-substances
- https://www.cdc.gov/injury/features/prescription-drug-overdose/index.html
- https://www.cdc.gov/drugoverdose/prescribing/guideline.html
- https://www.cdc.gov/drugoverdose/pdf/guidelines_at-a-glance-a.pdf
- https://www.cdc.gov/drugoverdose/pdf/pdo_checklist-a.pdf
- APA Webster, Lynn R. MD Risk Factors for Opioid-Use Disorder and Overdose, Anesthesia & Analgesia: November 2017 – Volume 125 – Issue 5 – p 1741-1748 doi: 10.1213/ANE.0000000000002496
- Andrea L. Nicol, Robert W. Hurley, Honorio T. Benzon Anesth Analg. Author manuscript; available in PMC 2018 Nov 1. Published in final edited form as: Anesth Analg. 2017 Nov; 125(5): 1682–1703. doi: 10.1213/ANE.0000000000002426
- Mart van Laar, Joseph V Pergolizzi, Jr, Hans-Ulrich Mellinghoff, Ignacio Morón Merchante, Srinivas Nalamachu, Joanne O’Brien, Serge Perrot, Robert B Raffa
- Open Rheumatol J. 2012; 6: 320–330. Published online 2012 Dec 13. doi: 10.2174/1874312901206010320
- Pak, S. C., Micalos, P. S., Maria, S. J., & Lord, B. (2015). Nonpharmacological interventions for pain management in paramedicine and the emergency setting: a review of the literature. Evidence-based complementary and alternative medicine: eCAM, 2015, 873039. https://doi.org/10.1155/2015/873039
- Safer D. J. (2019). Overprescribed Medications for US Adults: Four Major Examples. Journal of clinical medicine research, 11(9), 617–622. https://doi.org/10.14740/jocmr3906
- Dydyk AM, Jain NK, Gupta M. Opioid Use Disorder. [Updated 2020 Jun 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553166/
- https://www.cdc.gov/drugoverdose/training/oud/accessible/index.html
Vaping Induced Lung Injuries
- Centers for Disease Control and Prevention. (2019). Electronic cigarettes. Retrieved from: https://www.cdc.gov/tobacco/basic_information/e-cigarettes/index.htm
- Centers for Disease Control and Prevention. (2019). Smoking and tobacco use: for healthcare providers. Retrieved from: https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease/healthcare-providers/index.html
- Chatham-Stephens, K, et al. (2019). Characteristics of hospitalized and non-hospitalized patients in a nationwide outbreak of e-cigarette, or vaping, product use-associated lung injury. Morbidity Mortality Weekly, 68(1076-1080). Retrieved from: https://www.cdc.gov/mmwr/volumes/68/wr/mm6846e1.htm?s_cid=mm6846e1_w
- Dinikar, C. & O’Connor, G. T. (2016). The health effects of electronic cigarettes. The New England Journal of Medicine, 375 (1372-1381). Retrieved from: https://www.nejm.org/doi/full/10.1056/NEJMra1502466
- Halpern, S. D., et al. (2018). A pragmatic trial of e-cigarettes, incentives, and drugs for smoking cessation. The New England Journal of Medicine, 378(2302-2310). Retrieved from: https://www.nejm.org/doi/full/10.1056/NEJMsa1715757
- Martinelli, K. (2018). Teen vaping: What you need to know. Child Mind Institute. Retrieved from: https://childmind.org/article/teen-vaping-what-you-need-to-know/
- Rubinstein, M. L., et al. (2018). Adolescent exposure to toxic volatile organic chemicals from e-cigarettes. Pediatrics, 141(4). Retrieved from: https://pediatrics.aappublications.org/content/141/4/e20173557
- U.S. Department of Health and Human Services. (2016). E-cigarette use among youth and young adults: a report of the Surgeon General. Retrieved from: https://e-cigarettes.surgeongeneral.gov/documents/2016_SGR_Full_Report_non-508.pdf
LGBTQ Cultural Competence
- Waisel DB. Vulnerable populations in healthcare. Curr Opin Anesthesiol. 2013;26(2):186–92.
- Freid VM, Bernstein AB, Bush MA. Multiple chronic conditions among adults aged 45 and over: Trends over the past 10 years. NCHS Data Brief. 2012;2012(100):1–8.
- Institute of Medicine. Collecting sexual orientation and gender identity data in electronic health records: workshop summary. Washington DC: National Academy of Sciences; 2013.
- Quinn GP, Sanchez JA, Sutton SK, Vadaparampil ST, Nguyen GT, Green BL, et al. Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA-Cancer J Clin. 2015;65(5):384–400
- Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health. 2010;100(10):1953–60.
- Dilley JA, Simmons KW, Boysun MJ, Pizacani BA, Stark MJ. Demonstrating the importance and feasibility of including sexual orientation in public health surveys: health disparities in the Pacific northwest. Am J Public Health. 2010;100(3):460–7.
- Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay, and bisexual older adults: results from a population-based study. Am J Public Health. 2013;103(10):1802–9.
- Bauermeister J, Eaton L, Stephenson R. A multilevel analysis of neighborhood socioeconomic disadvantage and transactional sex with casual partners among young men who have sex with men living in metro Detroit. Behav Med. 2016;42(3):197–204.
- Smalley KB, Warren JC, Barefoot KN. Differences in health risk behaviors across understudied LGBT subgroups. Health Psychol. 2016;35(2):103–14.
- Staats C, Capatosto K, Wright RA, Jackson VW. State of the science: Implicit bias review 2016. Columbus: Kirwan Institute.
- Cochran SD, Bandiera FC, Mays VM. Sexual orientation-related differences in tobacco use and secondhand smoke exposure among US adults aged 20 to 59 years: 2003-2010 National Health and nutrition examination surveys. Am J Public Health. 2013;103(10):1837–44.
- Remafedi G, French S, Story M, Resnick MD, Blum R. The relationship between suicide risk and sexual orientation: results of a population-based study. Am J Public Health. 1998;88(1):57–60.
- Charlton BM, Corliss HL, Missmer SA, Frazier AL, Rosario M, Kahn JA, et al. Reproductive health screening disparities and sexual orientation in a cohort study of U.S. adolescent and young adult females. J Adolesc Health. 2011;49(5):505–10.
- Matthews AK, Brandenburg DL, Johnson TP, Hughes TL. Correlates of underutilization of gynecological cancer screening among lesbian and heterosexual women. Prev Med. 2004;38(1):105–13.
- Tracy JK, Lydecker AD, Ireland L. Barriers to cervical Cancer screening among lesbians. J Women’s Health. 2010;19(2):229–37.
- Grossman AH, D’Augelli AR. Transgender youth: invisible and vulnerable. J Homosex. 2006;51(1):111–28.
- Krehely J. How to close the LGBT health disparities gap. Center for American Progress; 2009. p. 1–9.
- Buchmueller T, Carpenter CS. Disparities in health insurance coverage, access, and outcomes for individuals in same-sex versus different-sex relationships, 2000-2007. Am J Public Health. 2010;100(3):489–95.
- Heck JE, Sell RL, Gorin SS. Health care access among individuals involved in same-sex relationships. Am J Public Health. 2006;96(6):1111–8.
- Kamen C, Palesh O, Gerry AA, Andrykowski MA, Heckler C, Mohile S, et al. Disparities in health risk behavior and psychological distress among gay versus heterosexual male Cancer survivors. LGBT Health. 2014;1(2):86–U103.
- Legal L. When health care Isn’t caring: lambda Legal’s survey of discrimination against LGBT people and people with HIV. New York: Lamba Legal; 2010.
- Grant JM, Mottet LA, Tanis J. National Transgender Discrimination Survey Report on health and health care. Washington DC: National Center for Transgender Equality and National Gay and Lesbian Task Force; 2010.
- Shires DA, Jaffee K. Factors associated with health care discrimination experiences among a National Sample of female-to-male transgender individuals. Health Soc Work. 2015;40(2):134–41.
- Eliason MJ, Dibble SL, Robertson PA. Lesbian, gay, bisexual, and transgender (LGBT) physicians’ experiences in the workplace. J Homosex. 2011;58(10):1355–71.
- Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25(6):445–54.
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8.
- Mereish EH, Bradford JB. Intersecting identities and substance use problems: sexual orientation, gender, race, and lifetime substance use problems. J Stud Alcohol Drugs. 2014;75(1):179–88.
- Torres CG, Renfrew M, Kenst K, Tan-McGrory A, Betancourt JR, Lopez L. Improving transgender health by building safe clinical environments that promote existing resilience: results from a qualitative analysis of providers. BMC Pediatr. 2015; 15:187.
- Burke SE, Dovidio JF, Przedworski JM, Hardeman RR, Perry SP, Phelan SM, et al. Do contact and empathy mitigate Bias against gay and lesbian people among heterosexual first-year medical students? A report from the medical student CHANGE study. Acad Med. 2015;90(5):645–51.
- Sabin JA, Riskind RG, Nosek BA. Health care Providers’ implicit and explicit attitudes toward lesbian women and gay men. Am J Public Health. 2015;105(9):1831–41.
- Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882–7.
- Wilson TD, Brekke N. Mental contamination and mental correction: unwanted influences on judgments and evaluation. Psychol Bull. 1994;116(1):117–42.
- Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit Bias in health care: a narrative review. Group Process Interg. 2016;19(4):528–42.
- Greenwald AG, Banaji MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychol Rev. 1995;102(1):4–27.
- Van Ryn M, Saha S. Exploring unconscious bias in disparities research and medical education. JAMA. 2011;306(9):995–6.
- Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998;74(6):1464–80.
- Nosek BA, Riskind RG. Policy implications of implicit social cognition. Soc Issue Policy Rev. 2012;6(1):113–47.
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
- Shavers VL, Fagan P, Jones D, Klein WMP, Boyington J, Moten C, et al. The state of research on racial/ethnic discrimination in the receipt of health care. Am J Public Health. 2012;102(5):953–66.
- Chapman EN, Kaatz A, Carnes M. Physicians and implicit Bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28(11):1504–10.
- Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment: Confronting racial and ethnic disparities in health care. Brian D. Smedley, Adrienne Y. Stith, and Alan R. Nelson, Editors; Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care; Board on Health Sciences Policy; Institute of Medicine. Washington, DC; 2003.
- Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41.
- Greenwald AG, Banaji MR, Nosek BA. Statistically small effects of the implicit association test can have societally large effects. J Pers Soc Psychol. 2015;108(4):553–61.
- Khan A, Plummer D, Hussain R, Minichiello V. Does physician bias affect the quality of care they deliver? Evidence in the care of sexually transmitted infections. Sex Transm Infect. 2008;84(2):150–1.
- Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P. (2019). Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC medical education, 19(1), 325. https://doi.org/10.1186/s12909-019-1727-3
- Human rights campaigns. Glossary of terms. Retrieved from https://www.hrc.org/resources/glossary-of-terms
- Advancing Effective Communication, Cultural Competence, and Patient– and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community, a field guide. Joint Commission. Retrieved from https://www.jointcommission.org/ /media/enterprise/tjc/imported-resource assets/documents/lgbtfieldguide_web_linked_verpdf.pdf?db=web hash=1EC363A65C710BCD1D4E14ED120CB2
- Delivering culturally sensitive care to LGBTQI Patients. The Journal for nurse practitioners. Volume 13, issue 5 p342-347.
Coronavirus: Nursing Considerations
- COVID-19 overview and infection prevention and Control priorities in non-us HEALTHCARE SETTINGS. (n.d.). Retrieved February 25, 2021, from https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/overview/index.html#background
- Commissioner, O. (n.d.). A Closer Look at COVID-19 Diagnostic Testing. Retrieved January 05, 2021, from https://www.fda.gov/health-professionals/closer-look-covid-19-diagnostic-testing
- Overview of Testing for SARS-CoV-2 (COVID-19). (n.d.). Retrieved January 05, 2021, from https://www.cdc.gov/coronavirus/2019-ncov/hcp/testing-overview.html
- Watson, J., Whiting, P. F., & Brush, J. E. (2020). Interpreting a covid-19 test result. Bmj, M1808. doi:10.1136/bmj.m1808
- Cascella M, Rajnik M, Cuomo A, et al. Features, Evaluation, and Treatment of Coronavirus. [Updated 2020 Oct 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554776/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7369540/
- Long-Term Effects of COVID-19. (n.d.). Retrieved January 11, 2021, from https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html
- J. (2020, December 28). A New Strain of Coronavirus: What You Should Know. Retrieved January 11, 2021, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/a-new-strain-of-coronavirus-what-you-should-know
- Dhont, S., Derom, E., Braeckel, E., Depuydt, P., & Lambrecht, B. (n.d.). The pathophysiology of ‘happy’ hypoxemia in COVID-19. Retrieved January 14, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7385717/
Effective Communication in Nursing
- Dictionary by Merriam-Webster: America’s most-trusted online dictionary. (n.d.). Retrieved February 22, 2021, from https://www.merriam-webster.com/
- Effects of poor communication in healthcare. (n.d.). Retrieved February 22, 2021, from https://www.hipaajournal.com/effects-of-poor-communication-in-healthcare/?amp
Nursing Documentation 101
- 29-1141 Registered Nurses. (2018, March 30). Retrieved March 1, 2019, from https://www.bls.gov/oes/2017/may/oes291141.htm
- Hendrich, A., Chow, M. P., Skierczynski, B. A., & Lu, Z. (2008). A 36-hospital time and motion study: how do medical-surgical nurses spend their time? The Permanente journal, 12(3), 25-34.
- Health IT Quick Stats. (2019, February 6). Retrieved March 1, 2019, from https://dashboard.healthit.gov/quickstats/quickstats.php
- Medical Practice Efficiencies & Cost Savings. (2018, August 13). Retrieved March 1, 2019, from https://www.healthit.gov/topic/health-it-and-health-information-exchange-basics/medical-practice-efficiencies-cost-savings
- Meaningful Use. (2017, January 18). Retrieved March 1, 2019, from https://www.cdc.gov/ehrmeaningfuluse/introduction.html
- Miller, L., Stimely, M., Matheny, P., Pope, M., McAtee, R. & Miller, K. Novice Nurse Preparedness to Effectively Use Electronic Health Records in Acute Care Settings: Critical Informatics Knowledge and Skill Gaps. (2014). Online Journal of Nursing Informatics,18(2). Retrieved March 1, 2019, from https://www.himss.org/novice-nurse-preparedness-effectively-use-electronic-health-records-acute-care-settings-critical
- HHS Office of the Secretary,Health Information Privacy Division. (2016, February 25). Individuals’ Right under HIPAA to Access their Health Information. Retrieved March 1, 2019, from https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/access/index.html
- Office for Civil Rights (OCR). (2015, December 18). 2000-Why is the HIPAA Security Rule needed and what is the purpose of the security standards. Retrieved March 1, 2019, from https://www.hhs.gov/hipaa/for-professionals/faq/2000/why-is-hipaa-needed-and-what-is-the-purpose-of-security-standards/index.html
- AHIMA Work Group (2013). Integrity of the Healthcare Record: Best Practices for EHR Documentation (2013 update). Journal of AHIMA,84(8), 58-62. Retrieved March 1, 2019, from http://library.ahima.org/doc?oid=300257#.XHuU6YhKiUl
- What is Malpractice? (n.d.). Retrieved from https://www.abpla.org/what-is-malpractice#medical
- Cady, R. F., Esq. (2009). Criminal Prosecution for Nursing Errors. JONA’s Healthcare Law, Ethics, and Regulation,11(1), 10-16. Retrieved March 1, 2019, from https://www.nursingcenter.com/cearticle?an=00128488-200901000-00003&Journal_ID=260876&Issue_ID=848807
- Kann, B. R., Beck, D. E., Margolin, D. A., Vargas, D., & Whitlow, C. B. (Eds.). (2018). Improving Outcomes in Colon & Rectal Surgery. Retrieved March 1, 2019, from https://www.books.google.com/books?id=O61vDwAAQBAJ&dq=
- Improving Outcomes in Colon & Rectal Surgery edited by Brian R. Kann, David E. Beck, David A. Margolin, H. David Vargas, Charles B. Whitlow&source=gbs_navlinks_s
- Peters, P. G. (2008). Twenty Years of Evidence on the Outcomes of Malpractice Claims. Clinical Orthopaedics and Related Research, 467(2), 352-357. doi:10.1007/s11999-008-0631-7
- Singh, H. (2018). National Practitioner Data Bank Generated Data Analysis Tool. Retrieved March 1, 2019, from https://www.npdb.hrsa.gov/analysistool/
- Top 5 Malpractice Claims Made Against Nursing Professionals. (n.d.). Retrieved March 1, 2019, from https://www.proliability.com/portals/0/docs/nursemalpracticewhitepaper.pdf
- American Nurses Association. (2010). ANA’s Principles for Nursing Documentation. Retrieved February 28, 2019, from https://www.nursingworld.org/~4af4f2/globalassets/docs/ana/ethics/principles-of-nursing-documentation.pdf
- Lippincott Nursing Education. (2018, February 22). Lippincott Nursing Education Blog. Retrieved March 1, 2019, from http://nursingeducation.lww.com/blog.entry.html/2018/02/22/nursing_documentatio-S5hF.html
- Reising, D. L., & Allen, P. N. (February 2007). Protecting yourself from malpractice claims. American Nurse Today,2(2). Retrieved March 1, 2019, from https://www.americannursetoday.com/protecting-yourself-from-malpractice-claims/.
- Reising, D. L. (2012). Make your nursing care malpractice-proof. American Nurse Today,7(1). Retrieved March 1, 2019, from https://www.americannursetoday.com/make-your-nursing-care-malpractice-proof/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate

