Course
2021 Michigan Renewal Bundle
Course Highlights
- In this course we will learn about Opioid abuse, cultural competence, nursing ethics, and more!
- You’ll also learn the basics of Human Trafficking and Pain Management, as required by the Michigan Board of Nursing.
- You’ll leave this course with a broader understanding of nursing documentation, patient confidentiality, and nurse turnover.
About
Contact Hours Awarded: 25.5
Course By:
Multiple Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
This 2021 Michigan License Renewal Bundle meets all renewal requirements for Michigan LPNs and RNs. Upon completion of this course, you will receive a certificate of completion for 25.5 contact hours.
This course features multiple interesting topics in one easy course and includes the required Human Trafficking and Pain and Symptom Management Courses.
Course Outline
- Human Trafficking – Michigan
- Michigan Pain and Symptom Management for Nurses
- Opioid Abuse
- Vaping Induced Lung Injuries
- LGBTQ Cultural Competence
- Coronavirus: Nursing Considerations
- Effective Communication in Nursing
- Flu Treatment, Symptoms, and Red Flags
- Nursing Documentation 101
- End of Life Process
- Alzheimer’s Nursing Care
- PTSD in Nursing
- Nursing Ethics
- Ensuring Patient Confidentiality in Nursing
- A Nurse’s Guide: How to Deal with Difficult Patients
- How to Reduce New Nurse Turnover
- References
Human Trafficking – Michigan
Prevalence and Definition
The Polaris Project estimates that collectively there are over 25 million victims of human trafficking worldwide. These are individuals that have been forced into sexual or labor servitude. Of those, several hundred thousand are estimated to be in the United States (1). It is very difficult to estimate accurately as so often this is a crime that is unseen and hidden from the public eye. In 2019, there were 932 contacts made concerning human trafficking reported within Michigan to the National Human Trafficking Hotline via telephone calls, texts, or online submissions. This ranks Michigan at number six within the top ten of human trafficking hot spots of the U.S. (1). 364 cases were reported and 184 of the calls for help came from the victims themselves (2). These numbers exemplify the number of potential victims that are not reaching out for help.
Often, when human trafficking is discussed, a common misconception is that it is simply the transporting of humans. Human trafficking covers a much broader scope than this. It is this a modern age form of slavery and involves the exploitation of individuals for monetary or sexual gain. As stated by the Department of Homeland Security, “Human trafficking involves the use of force, fraud, or coercion to obtain some type of labor or commercial sex act” (3).
As defined by U.S. law, there are three categories of human trafficking (all from 1):
- Children under the age of 18 induced into commercial sex
- Adults (age 18 or over) induced into commercial sex through force, fraud, or coercion
- Children and adults induced to perform labor or services through force, fraud, or coercion
The majority of trafficking in the United States involves sex crimes, followed by labor (4). These crimes may be occurring simultaneously to the same victim. Types of trafficking can include forced prostitution, pornography, strip dancing, criminal enterprise and bonded labor in domestic servitude or migrant work. Outside of street prostitution, sex trafficking is most likely to be occurring in venues such as strip clubs, massage parlors, or other fictitious business fronts for prostitution. A major difference with sex trafficking of minors is that, unlike adults, force, coercion, or fraud does not need to be present for prosecution (6). As there are several different avenues for and types of human trafficking, recognition can be challenging
Risk Factors
The profile of the human trafficking victim is not easy to define. Victims of human trafficking come from varied backgrounds that may or may not be what is expected or stereotypical. Victims may come from any race, socioeconomic status, color, religion, age, gender, sexual orientation, or gender identity, and on. The main commonality is that there is a layer of deception whereby the human trafficker is targeting a vulnerability in the victim. As stated by the Department of Justice, trafficking victims are deceived with “. . . false promises of love, a good job, or a stable life and are lured into situations where they are made to work in deplorable conditions with little or no pay” (5). There are some trends noted that do make certain populations more at risk, but keep in mind that this does not encompass all potential victims and vigilance should be taken to avoid assumptions.
The risk factors for human trafficking are just as varied and dependent upon the type of trafficking and method by which the abuser is able to hold the victim indentured or captive. This figurative prison may be physically, emotionally, or monetarily induced. The Center for Disease Control and Prevention (CDC) lists the following characteristics and factors:
- Many victims are women and girls, though men and boys are also impacted
- Victims include all races, ethnicities, sexual orientations, gender identifies, citizens, non-citizens, and income levels
- Victims are trapped and controlled through assault, threat, false promises, perceived sense of protection, isolation, shaming, and debt
Several higher risk populations have been identified through the data gathered from the Polaris Project. It was found that children who were or had been within the foster care system or runaway homeless youth were more likely to encounter sexual victimization. Other factors include substance abuse, recent relocation or migration, unstable housing situations, and underlying mental health disorders (7).
As a population that is often overlooked, shamed, or lacks resources, members of the lesbian, gay, bisexual, transgender, queer, or questions (LGBTQ) community are more vulnerable to being subject to human trafficking. Up to 40% of homeless youth are part of the LGBTQ community and may not seek assistance for fear of being shunned (8).
Illegal and sponsored immigration remains at a higher risk of trafficking and exploitation. The NHRTC reports a significant number of calls that reference foreign nationals (2). Individuals wishing to become American citizens are lured with the promise of freedom in exchange for large fees that are made impossible to be worked off. While there are laws in place to prevent, this type of servant bondage is forced upon the victims who are in a new country and often lack resources or are unable to seek assistance due to cultural, language, and accessibility barriers. Further, cases have been reported where the employer or trafficker withhold visas or identification barriers in order promote compliance and are essentially holding the victim hostage (9).
Recruitment Techniques
A major tactic of the perpetrators of these crimes is to prey on vulnerable individuals with a lack of resources. Thus, a primary ploy used is a layer of deception whereby the human trafficker is targeting the needs or wants of the victim.
Traffickers are often individuals that the victim has come to trust. This may be a girlfriend or boyfriend, spouse, or other family member. Victims are also commonly sold to outside parties.
In cases of sexual trafficking, typically young women and men are groomed and given preferential treatment, gifts, and drugs until they become reliant upon the “John.” In other cases, individuals are tempted with the promise of a better life, or in the case of immigration, sponsorship for a visa (9).
Michigan and Federal Laws
In 2006, Michigan joined 26 other states in establishing a statute banning human trafficking. Today, there are 39 states that have committed to this crusade. The bill defined and prohibited the following:
- Forced Labor or Services MCL 750.462b
- “Labor” means work of economic or financial value.
- “Services” means an ongoing relationship between a person and an individual in which the individual performs activities under the supervision of or for the benefit of the person, including, but not limited to commercial sexual activity and sexually explicit performances.
- Debt Bondage MCL750.462c
- Enterprise Liability; Financially Benefitting MCL 750.462d
- Trafficking a Minor MCL 750.462e
- Covers both sex trafficking and labor trafficking of a minor
- NO Force Fraud or Coercion Required
- “regardless of whether the person knows the age of the minor” (10)
The bill was amended in 2010 to give victims the opportunity to seek damages that were due to bondage, suffering, and loss of quality of life in addition to any related medical costs incurred (10).
In 2014, Michigan legislation further bolstered the State’s position in the battle on human trafficking. Mandatory training for medical professionals was made a requirement of maintaining licensure. The Human Trafficking Commission and the Human Trafficking Health Advisory Board were created to track progress, garner funds through grants, and provide a means of connecting local government and non-government agencies access to resources and funding (11).
Safe Harbor provisions were put into law that protect minors from prostitution charges, classifies minors found in prostitution to be human trafficking victims, and mandates that referrals are made to Child Protective Services (CPS) for mandatory investigation. Several changes were made to adult prostitution charges if it is found to be in relation to a sex trafficking ring with the goal of protecting victims of sex trafficking crimes rather than punishing (11).
A specific U.S. Federal law addressing trafficking crimes was first enacted with the Trafficking Victims Protection Act of 2000. The bill has since been revised several times; however, the fundamental of it is to provide guidance and authorization for their “three-pronged approach that includes prevention, protection, and prosecution” and covers both sex and labor trafficking (12).
Preventing Sex Trafficking and Strengthening Families Act of 2014 and The Justice for Victims of Trafficking Act of 2015 are both aimed at providing victims increased protection for exploitation and increased resources specifically aimed at prevention and support for child and youth sex trafficking crimes (12).
Mandatory Reporting in Michigan
Nurses in Michigan are classified as mandatory reporters for cases of suspected child abuse or neglect. Suspected human trafficking of a minor would fall under this category. Either a verbal or online report must be given to Centralized Intake (CI) at the Department of Health and Human Services. CI can be reached 24 hours a day by telephone at 1-855-444-3911 or register to submit an online report at https://newmibridges.michigan.gov/ under the Partnerships tab (13). If calling the hotline, a DHS-3200 form must be faxed or emailed within 72 hours of the initial report to CI. Online reporting eliminates the need to complete this form.
The following states the criminal and civil liability of failing to follow the law as a mandatory reporter:
In a civil action, the mandated reporter may be held liable for all damages that any person suffers due to the mandated reporters’ failure to file a report. In a criminal action, the mandated reporter may be found guilty of a misdemeanor punishable by imprisonment for up to 93 days and a fine of $500.
A person making a good faith report is protected from civil and criminal prosecution and cannot be penalized for making the report or cooperating with a CPS investigation (13).
Reporting of suspected adult human trafficking is not as clear regarding mandatory reporting. However, vulnerable adults suspected of being abused, exploited, or victimized fall under the same guidelines and are reported to CI in the same manner as above. Vulnerable adults in Michigan are defined as “A condition in which an adult is unable to protect himself or herself from abuse, neglect, or exploitation because of a mental or physical impairment or advanced age” (13).
Recognizing Signs of Human Trafficking
According to the Department of Health and Human Services, close 90% of human trafficking victims visit a health care facility at least once while in servitude and are not identified as such by health care providers (14). This is due to a lack of education, lack of consistent use of identification and screening tools, and time constraints within the current health care system. As a mandatory reporter and healthcare team member, it is imperative to use best practice in recognizing the signs and symptoms as well as the tools that are available.
Signs and Symptoms
Human trafficking victims may present to a healthcare setting with primary or underlying signs that may be related to physical or mental abuse. These signs and symptoms may be related to the reason that they are seeking treatment or may be identified by the healthcare provider during a thorough assessment. The following physical and psychological sequelae may be noted during an assessment as potential evidence of victimization (all derived from 9, 15):
Physical
- Unexplained or implausible injuries
- Bruising
- Wounds and Cuts
- Missing or broken teeth
- Closed head injuries
- Blunt force trauma
Neurological
- Headaches
- Migraines
- Memory loss or difficulty concentrating
- Vertigo
- Insomnia
- Brain trauma
Gastrointestinal
- Diarrhea
- Constipation
Dietary
- Malnutrition
- Anorexia
- Severe weight loss
Cardiovascular and Respiratory
- Tachyarrhythmias
- Hypertension
- Respiratory distress
Reproductive System
- Sexually transmitted disease
- Vaginal and/or anal fissures
- Previous Abortions
Psychological
- Depression
- Suicidal Ideation
- Anxiety
- Self-harm including cutting or branding
- Drug and alcohol abuse
- PTSD Symptoms
- Regression
- Anger
- Dissociative and Depersonalization Tendencies
Red Flags and Indicators
There are several characteristics that should be kept in mind as red flags during the interview and assessment that may indicate potential trafficking. These include, but are not limited to (all derived from 9, 15, 16):
- Tattoos that indicate ownership, a number, or tracking system or are out of character/obscene
- Inappropriate clothing for climate
- Workplace violence or abuse
- Unsanitary living conditions
- Multiple families or people sharing a living space that is too small
- Shares living space with employer
- Is not in control of financial assets
- Refusal to speak alone with health professionals
- Accompanied by individual that refuses to allow patient to speak for themselves or be alone
- Prostitution under age 18
- Answers are scripted
- Answers are implausible or contraindicate
- Appears younger or older than stated age
Interview Tools and Techniques
Check with your facilities protocol for specific guidance on assessment and examination protocols for suspected abuse victims. There are also many scripted interviewing tools available online that assist with asking targeted questions. First, it is important to establish the patient’s safety and to gain trust.
Gaining trust can be difficult and conducting assessments and interviews should be completed in a non-threatening environment with an unbiased and non-judgmental tone. Creating a space that is quiet and will not be interrupted is important. This will ensure that the potential victim feels safe communicating and is not concerned that she or he will be overheard. Present your demeanor in a non-threatening manner, at eye level, and focus on being attentive with observant listening. Maintain respectful eye contact to convey interest and reflective listening. If taking notes during the interview is required, explain to the patient what will be documented and what it will be utilized for (17).
The National Human Trafficking Resource Center (NHTRC) offers a plethora of resources and scripted questions. The following are general questions on assessing if the individual is being forced into a situation and can be applied to any of the specific types of human trafficking (all from 17):
“Did someone control, supervise or monitor your work/your actions?”
“Was your communication ever restricted or monitored?”
“Were you able to access medical care?”
“Were you ever allowed to leave the place that you were living/working? Under what conditions?”
“Was your movement outside of your residence/workplace ever monitored or controlled?”
“What did you think would have happened if you left the situation? Was there ever a time when you wanted to leave, but felt that you couldn’t? What do you think would have happened if you left without telling anyone?”
“Did you feel that it was your only option to stay in the situation?”
“Did anyone ever force you to do something physically or sexually that you didn’t feel comfortable doing?”
“Were you ever physically abused (shoved, slapped, hit, kicked, scratched, punched, burned, etc.) by anyone?”
“Were you ever sexually abused (sexual assault/unwanted touching, rape, sexual exploitation, etc.) by anyone?”
“Did anyone ever introduce you to drugs, medications as a method of control?”
While screening tools provide a base for asking difficult questions, the NHTRC advises “Before screening, users should also be prepared to draw upon the expertise of local legal and medical staff and to refer identified trafficking victims to appropriate housing, health, and social services in their area . . . the tool is a complement to, not a substitute for, specialized training in human trafficking, good professional practice and victim-centered service” (17).
The NHTRC also provides a 24-hour national hotline that is able to guide health professionals through completing assessments and determining the next best steps to intervene or offer the victim assistance. This is a very beneficial resource; however, it must be understood that calling NHTRC does not fulfill the mandatory reporting requirement for Michigan and the Centralized Intake (CI) at the Department of Health and Human Services is the only means of legally fulfilling the reporting obligation.
Interventions and Collaboration
When presented with a suspected human trafficking victim, it is likely that the individual will not be alone. Maintaining safety and support for the patient may require separation from the suspected trafficker. While this may not be possible, an attempt should be made to bring the patient to a room or examination area unaccompanied.
Be conscious of any cultural preferences that may affect the patient. If there are language barriers preventing meaningful communication, enlist the assistance of a professional interpreter. This is especially vital in cases where the accompanying visitor or family is attempting to interpret for the patient and may be filtering the victim’s responses.
For patients that seek healthcare related to sexual abuse, a SANE assessment and rape kit should be obtained per facility protocol. With permission, patients should be tested for sexually transmitted infections including HIV, gonorrhea, UTIs, syphilis, and pubic lice, as well as a pregnancy test for females. Forced and coerced abortions are frequent among minor females in the sex industry (18).
Thorough documentation of the patient’s reported reason for visit, physical and neurological assessment including any trauma, bruising, wounds, affect, and pertinent statements should be noted in the patient’s electronic medical record.
Educate yourself on local resources and be able to provide assistance with finding access to healthcare, mental health, and rehabilitative resources that are available in the community. Victims may not want to take pamphlets with them that may be found, so providing locations or addresses of shelters or clinics with operating times may be a safer option.
Collaborate with the healthcare team, law enforcement, and social work for suspected child or vulnerable adult trafficking.
Mandatory reporting of suspected cases of child abuse or trafficking is not encumbered by HIPAA disclosure when reporting to authorities; however, when reporting suspected adult trafficking, disclosure and permission must be granted unless there is an imminent threat to the safety of the patient, or the patient has been identified as a vulnerable population. Thoroughly assess if the individual meets criteria as a vulnerable adult and proceed accordingly. If the adult does not meet criteria, permission must be gained to report.
If a competent adult does disclose that they are a trafficking victim, determine if the patient is in immediate, life-threatening danger. If so, follow facility protocol and encourage and support the patient in reporting to a law enforcement agency. If there is no immediate danger, supportive care and assistance should be provided. The patient should be informed of the options available for social services, reporting, and resources. Creation of a safety plan is highly recommended (15).
Prevention
Prevention of human trafficking requires public education, awareness, and knowing how to properly respond when faced with suspicions. The Blue Campaign is a strategy from the Department of Homeland Security to bring national awareness to the issue and provide specialized training to law enforcement and federal employees. Blue Campaign pamphlets and other materials are available at their website, www.dhs.gov/blue-campaign, for distribution.
The Center for Disease Control takes the stance that sex trafficking is preventable via community awareness and acknowledging exploitation when it does occur. They state “Strategies based on the best available evidence exist to prevent related forms of violence, and they may also reduce sex trafficking. States and communities can implement and evaluate efforts that:
- Encourage health behaviors in relationships
- Foster safe homes and neighborhoods
- Identify and address vulnerabilities during health care visits
- Reduce demand for commercial sex
- End business profits from trafficking-related transactions” (6).
One of the largest barriers to prevention in the healthcare system is the inability to recognize signs and symptoms. As cited above, a significant number of human trafficking victims have filtered in and out of healthcare systems without being recognized. This misses the opportunity to connect, provide resources, and offer further assistance. The NHTRC provides many resources for training within healthcare facilities and standardized forms and interviewing questions that may be tailored to individual situations and facility needs.
Resources
National Human Trafficking Resource Center
Call: 1-888-373-7888
SMS: 233733 (Befree) – Text “HELP” OR “INFO”
Online chat: humantraffickinghotline.org/chat
This network provides healthcare facilities and individuals with information and connections to over 3,200 referral contacts that will assist human trafficking victims. These contacts include low or no-cost legal services, law enforcement agencies, social services, and anti-trafficking organizations. Communication is enhanced as dialect is available in English, Spanish, and 200 other languages.
Michigan Department of Health and Human Services
Online: https://www.michigan.gov/mdhhs/
Call: 1-855-444-3911
The MDHHS provides resources for the public and healthcare workers to report suspect or witnessed abuse or neglect of minors, vulnerable adults, and victims of domestic violence. It also provides guidance for mandatory reporting obligations in Michigan.
Michigan Human Trafficking Task Force
Address: P.O. Box 811653 Lansing, MI 48917
Online: Welcome
Email: Jane P. White, Director [email protected]
Works with a wide expanse of agencies to collaborate on meeting the needs of victims, communities, and law enforcement through volunteer work, funding, training, and resource support.
HEAL (Health, Education, Advocacy, Linkage) Trafficking
Online: www.Healtrafficking.org
The HEAL Trafficking Direct Service Committee works to improve the clinical care for trafficked persons by providing opportunities for service providers to connect, access support, share information and promising practices, identify best practices, and expand the referral network.
National Center for Missing & Exploited Children
Address: 333 John Carlyle Suite 125 Alexandria, VA 22314-3175
24 Hour Call Center: 1-800-THE LOST (1-800-843-5678)
Online: http://www.missingkids.org/theissues/trafficking
Provides specialized technical assistance, analysis, and recovery services on cases involving child sex trafficking.
Michigan Pain and Symptom Management for Nurses
Epidemiology of Pain
Pain is a subjective, complicated symptom that afflicts every human at some point in their lives. Managing pain within healthcare settings is a challenge and must take into consideration patient-centered preferences, treatment goals, as well as guidelines and laws from governing bodies. For many years, opioids were the first line of defense against acute and chronic pain conditions. With the opioid crisis, this mindset has been required to change.
Due to an overabundance of prescribing opioids, the opioid related death toll has continued to rise. Not only has this fatal epidemic resulted in untimely deaths for many, but it is also estimated that “For every 1 prescription opioid death, there are 20 specialty substance abuse treatment admissions, 45 emergency department visits for nonmedical use and adverse events, 156 people with substance use disorder and dependence, and 533 people using the drugs nonmedically overall” (1). This public health crisis has resulted in the conviction of pharmaceutical companies that were behind the political stronghold monopoly on pain management in America. As a result, the Federal government has collaborated with The Institute of Medicine (IOM) and the Centers for Disease Control (CDC), among many other experts in the field, to develop a plan that protects the American public from unintended opioid use and promotes a multi-disciplined, multi-modal approach to combating pain in America.
Statistics
Pain is a widespread public health concern that reaches every corner within America. In a 2011 report titled, Relieving Pain in America: A Blueprint for Transforming, Care, Education, and Research, the IOM revealed that pain affects nearly 100 million Americans and nationally costs upwards of 635 billion each year (2). Of these numbers, over 25 million American adults report that they suffer from pain daily, while 23.4 state a significant amount of pain (3).
Researchers gathered data from 8,781 American adult participants regarding individual perceptions of their overall health, underlying illnesses, and pain experiences within the previous three months. This study ranked pain on a scale of categories from one through four, with one being the least amount of pain, and four being the highest level of pain. From this data, it is estimated that almost 40 million individuals ranked themselves as living with pain at a category three or four. Individuals in these categories were also found more likely to have an accompanying disability, access healthcare on a more frequent basis, and have an overall worse quality of health and life (3).
What is Pain and Why Does it Occur?
Merriam-Webster defines pain as “a localized or generalized unpleasant bodily sensation or complex of sensations that causes mild to severe physical discomfort and emotional distress and typically results from bodily disorder (such as injury or disease) (4)”.
Pain is the body’s defense to achieve a response against further damage from a perceived threatening stimulus. The brain perceives pain via specific pathways. Four stages of pain transmission occur: transduction, transmission, perception and modulation (5).
Receptors within afferent fibers are activated when a potential threatening stimulus occurs. This initiates three stages of pain perception. Initially, pain sensitivity is triggered. From there, signals follow a network of peripheral neural pathways towards the spinal cord. Within the spinal cord is the dorsal horn, which contains neurons that translate and relay information about the painful or irritating peripheral stimulus to the thalamus and cortex to elicit a protective response (5,6).
Pain can be further distinguished within two frameworks, chronic and acute, and by pain related conditions, such as inflammatory responses, nociceptive, and physiological dysfunctions.
Identifying Types of Pain
Pain is classified by three distinct types: nociceptive, inflammatory, and neuropathic. Following are general descriptions of the types of pain; however, it must be noted that these pains can overlay each other and be occurring simultaneously.
Nociceptive pain is that which is due to nerve impairment or injury and is the most common type of pain that occurs. It is sometimes noted as being central pain that is caused by repeated, potentially or harmful stimuli. The nociceptors activated in this type of pain are spread throughout the body within internal organs, bones, joints, and the integumentary system (6). Nociceptive pain is generally described as radicular, somatic, or visceral depending on the nerve involvement. Examples of nociceptive pain include the sensation from touching a hot object, a broken arm, or a paper cut at the initial time of injury. It may also describe pain caused by cancer, arthritic changes, and ischemic pain that is not originated from nerve injury.
Inflammatory pain is part of the cascade of sequelae that makes up the immunological defense to damage caused by heat, toxins, trauma, foreign substances, or infection. Neutrophils, along with prostaglandins, histamine, and other chemical mediators flood the location of injured tissues as a part of the bodies normal, inflammatory response. Classic signs include erythema, edema, and heat at the site of injury (6). Inflammatory pain can be seen in cases of an ankle sprain, cellulitis, and allergic reactions.
Neuropathic pain is also often associated with a phenomenon called allodynia. Allodynia is the sensation of pain from an activity or event that is typically not associated with causing pain. Rather than being the result of a physiological event, neuropathic pain is pathologic in nature. According to Yam, Loh, Tan, Adam, Manan, and Basir (2018), “This condition can be described as “pathologic” pain, because neuropathic pain actually serves no purpose in terms of defense system for our body, and the pain could be in the form of continuous sensation or episodic incidents” (6). It is thought to be caused by disorders affecting the peripheral or central nervous system and is linked to diseases that cause nerve damage such as trauma, toxins, diabetes, as well as certain viral infections, such as herpes zoster.

Self Quiz
Ask yourself...
Think of a patient you have encountered in your practice who experienced chronic pain.
- How would you classify this patient’s pain?
- What are the key differences between each type of pain?
- What are some examples of each type of pain?
Chronic vs. Acute
Acute pain is that which is short-term and self-limiting. The timeframe of acute pain is based on the expected healing process of the injurious event and may be up to six months. Chronic pain lasts beyond the expected period of healing or is recurrent. Acute pain can usually be attributed by a defined contributing factor or event, such as appendicitis or a broken bone. Chronic pain can be related to a myriad of causes or the etiology may be unknown.
In clinical settings, pain lasting more than three months is typically used to define the transition from acute to chronic. As such, chronic pain must be treated and managed differently than acute pain.
Risk Factors
Several risk factors have been identified that make it more likely for an individual to experience chronic pain. In general, age influences the prevalence of chronic pain by population, with those age 18 to 39 having an increased prevalence of chronic pain. This may be due to other age groups under-reporting. Those over 80 were found to report acute pain more often but were less likely to acknowledge chronic pain when asked. As well, cognitive decline, dementia and other age-related diseases must be considered as factors when collecting data. Chronic pain after surgery is reported at a higher rate amongst adolescents (7).
Chronic pain is more likely to be experienced and reported by females over males. However, studies have shown that women experience pain differently than males at a lower threshold. Women have been found to be more likely to seek treatment for pain (7,8).
Certain co-morbidities have been identified that are linked to an increase of chronic pain.
Almost 90% of patients reporting chronic pain have significant co-morbidities. Co-morbidities with the highest link to chronic pain are cardiovascular and respiratory diseases and depression. The link between chronic pain also affects mortality rates. In those reporting severe chronic pain, the 10-year survival rate is decreases significantly. At ten years, those reporting severe chronic pain are twice as likely to have died from ischemic heart disease or respiratory disease than those with little to no pain (7).
Depression and anxiety are reported at a rate four times higher in individuals with chronic pain than those living without pain (7). Specific conditions that have a higher rate of being linked to mental health disorders include (all from 9):
- Arthritis
- Fibromyalgia
- Back/Neck pain
- Chronic migraines
- Menstrual-related pain
Other factors that have been found to influence the prevalence of reported chronic pain include (7,8):
- Poverty
- Self-identify as minority
- Obesity
- Manual labor occupations
- Unemployed
- Smoker
- Alcohol use
- Lack of physical activity
- Poor nutrition
- Low levels of Vitamin D
- Post-surgical and medical interventions
- Sleep Disorders

Self Quiz
Ask yourself...
- What co-morbidities have the highest link to chronic pain?
Physical and Psychological Elements of Pain
Pain elicits a response from the sympathetic nervous system (SNS) leading to signs and symptoms affecting all systems of the body. The following are some of the physical effects that pain may cause within each individual system.
With the sensation of pain, the cardiovascular system anticipates an event that is threatening. The SNS produces a rush of adrenaline and cortisol that results in tachycardia, hypertension, and increased oxygen demand. The respiratory response includes elevated breathing that is shallow. The cortisol levels affect the endocrine system, resulting in a surge of glucose by triggering a release of glucagon from the liver that will keep up with the demands needed for the fight or flight response. In contrast, with chronic pain, continued elevated cortisol levels may lead chronic hyperglycemia. The gastrointestinal system slows gastric motility which may lead to nausea, vomiting, and constipation. Chronic pain may lead to an increase in gastrointestinal discomfort, including irritable bowel syndrome. The urinary tract reacts to stress with oversensitivity leading to an increased urgency to urinate and, in some cases, incontinence (5).
Physical indications of pain can be seen from the musculoskeletal system piloerection, tremors, and muscle tension and rigidity. The nervous system reconfigures with the processing of pain and attempts to adapt to the additional stresses. Repeated episodes of acute pain can increase the risk of an individual developing chronic pain. Cumulatively, the stresses and changes that occur on these systems have a negative effect on the immune system. The immune system is unable to keep up with the demands and because desensitized to repeated inflammation culminating in a lowered immune response. The lowered immune response then poses an increased risk of infection for the individual (5).
Psychological Reponses
Pain can cause a wide array of psychological symptoms that are subjective and may be difficult to quantify. These include anxiety and fear, poor concentration, and anxiety and/or fear (5). When pain is experienced, the activation of certain parts of the brain induce a heightened awareness and fear as a defense mechanism. Part of this process also provides a certain level of natural analgesia. With long-term pain this results in continued activation of this system, leading to increased risk for depression, anxiety, and abnormal sleep patterns (5). As stated by Swift (2018), “A high threat level induces strong emotions such as fear or intense anxiety, leading to a state of high arousal, awareness and/or vigilance, which in turn reduces sensitivity to pain. A low or moderate threat level causes a less intense response, such as low-level anxiety or depression, which induces a low-to-moderate state of arousal in which pain is more easily felt” (5).

Self Quiz
Ask yourself...
- What are some long-term effects of chronic pain on the body?
- Have you ever personally experienced pain or a patient with chronic pain that led to anxiety, depression, or sleeping disorder? How was this managed?
Pain Management
As guidelines have changed due to the opioid crisis, new evidence published by the CDC suggests that opioid dependency can occur in as little as a ten-day course of treatment. In addition, the American Pain Society and the American Society of Anesthesiologists have released guidelines that stress a multi-modal approach to pain management in the operative and recovery setting. Of the recommendations, the following were released as having high-quality evidence and strongly recommended (as cited in 10):
“. . . that clinicians offer multimodal analgesia, or the use of a variety of analgesic medications and techniques combined with nonpharmacological interventions, for the treatment of postoperative pain in children and adults”
“. . . that clinicians provide adults and children with acetaminophen and/or non-steroidal anti-inflammatory drugs (NSAIDs) as part of multimodal analgesia for management of postoperative pain in patients without contraindications”
“. . . that clinicians offer neuraxial analgesia for major thoracic and abdominal procedures, particularly in patients at risk for cardiac complications, pulmonary complications, or prolonged ileus”
“. . . that clinicians consider surgical site-specific peripheral regional anesthetic techniques in adults and children for procedures with evidence indicating efficacy”.
The shift has moved from starting patients on opioids after surgeries or other pain inducing procedures, to treating pain using the multi-modal approach which stresses using alternatives to opioids as the first line of defense. The CDC further recommends and advises (11):
“Nonopioid medications are not generally associated with development of substance use disorder. The number of fatal overdoses associated with nonopioid medications is a fraction of those associated with opioid medications. Nonopioid medications are also associated with certain risks, particularly in older patients, pregnant patients, and patients. With certain comorbidities such as cardiovascular, renal, gastrointestinal, and liver disease. Nonpharmacological treatments can reduce pain and improve function in patients with chronic pain. These treatments can also encourage active patient participation in the care plan, address the effects of pain in the patient’s life, and can result in sustained improvement in pain and function with minimal risks. If opioids are used, they should be combined with nonopioid medication and nonpharmacological treatments, as appropriate.”
Pharmacological Pain Treatments (adapted from 11):
Opioids
May be used for moderate to severe acute or chronic lower back pain, osteoarthritis, and neuropathic pain. Studies showing long-term efficacy are extremely limited. Opioids are suggested only after other non-opioid and non-pharmacological therapies have failed to provide relief. This class should be used with caution as it may induce sedation, respiratory depression, nausea and vomiting, and constipation.
Short-Acting Opioids
- Codeine
- Hydrocodone/acetaminophen or ibuprofen
- Oxycodone/acetaminophen or ibuprofen
- Hydromorphone
- Morphine
- tramadol
Long-Acting Opioids
- Fentanyl
- Hydrocodone
- Methadone
- Morphine
- Oxycodone
- Oxymorphone
- Tapentadol
Anticonvulsants
May be used for fibromyalgia, diabetic and other neuropathies, and neuralgias. Use with caution as significant drug-drug reactions have occurred. Dosing should be adjusted for renal impairment. May cause sedation, dizziness, dry mouth, weight gain, and edema.
- Gabapentin
- Pregabalin
- Carbamazepine
- Valproic acid
Antidepressants
Commonly prescribed for fibromyalgia, low back pain with radiculopathy, migraines, neuropathies and neuralgias, and chronic musculoskeletal pain. Patient must be monitored for mood changes and is at an increased risk for suicide. Other side effects may include sedation, urinary retention, dry mouth, weight gain, and blurry vision. Cardiac patients must be monitored for arrythmias and blood pressure changes.
Tricyclic Antidepressants
- Amitriptyline
- Desipramine
- Nortriptyline
Serotonin-Norepinephrine Reuptake Inhibitors
- Duloxetine
- Milnacipran
- Venlafaxine
Muscle Relaxers
Effective for acute lower back pain and fibromyalgia. May cause sedation and dizziness. Caution must be used when operating a car or machinery.
- Carisoprodol
- Cyclobenzaprine
- Metaxalone
- Methocarbamol
- Tizanidine
Topical Agents
Helpful for osteoarthritic and rheumatoid arthritic pain as well as neuropathies. May be used for relief of sprains, strains, and back pain.
- Capsaicin
- Diclofenac Topical Gel
- Lidocaine 5% patches
- Menthol/Salicylate
Non-Steroidal Anti-Inflammatory Drugs
May be used to treat backache, joint pain and inflammation, headache, arthritic pain, muscle aches and strains, and menstrual cramps. Caution to be used in patients with liver or kidney disease and alcohol misuse. May cause gastrointestinal discomfort or bleeding. Use with caution if patient in on anticoagulation therapy.
- Ibuprofen
- Diclofenac
- Indomethacin
- Meloxicam
- Naproxen
- Celecoxib
- Aspirin
Acetaminophen
Remains one of the most prescribed pain relievers for headache, backache, muscle ache, and joint pain. Caution must be used with liver disease and alcohol misuse. Dosage must not exceed 3,000 – 4,000 mg/day.
Interventional Treatments
Include epidural or intraarticular glucocorticoid injections and arthrocentesis. The CDC recommends these for short-term treatment of inflammatory diseases such as rheumatoid arthritis, osteoarthritis, rotator cuff disease and other radiculopathies.

Self Quiz
Ask yourself...
- What Are some examples of long-acting opioids?
- What are some examples of short acting opioids?
- Why is it so important to monitor for mood changes with antidepressants?
Non-Pharmacological Treatment
The CDC provides many strategies for healthcare providers to manage the challenges of patient pain control in a manner that lessens the need for opioid use and provides alternative options. Primarily, a patient-centered approach to treatment is now the gold standard and should include patient engagement.
Suggestions and strategies to incorporate patient cooperation and engagement with their pain management plan include (all from 12):
- Use reflective listening by maintaining eye contact, empathizing, and confirming understanding
- Set agreed upon, reasonable and achievable goals
- Discuss treatment options using a multi-modal treatment plan
As part of a multimodal therapy in treating pain, the CDC highly recommends incorporating exercise along with other psychologically based approaches into care. These may include:
- Physical and Occupational Therapy, including exercise such as swimming, yoga, walking, free weights, and other strength training. This can improve strength and posture, which may provide relief from lower back, hip, and osteoarthritic pain, improve fibromyalgia symptoms, and has been shown effective in preventing migraines (12).
- Cognitive behavior therapy (CBT) is a psychosocial training technique that addresses modifiable situation factors and cognitive processes that may affect the experience of pain. CBT aims to provide coping techniques, relaxation methods, and may include self-help instruction, professional counseling, or support group attendance (12).
- Heat Therapy
- Cryotherapy
- Massage
- Ultrasound
- Transcutaneous Electric Nerve Stimulation (TENS) Units
- Acupuncture
- Hypnosis
- Stress Management
- Chiropractic Manipulation
- Herbal Preparations
- Aromatherapy

Self Quiz
Ask yourself...
- Can you think of a patient experience that you have used cognitive behavior therapy to help better manage their pain?
- Do you think it was effective?
- Why or why not?
Federal and Michigan Laws on Opioid Prescribing and Use
In 2016, the CDC reported that over 40 Americans were dying each day due to prescription opioid overdoses. The opioid crisis has been attributed to the over prescribing of opioids for pain and non-pain conditions with a lack of oversight leading to a 400% increase in opioid prescribing and sales since 1999 (13). In response, the federal government implemented an initiative to combat the issue with improved education, guidelines, and treatment management. In October of 2018, the Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act, a 660-page bill was signed into law. This comprehensive, bi-partisan legislation aimed to provide funding and expand access to increase treatment availability through Medicaid and Medicare, expand alternative non-opioid pain management treatment, set guidelines for improved patient education, and identify best practices.
Prescription-drug monitoring program and the use of electronic prescribing for Schedule II and III medications is supported by the Federal government and allows individual states to have primary control over authorization and enforcement. The following are the regulatory practices specific to Michigan.
Drug Classification and Schedule in Michigan
Under the Public Health Code, Act 368, state and federal agencies monitor certain drugs based on their risk of addiction, dependance, and abuse characteristics. These controlled substances are categorized based on a system of Schedules I through V. There are three criteria that determines the drugs category: acceptable medical use, potential for abuse, and the predictive value of dependance if it is abused (14). The schedules are as follows:
Schedule I
Schedule I drugs are considered to have no appropriate medical use and have an extremely high potential for abuse. Examples of Schedule I drugs include:
- LSD
- Heroin
- Bath Salts
- Quaaludes
Schedule II
Schedule II drugs have a high potential for abuse and may lead to psychological or physical dependance. Examples of Schedule II drugs include:
- Fentanyl
- Demerol
- OxyContin
- Morphine
- Codeine
- Marijuana
Schedule III
Schedule III drugs have a high potential for abuse and may lead to psychological or physical dependence. Examples of Schedule III drugs include:
- Acetaminophen with Codeine
- Vicodin
- Suboxone
- Ketamine
- Anabolic Steroids
Schedule IV
Schedule IV drugs have a low to moderate potential for psychological or physical dependence but have a lower risk for abuse. Examples of Schedule IV drugs include:
- Ativan
- Xanax
- Valium
- Soma
- Klonopin
Schedule V
Schedule V drugs are a low potential for physical or psychological dependence or abuse. Examples of Schedule V drugs include:
- Gabapentin
- Robitussin
- Ezogabine
- Phenergan with Codeine
Michigan Laws
In 2016, Michigan, along with 32 other states, recognized the dramatic increase in deaths caused by overdoses in the United States. Overdose had become one of the leading causes of accidental death in the nation. The Good Samaritan Laws were introduced to encourage quick response to potentially fatal overdoses with a decrease in the fear for legal repercussion.
Michigan’s Good Samaritan Law
As stated by Michigan Department of Health and Human Services:
During a drug overdose, a quick response can save a life. However, people illegally using drugs sometimes fail to seek medical attention during an overdose for fear of alerting the police to their illegal drug use. In order to prioritize saving lives, Michigan passed a Good Samaritan law in 2016.
Michigan’s Good Samaritan law prevents drug possession charges against those that seek medical assistance for an overdose in certain circumstances. This law makes saving lives the priority during a drug overdose, not criminal prosecutions of illegal drug users (15,16).
The following are pertinent Public Acts and Laws enacted starting in 2017 that were put into effect to support the efforts of tackling the opioid crisis. This also gives structure to primary care providers ability to prescribe opioids and decreases the accessibility of opioids through (all from 15):
Public Act 246 of 2017
Disclosure of prescription opioid information with the risks to minors and patients is required, beginning 6/1/18. This act also includes the use of the Start Talking form. The form includes the patient’s information, type of controlled substance containing an opioid, signature of patient or guardian, and number of refills allowed. The form required that the provider shares the following information to the patient regarding the substance having potential for abuse (MDHHS-5730, Rev. 3-20):
- The risks of substance use disorder and overdose associated with the controlled substance containing an opioid.
- Individuals with mental illness and substance use disorder may have an increased risk of addictions to a controlled substance. (Required only for minors.)
- Mixing opioids with benzodiazepines, alcohol, muscle relaxers, or any other drug that may depress the central nervous system can cause serious health risks, including death or disability. (Required only for minors.)
- For a female who is pregnant or is of reproductive age, the heightened risk of short and long-term effects of opioids, including by not limited to neonatal abstinence syndrome.
- Any other information necessary for patients to use the drug safely and effective as found in the patient counseling information section of the labeling for the controlled substance.
- Safe disposal of opioids has shown to reduce injury and death in family members. Proper disposal of expired, unused, or unwanted controlled substances may be done through community take-back programs, local pharmacies, or local law enforcement agencies. Information on where to return you prescription drugs can be found at http://www.michigan.gov/EGLEDrugDisposal.
- It is a felony to illegally deliver, distribute or share a controlled substance without a prescription properly issued by a licensed health care prescriber.
Public Act 247 of 2017
Requires prescribers to be in a bona fide prescriber-patient relationship prior to prescribing Schedules 2-5 controlled substances. These provisions were due to take effect on 3/31/18, however the implementation date has been pushed back by Public Act 101 of 2018.
Public Act 248 of 2017
Requires the review of MAPS prior to prescribing or dispensing to a patient a controlled substance in a quantity that exceeds a 3-day supply, beginning 6/1/18. Further, the act requires that a licensed prescriber be registered with MAPS prior to prescribing or dispensing a controlled substance to a patient, beginning 6/1/18.
Public Act 249 of 2017
Provides sanctions for failing to comply with the new MAPS usage mandates, failure to establish bona fide prescriber-patient relationships, and failure to inform patients regarding the risks associated with the prescription of opioid drugs.
Public Act 250 of 2017
Requires health professionals that treat patients for opioid-related overdoses to provide such patients with information regarding Substance Use Disorder Services, beginning 3/27/18.
Public Act 251 or 2017
Requires prescribers treating for acute pain to not prescribe such patients with more than a 7-day supply of an opioid within a 7-day period, beginning 7/1/18.
Public Act 252 of 2017
Provides that before dispensing or prescribing buprenorphine or a drug containing buprenorphine and methadone to a patient in a substance use disorder program, the prescriber shall review a MAPS report on the patient, beginning 3/27/18.
Public Act 253 of 2017
Codifies Medicaid coverage for detox programs, beginning 3/27/18.
Public Act 254 of 2017
Requires the Prescription Drug and Opioid Abuse Commission (PDOAC) to develop for Michigan’s Department of Education (MDE) recommendations for the instruction of pupils on the dangers of prescription opioid drug abuse, by 7/1/18.
Public Act 255 of 2017
Requires MDE to make available to school districts a model program of instruction on the dangers of prescription opioid abuse, developed or adopted by the PDOAC, by 7/1/19. Further, beginning in the 2019-2020 school year, MDE shall ensure that the state include within its health education standards, instruction on prescription opioid drug abuse.
Public Act 101 of 2018
Pushes back the effective date for the bona fide prescriber-patient relationship requirement to 3/31/19, on the date on which rules are promulgated.

Self Quiz
Ask yourself...
- What is Michigan’s Good Samaritan Law? Do you feel this is beneficial?
- What is the daily supply limit of an opioid hen a patient is being treated for acute pain? Is this helpful in helping to further exacerbate the opioid crisis? In what instances would this be problematic?
CDC Guidelines and Recommendations on Prescribing and Use
The CDC continues to promote guidelines initiated in 2016 to support the U.S. government’s initiative to curb the increasingly troubling deaths related to opioid overdose. These guidelines were aimed at assisting primary healthcare providers in effectively managing and treating patient’s pain while addressing health and safety concerns. In relation to opioid use, the guidelines revolved around three main principles (all from 13):
- Nonopioid therapy is preferred for chronic pain outside of active cancer, palliative, and end-of-life care.
- When opioids are used, the lowest possible effective dosage should be prescribed to reduce risks of opioid use disorder and overdose.
- Providers should always exercise caution when prescribing opioids and monitor all patients closely.
Drug Diversion Within the Healthcare System
According to the Drug Enforcement Administration, the most commonly abused drugs are among five classes and are frequently used in the treatment of pain. These include opioids, depressants, stimulants, hallucinogenic, and anabolic steroids. Of these, the opioid fentanyl is the number one drug that is found to be involved in drug diversion cases (17).
When used outside of medical purposes, fentanyl has a very high rate of fatality. Far from being just a public problem, the diversion of drugs is a significant problem for healthcare organizations and abusers can be found at all levels, from the C-suite to frontline staff. There are several signs of drug diversion, including poor appearance, failing job performance, uncharacteristic behaviors for the individual, and accessing medication that is not required for their job (17).
The Joint Commission offers these guidelines for monitoring to identify potential trends and patterns that may indicate the occurrence of drug diversion in the clinical setting (all from 17):
- Schedule II – V substances are removed:
- Without provider orders
- Under patients not assigned to the nurse
- Under patients that have been discharged or transferred
- Excessively by one individual
- Substitute drug is removed and administered while controlled substance is diverted’
- Verbal order for controlled substances is created but not verified by prescriber
- Prescription pads are diverted and used to forge prescriptions for controlled substances
- Provider self-prescribes controlled substances
- Patient alters written prescription
- Unadministered medication that is documented as given to patient
- Wastes are not completed according to policy and procedures
- Multiple discrepancies or overrides are noted
- Patient’s report unrelieved pain, despite increasing documented pain medication administration
- Assistance is frequently offered to administer medications for other nursing staff
- Expired controlled substances go missing or are diverted from medication dispensing systems
Individual policy and procedure should be followed when drug diversion is recognized in a clinical setting with consideration to the safety of the patients and offender both addressed. The drug diversion should be reported to an immediate supervisor or manager. Nursing management should contact Quality Control and initiate a thorough root-cause analysis.
Risks of drug diversion include transmission of blood borne pathogens, patient safety compromised due to impaired healthcare provider, uncontrolled patient pain, and potential for healthcare provider overdose.
The Joint Commission advocates for a “see something, say something” approach to combatting healthcare provider drug diversion. A plan to prevent drug diversion within the health care organizations should include three approaches: prevention, detection, and response.
Additionally, they state “Detection of drug diversion is challenging, and even the best efforts have not yet achieved complete eradication of diversion. Patient and workplace safety require effective reliable safeguards to maintain the integrity of safe medication practices to protect against diversion. Diversion prevention requires continuous prioritization and active management to guard against complacency” (17).

Self Quiz
Ask yourself...
- What can you do as a healthcare provider to prevent healthcare provider drug diversion?
- Have you seen specific examples of healthcare provider drug diversion in your workplace? What can you learn from that situation?
Risks of Opioid Use and Misuse
Opioids target mu receptors in the brain and spinal cord. Through inhibition of GABA, dopamine is released. Opioid’s increased risk for addiction is due to the increase of circulating dopamine which is associated with increased pleasure responses. Opioid use has been clinically linked to an increase in addiction as well as substance use disorder. Substance use disorder has been defined by the American Psychiatric Association (ASA) as “. . . a problematic pattern of use of an intoxicating substance, leading to clinically significant impairment or distress” (18). Per the ASA, this is calculated by at least two of the following characteristics (all from 18):
- The substance is often taken in larger amounts or over a longer period than it was intended
- There is persistent desire or unsuccessful effort to cut down or control use of the substance
- A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from its effects
- Craving or a strong desire or urge to use the substance
- Recurrent use of the substance, resulting in a failure to fulfill major role obligations at work, school, or home
- Continued use of the substance despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of its use
- Important social, occupational, or recreation activities are given up or reduced because of use of the substance
- Recurrent use of the substance in situations in which it is physically hazardous
- Use of the substance is continued despite having knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance
- Tolerance: a need for markedly increased amounts of the substance to achieve intoxication or desired effect OR a markedly diminished effect with continued use of the same amount of the substance
- Withdrawal: characteristic withdrawal syndrome for that substance OR the substance (or a closely related substance) is taken to relieve or avoid withdrawal symptoms
A comparison study was performed based on information garnered in a 2016-2017 study group that focused on the use and misuse of opioids among individuals medicating with opioids inappropriately. This group was split into four categories and compared medical prescription opioid users with prescriptions with the following: misusers without prescriptions, misusers of own prescriptions, and misusers with both types of misuse (19).
Individual misusers without a prescription were typically younger, male, and unmarried versus misusers with prescriptions, whether using medically or misusing. It was found that misusers also had an alcohol disorder, used marijuana, and misused benzos and stimulants. As well, noted was that misusers were more likely to be nicotine dependent and to use cocaine and/or heroin (19).
Prescription users were more likely to concurrently use prescribed benzodiazepines and stimulants. Depression among all misusers was higher compared with the medical users. The misuser also more commonly had received treatment from an inpatient mental health treatment center as well as had been prescribed a medication for a mental health condition. Overall, this group was not more likely to have a physical health condition (19).
Perceived Barriers to Pain Management
As another consequence of the opioid crisis, a stigma has been cast upon individuals with chronic pain whether they are taking opioids or not. Healthcare professionals should be cautioned against projecting biases onto sufferers of pain as seeking pain medications for misuse reasons. As previously detailed, many patients experiencing pain have co-morbidities and are at a higher risk of having mental health issues in addition to pain.
Barriers to non-opioid and non-pharmacological pain control may include insufficient medication regimen ordered to address patient’s pain, inadequate training, nursing workload, and a lack of collaborative approach by the healthcare team (20). Barriers to the use of non-pharmacological pain relief methods have been cited as (all from 20):
- Inadequate training of personnel in how to examine pain and non-pharmacological control methods
- Patients’ lack of cooperation in the use of non-pharmacological methods to relieve pain
- Insufficient knowledge about non-pharmaceutical pain relief methods
- Time-consuming methods of nonpharmaceutical pain relief
- Nurse’s reluctance to use non-pharmaceutical pain relief methods
- Failure to use non-pharmacological methods by the physician
The study found that with improved education, communication, and collaboration, improved pain management can be achieved by patients.

Self Quiz
Ask yourself...
- What are some steps that you as a healthcare provider can take in preventing the stigma with chronic pain patients as it relates to opioid use?
Nursing Considerations and Interventions
Nursing care plans focused on pain management may be categorized by acute or chronic pain; however, the management and interventions are very similar for each. The outcomes should be specific to the patient presentation, disease process, and preferences (21).
Pain Assessment and Screening Tools
Screening tools are one of the easiest and most effective ways to evaluate for pain. Some of the most commonly used tools in clinical care include (5, 21):
- Wong-Baker FACES Scale – may be used for children over the age of 3 and adults
- FLACC and CRIES – used for infants
- COMFORT Scale – May be used in children and cognitively impaired or sedated adults
- Visual Analog Scale
- Numerical Rating Scale
Pain should be also assessed by the patient reported characteristics using pain standardization scales such the McGill Pain Questionnaire. Some of the verbiage used to describe pain include (5):
- Aching
- Burning
- Shooting
- Stabbing
- Throbbing
- Tender
In addition to screening tools, the nursing assessment should include visualization of signs of pain that can include guarding or protecting certain areas of the body, facial changes such as grimacing or furrowing of brows, and other manifestations of pain such as restlessness, moaning, or crying (5).

Self Quiz
Ask yourself...
- Which of the pain scale tools have you used in your professional practice? Do you think they were effective in helping you determine your patients’ level of pain? Do you think one is more effective than another?
Nursing Interventions Related to Pain
- Provide therapeutic communication and patient-centered care, taking into consideration patient preference.
- Assess and document patient baseline of vital signs, complete head-to-toe assessment, and review medications.
- Assess and document patient pain through use of a pain scale, and responses to interventions.
- Establish an agreed upon pain level that is acceptable to the patient, providing education that no pain at all is not a reasonable goal.
- Administer pain medications per physician orders.
- Regularly assess for sedation in patients who are receiving pain medication.
- Administer naloxone for patients presenting with clinical signs of over-sedation with opioid use.
- Provide education on and integrate alternative pain t per patient preference and provider orders.
As nurses, being able to have a firm concept of the different types of pain, the contributing factors that lead to pain and the various modes of treatment will allow you to provide better care for your patients, while simultaneously allowing you to relate to them on a more specific level and formulate a more individualized plan of care.
Opioid Abuse
What are Opiates?
Opiates are powerful substances which are commonly used to alleviate both acute and chronic pain. The history of opiate use / abuse goes back many thousands of years. The first recorded reference is from 3,400 B.C. when opium was cultivated in southwest Asia. There were even wars fought over the previous flow in the mid 1800s (1). The most famous historical event related to opium were the advent of “opium dens.” These were underground “dens” where opium was bought, sold, and used (1). Much like today, the addictive properties of opium overcame many individuals and caused great harm to the world and communities. Indeed, the opiate epidemic of the 2000’s is not the first in modern history, though it is much different and more severe than previous epidemics.
Today opiates are used for both acute and chronic pain. The ability to quickly, reliably, and (when used appropriately) safely reduce pain is what makes the drug class so valuable. Many common drugs are opiate derivatives or synthetics including morphine, codeine, oxycodone, heroin, hydromorphone, and fentanyl.
In the United States Opiates are considered controlled substances and most of them are classified as schedule II (with heroin classified as schedule I) (2). Opiates will always have a place in medicine and treatment of pain and are incredibly useful, however, the current opiate epidemic in America makes clear the potential consequences of opiate abuse.
Preventing Abuse, Misuse, and Harm
Every day 130 Americans die of opiate overdose (3). Additionally, there are 4.3 million Americans each month who engage in the non-medical (non-prescribed or illicit) use of opiates (5). However, it is key to remember that opiate-related deaths are not the only negative consequences. There are many overdoses which do not end in death, and on the other end of the spectrum many negative affects do not cause death. Addiction can cause loss of job, damage to relationships, psychologic distress, homelessness, and many more negative side-effects.
So how do healthcare professionals help reduce the impact of opiate addiction and misuse? The approach must be multi-modal, aimed at primary, secondary, and tertiary prevention.
- Primary prevention includes appropriate opiate prescribing, risk stratification with patients, and preventing opiate addiction.
- Secondary prevention is aimed at mitigating the effects of opiate addiction. This includes rehabilitation and cessation of opiates in addicted individuals, ideally in favor of non-opiate treatment options.
- Tertiary prevention is the reduction in harm from opiate addiction and overdose. This includes resuscitation of overdose patients and helping patients recover from the effects of opiate addiction.
Appropriate Prescribing
The Centers for Disease Control and Prevention (CDC) offers excellent guidance on how to appropriate prescribe opiates, though it will continue to require a great deal of knowledge and effort from individual prescribers and managers of chronic pain. For the purposes of this article, we will focus on the CDC recommendations. Below we will discuss the 12 key points of opiate management, per the CDC.
1. Opioids Are Not First-Line Therapy
“Nonpharmacologic therapy and nonopioid pharmacologic therapy are preferred for chronic pain. Clinicians should consider opioid therapy only if expected benefits for both pain and function are anticipated to outweigh risks to the patient. If opioids are used, they should be combined with nonpharmacologic therapy and nonopioid pharmacologic therapy, as appropriate.” (5)
Author’s Input
Many patients experience pain. Indeed, it is one of the most common complaints in primary care offices. When dealing with chronic pain, we should consider ALL non-opiate therapies for patients prior to prescribing opiates. This can include physical therapy, meditation, exercise / movement, treatment of underlying depression and/or psychiatric issues, meditation, modification of aggravating factors, and many more interventions. In some cases, none of these alone or combination will be enough to provide satisfactory relief, but we must utilize non-opiate and non-pharmacological solutions as much as possible to reduce opioid abuse, and dose (if opiates are necessary).
2. Establish Goals for Pain and Function
“Before starting opioid therapy for chronic pain, clinicians should establish treatment goals with all patients, including realistic goals for pain and function, and should consider how opioid therapy will be discontinued if benefits do not outweigh risks. Clinicians should continue opioid therapy only if there is clinically meaningful improvement in pain and function that outweighs risks to patient safety “(5).
Author’s Input
Many patients erroneously believe that cessation of pain is the goal of therapy. This is not based in fact nor is it reasonable, as many patients (even with opiate therapy) will not have complete remission of pain. The goal of the clinician should be to work with the patient to provide the minimal risk intervention that will provide acceptable pain control.
3. Discuss Risks and Benefits
“Before starting and periodically during opioid therapy, clinicians should discuss with patients known risks and realistic benefits of opioid therapy and patient and clinician responsibilities for managing therapy” (5).
Author’s Input
A prescription for an opiate should never be written to a patient without a through discussion of the risks and benefits. The clinician must first be convinced that the risk to benefit favors prescribing an opiate. Then, they must discuss their rationale with the patient. An individual assessment regarding the risks should be provided to each and every patient.
4. Prescribe Immediate-Release Opioids First
“When starting opioid therapy for chronic pain, clinicians should prescribe immediate-release opioids instead of extended-release/ long-acting (ER/LA) opioids” (5).
Author’s Input
Extended-release opioids have been associated with higher rates of overdose and higher potential for Opioid abuse. Immediate-release opioids should be utilized first, whenever possible.
5. Clinicians Should Prescribe the Lowest Effective Dosage
“Clinicians should use caution when prescribing opioids at any dosage, should carefully reassess evidence of individual benefits and risks when considering increasing dosage to ≥50 morphine milligram equivalents (MME)/day, and should avoid increasing dosage to ≥90 MME/day or carefully justify a decision to titrate dosage to ≥90 MME/day.”
Author’s Input
The clinician must keep in mind that the “minimum required dose” may change over time. As a patient implements more non-pharmacologic interventions the required dose may decrease. Conversely, there can be some degree of tachyphylaxis with opiates and the required dose may also increase. Dose titration requires careful clinician judgement.
6. Prescribe Short Durations for Acute Pain
“Long-term opioid use often begins with treatment of acute pain. When opioids are used for acute pain, clinicians should prescribe the lowest effective dose of immediate-release opioids and should prescribe no greater quantity than needed for the expected duration of pain severe enough to require opioids. Three days or less will often be sufficient; more than seven days will rarely be needed” (5).
Author’s Input
It is well established that chronic opioid therapy is not the most effective therapy for pain management. Clinicians should consider adjuncts for ongoing or chronic pain patients.
7. Evaluate Benefits and Harms Frequently
“Clinicians should evaluate benefits and harms with patients within 1 to 4 weeks of starting opioid therapy for chronic pain or of dose escalation. Clinicians should evaluate benefits and harms of continued therapy with patients every 3 months or more frequently. If benefits do not outweigh harms of continued opioid therapy, clinicians should optimize other therapies and work with patients to taper opioids to lower dosages or to taper and discontinue opioids” (5).
Author’s Input
It is important that clinicians consider changing circumstances. A patient’s health status or life circumstances may change such that opiate therapy benefits no longer outweigh the harm, or vice-versa.
8. Use Strategies to Mitigate Risk
“Before starting and periodically during continuation of opioid therapy, clinicians should evaluate risk factors for opioid-related harms. Clinicians should incorporate into the management plan strategies to mitigate risk, including considering offering naloxone when factors that increase risk for opioid overdose, such as history of overdose, history of substance use disorder, higher opioid dosages (≥50 MME/day)” (5).
Author’s Input
Naloxone therapy should be considered for all patients who are at high risk of Opioid overdose.
9. Review Prescription Drug Monitoring Program Data
“Clinicians should review the patient’s history of controlled substance prescriptions using state prescription drug monitoring program (PDMP) data to determine whether the patient is receiving opioid dosages or dangerous combinations that put him or her at high risk for overdose. Clinicians should review PDMP data when starting opioid therapy for chronic pain and periodically during opioid therapy for chronic pain, ranging from every prescription to every 3 months” (5).
Author’s Input
Each state has robust data regarding prescription medication; utilizing this data can help reduce opioid misappropriation and concurrent prescriptions (doctor shopping).
10. Use Urine Drug Testing
“When prescribing opioids for chronic pain, clinicians should use urine drug testing before starting opioid therapy and consider urine drug testing at least annually to assess for prescribed medications as well as other controlled prescription drugs and illicit drugs,” (5).
Author’s Input
The author recommends that clinicians take great care in this area. Indeed, drug testing can help identify those who are already abusing other substances, but it can also harm the trusting relationship developed between a patient and clinician. The patient should be re-assured that the testing is performed for their own good and out of concern for their own health, rather than punitively or because the clinician “mistrusts” them, as these may be the default thoughts of many patients.
11. Avoid Concurrent Opioid and Benzodiazepine Prescribing
“Clinicians should avoid prescribing opioid pain medication and benzodiazepines concurrently ‘whenever possible’ “(5).
Author’s Input
The highest risk of overdose of opioid abuse is commonly seen when opiates and benzodiazepine (or any combination of sedating medications) are prescribed concurrently, especially in conjunction with alcohol. For this reason, clinicians should strongly consider avoiding such risks and only prescribing this combination when absolutely necessary.
12. Offer Treatment for Opioid Abuse Disorder (OAD)
“Clinicians should offer or arrange evidence-based treatment (usually medication-assisted treatment with buprenorphine or methadone in combination with behavioral therapies) for patients with opioid abuse disorder” (5).
Author’s Input
In acute cares settings, clinicians often view OAD as a secondary illness and it is frequently left unaddressed. However, there are now effective treatments for OAD. Given the significant morbidity, mortality, and associated quality of life issues, patients with OAD should be offered treatment, even if it not the primary reason for treatment.
Risk Factors for Opiate Harm or Misuse
The risk to benefit has been discussed many times previously and is often referenced by the CDC. The benefits of opiate therapy are typically obvious (reduced pain, increased quality of life, etc.), but the risks are less often discussed. So how do nurses know who is at higher risk of the negative effects of opiates?
According to the CDC, the major risk factors are:
- Illegal drug use; prescription drug use for non-medical reasons.
- History of substance use disorder or overdose.
- Mental health conditions (e.g., depression, anxiety).
- Sleep-disordered breathing. • Concurrent benzodiazepine use (6).
Mortality from opiates is highest in those who are middle-aged, have psychiatric conditions, and/or have previously abused substances (7). It is important that clinicians utilize this information when consider risk and benefits associated with opiate therapy.
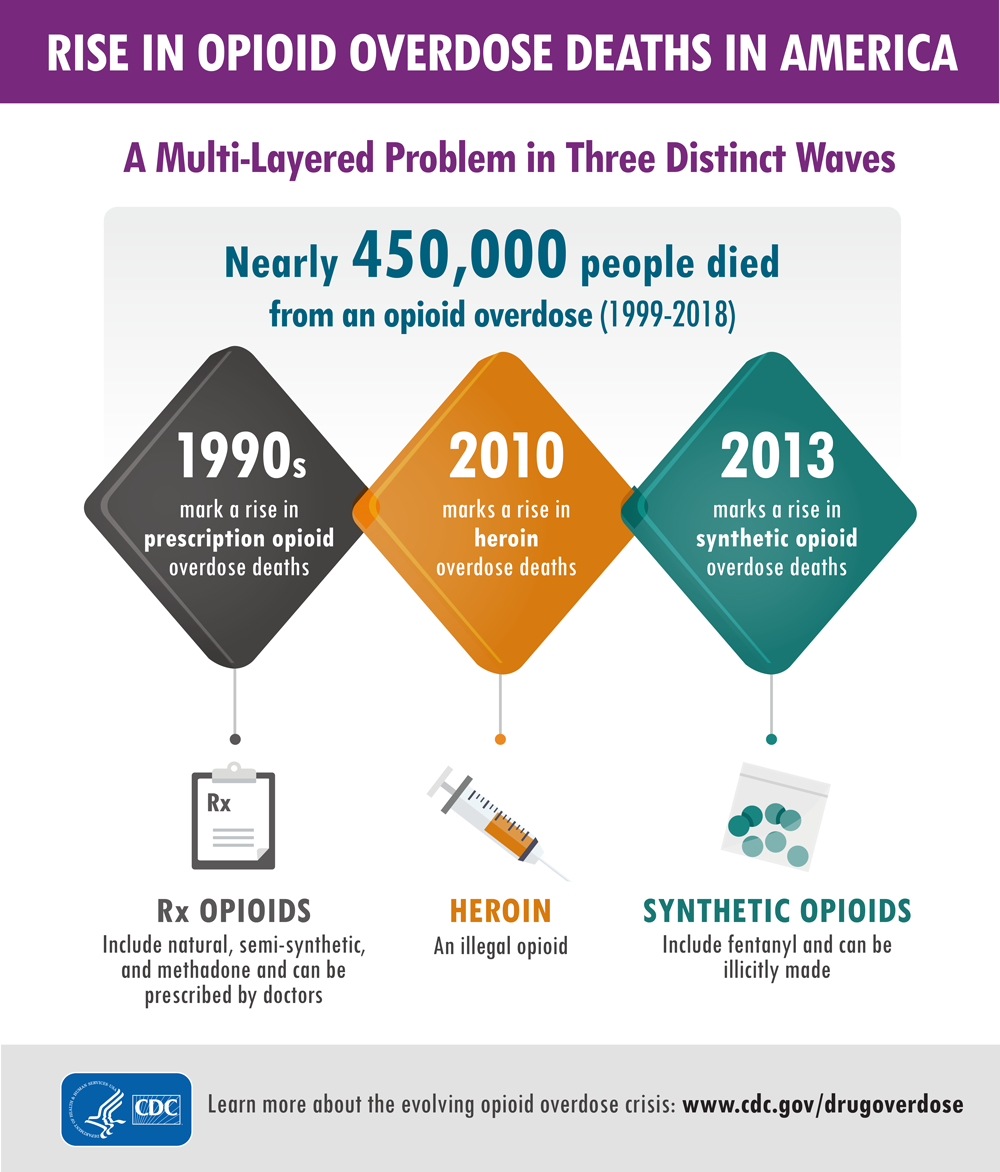
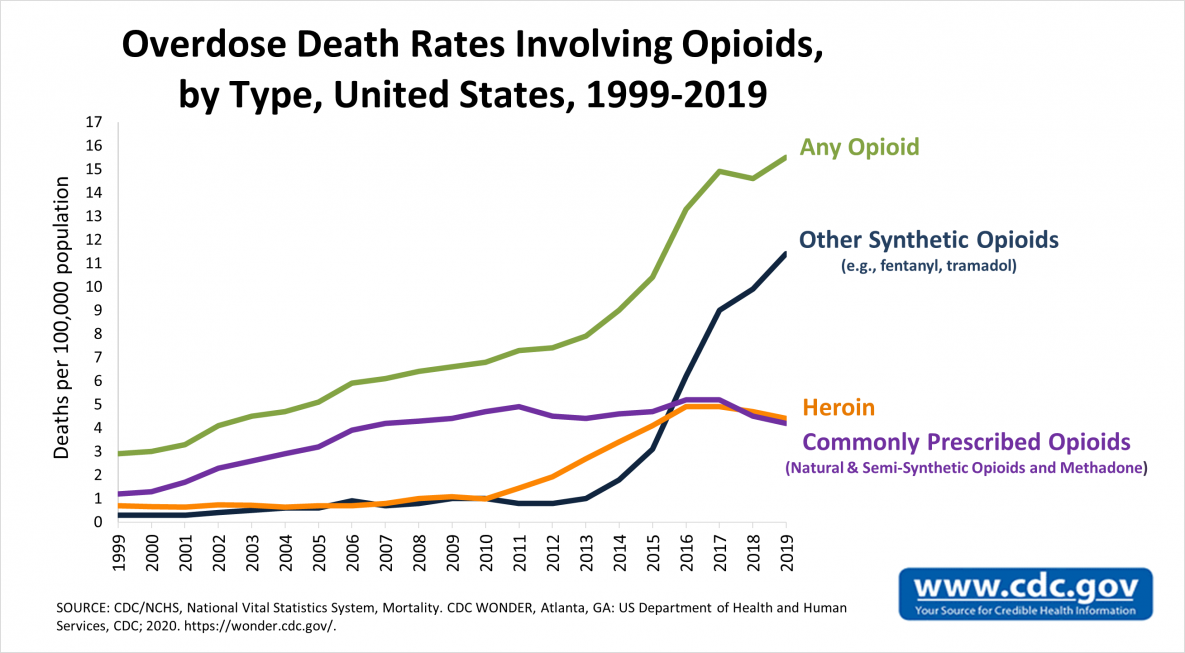
Signs of Abuse, Diversion, and Addiction
Clinicians should remain vigilant for signs of opiate use disorder, as it can occur in any patient (even those not prescribed opiates). Opiate use disorder is characterized in the DSM-5 as a desire to utilize opiates despite social and professional consequences (12). It includes dependence and addiction, with addiction being on the severe end of the spectrum (12). Opiate use disorder can be diagnosed when at least two of the following are observed in a 12-month period:
- Opioids are often taken in larger amounts or over a longer period than was intended.
- There is a persistent desire or unsuccessful efforts to cut down or control opioid use.
- A great deal of time is spent in activities necessary to obtain the opioid, use the opioid, or recover from its effects.
- Craving, or a strong desire or urge to use opioids.
- Recurrent opioid use resulting in a failure to fulfill major role obligations at work, school, or home.
- Continued opioid use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of opioids.
- Important social, occupational, or recreational activities are given up or reduced because of opioid use.
- Recurrent opioid use in situations in which it is physically hazardous.
- Continued opioid use despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance.
- Exhibits tolerance (discussed in the next section).
- Exhibits withdrawal (discussed in the next section) (centers for disease control, reference 13).
Urine drug screening can be useful in patients with suspected opiate abuse disorder as it may identify concurrently abused substances. If a patient is found to have opiate abuse disorder the “risk” side of the “risk-to-benefit” equation is now shifted, and the continued use should be carefully weighed against the potential for negative effects, including addiction. Addiction is defined as continued use despite adverse events or consequences (12).
For those prescribed opiates, clinicians should have candid conversations about the risks of continued use for those with OAD. The CDC offers some creative examples of how to discuss the condition with patients, which nurses may find helpful in their interactions (these are only examples, and the wording depends on the patient’s specific scenario and needs):
“Trouble controlling the use of opioid medication makes it unsafe, and long-term risk over time is substantial.”
“The medicine has become a problem in itself. You have developed a known complication of therapy that we should not ignore.”
“Continuing the current medication is not a reasonable option due to the risks, but there are options for treating what we call opioid use disorder, also known as OUD.”
“It seems as if you are running out of your medication more quickly than anticipated.”
“Sometimes people become too comfortable with the medications and start to take them for reasons other than pain.”
“You meet the criteria for opioid use disorder, also known as OUD. It’s helpful to put a name on it because it opens up a variety of approaches to help with your specific circumstance.” (All derived from source 13).
So, once we identify a patient with OAD, what do we do? At this point, as above, a candid conversation with the patient must occur. A treatment plan should be formulated, which would include a careful consideration for discontinuing for the opiate (if possible). This provides an excellent transition into our next section, opiate alternatives.
Opiate Alternatives
Opiate alternatives can be broadly classified as pharmacologic and non-pharmacologic. We will first discuss pharmacologic alternatives.
Pharmacologic:
Acetaminophen
Commonly known as Tylenol ™ is over the counter and has a very favorable safety profile when used correctly. Acetaminophen is considered first-line therapy in any pain management regimen (9).
NSAIDs (Nonsteroidal anti-inflammatory drugs)
NSAIDs can be immensely powerful in pain management, as many pain conditions are related to inflammation. However, patient tolerance can be an issue with chronic NSAID exposure. Indeed, many clinicians shy away from NSAIDS due to the perceived risk profile (9).
Tricyclic Antidepressants
TCAs provide significant pain relief to many patients, as they have the unique ability to change the perceptions of pain (5). However, tricyclics have many side-effects of their own and thus have been phased out in lieu of newer antidepressants. This in the pain realm they should be considered for certain patients, particularly those with concurrent untreated depression.
SSRI Antidepressants
SSRIs are typically tolerated better than tricyclics (9) but again are not recommend for first-line analgesia. They are typically reserved for those with concurrent psychiatric illness which may benefit from the overall effect of the drug, and on a case-by-case basis for selected patients.
Muscle Relaxants
Medications such as gabapentin can be extremely useful especially in pain originating from musculoskeletal causes. However, the mechanism of action is poorly understood (9) and side effects can be troublesome. In one study approximately 25% of patients taking muscle relaxants for chronic pain discontinued the agents due to adverse effects.
Topicals
Many topical agents now exist, including NSAIDS (9). Topicals are typically considered analgesic-sparing rather than standalone treatment (9). The American College of Rheumatology has excellent and detailed guidance on how to utilize topicals, which deserves a course of its own.
Corticosteroids
Corticosteroids have very potent anti-inflammatory effects (9) and have a proven role in pain management. Short-term therapy is typically favored over long-term therapy due to the potential issues of long-term systemic therapy (osteoporosis, immunosuppression, risk of serious or fatal infections, weight gain, muscle weakness, diabetes, Cushing’s syndrome, hypertension, glaucoma, and cataracts). Though some serious adverse events can occur with short-term therapy (psychosis, anxiety, avascular necrosis, etc.) (9). corticosteroids can be beneficial for patients with acute pain. Perhaps the best use of these agents is in targeted (injectable) delivery.
Non-Pharmacologic:
These therapies will be discussed less in-depth, as they typically require referrals for treatment. However, it is important that nurses are aware of the of the existence of these therapies and can make appropriate referrals and recommendations. Physical therapy consults are invaluable as they often utilize many of the tools below and are more knowledge about non-pharmacologic therapies in general.
- psychological interventions (including distraction, stress management, hypnosis, and other cognitive-behavioral interventions)
- acupuncture and acupressure
- transcutaneous electrical nerve stimulation
- physical therapies (including massage, heat/cold, physiotherapy, osteopathy, and chiropractic) (10)
Conclusion
Nurses should view the non-pharmacologic therapies as “tools” available to help patients dealing with acute and chronic pain. Though opiate therapy is a valuable tool as well, its potential negative effects are often under-considered, and the rate of opiate prescription currently is excessive (10).
When evaluating patients with pain, nurses should work with patients and providers to ensure that the patient is on an optimal pain regimen, which ideally should include both pharmacologic and non-pharmacologic therapies. Seeking referral and consultation from relevant professionals can also be powerful in pain management (physical therapists, chiropractors, psychiatrists, etc.).
Vaping Induced Lung Injuries
Vaping Trends: The appeal and the rise in popularity
What started as a product designed for cigarette smokers wanting to wean off the habit while still allowing them to have the physical ritual of smoking, vaping has now become a cultural phenomenon. Minimal odor, sleek packaging, and few, if any, regulations about when and where people can vape created an appeal even to those who had never used nicotine before and the market quickly turned its attention to gaining new customers through the addition of flavors, additives like THC, and devices that look like flash drives.
The use of electronic cigarettes involves a battery-operated device and a cartridge of nicotine-containing liquid. The liquid is heated into an aerosol which is then inhaled (or vaped). The devices are most popular among adolescents, with 27.5% of high schoolers having used e-cigarettes in the last 30 days in a 2019 survey (1). Adults are using them too, with as many as 2.8% of US adults regularly vaping in 2019, many of whom had never even been cigarette smokers (1).
One of the main reasons vaping has become so popular so quickly is because of the common misconception that it is a low-risk alternative to cigarette smoking, with many companies claiming fewer toxins and not including complete ingredient lists. While e-cigarettes do contain fewer chemicals than traditional cigarettes, they are by no means a “healthy” alternative and contain their own slew of ingredients, including heavy metals such as nickel and lead, glycerin, carcinogens, and nicotine, which is a highly addictive substance (8). The nicotine level in the cartridges is also extremely high, with a typical “pod,” or cartridge, containing the same amount of nicotine as a package of cigarettes (6). This is enough to make even casual users quickly addicted. The FDA has cracked down on these loopholes in recent years, now requiring warning labels and attempting to regulate the production of flavors, but the popularity of vaping has already exploded and the effort to reverse the trend is an uphill battle.

Self Quiz
Ask yourself...
- What prior knowledge did you have about vaping and its posed dangers?
- What vaping induced lung injuries were you aware of?
- What are some misconceptions surrounding vaping, as well as vaping induced lung injuries, that have led to increased popularity?
Health Risks
EVALI (e-cigarette or vaping induced lung injury).
Not surprisingly, the increase in vaping has been followed by a rise in health issues for the users. Most notably among emerging illnesses (and in the media recently) is lung damage referred to as e-cigarette/vaping associated lung injury, or EVALI (2).
A recent Morbidity and Mortality Weekly Report classifies EVALI as a diagnosis of exclusion as there is currently no specific testing for the illness, but it is one that should be considered early in the presentation of symptoms to not delay treatment (3). Most patients affected presented with cough, chest pain, and dyspnea, with many others having fever, chills, weight loss, vomiting, or diarrhea. At least 30% of patients presented with an oxygen saturation of less than 95%. Tachypnea was not frequently noted, but tachycardia was common. Xray revealed abnormal lung findings in 82% of patients and CT of the lungs was abnormal in 96% (3). This emerging issue is placing significant burden on the healthcare system, as most of these patients require inpatient management with steroids and supplemental oxygen, at least for the first 24-48 hours.
When this diagnosis resulted in several deaths in mid to late 2019, it was met with panic in the media and general public as healthcare professionals scrambled to find what exactly about vaping was causing the decrease in lung function. Emerging evidence now strongly suggests that the injury to the respiratory tract is caused by Vitamin E acetate, an additive in many e-cigarette pods (3). Fluid collected from symptomatic patients’ lungs was found to contain Vitamin E acetate in most cases and buildup over time is believed to be responsible for this lung injury (3). It is too early to rule out damage from other additives (like the glycerin used for flavoring) and researchers note that while these components are safe for oral consumption and often found in food, the effects of inhalation have not been studied and frequent exposure to the lungs should not be considered safe (4).
For now, though, Vitamin E acetate is considered the main culprit and is most commonly found in cartridges containing THC, particularly those made informally by people at home rather than those purchased from a manufacturer (3).
While all vaping should be avoided, for those who do use e-cigarettes it is safest to avoid cartridges containing THC and home-made cartridges.
Other Health Concerns
In addition to the potentially lethal complications of EVALI, routine nicotine use of any kind can have serious health implications, and e-cigarettes are no different. Cardiovascular health is affected, with increased heart rate and blood pressure within minutes of nicotine use. Risk of heart attack, stroke, chronic cough, compromised immune system, and impaired oxygenation, all are increased. Nicotine’s effects on a young, developing brain are well documented as well, with attention problems, impulse control issues, and an increased addiction response all posing serious risks to teens who vape regularly (6). Substance use of any kind is closely tied to mental illnesses such as anxiety and depression as well as ongoing struggles with addiction and substance abuse throughout adulthood (6).
The risk of cancer is also not solely tied to traditional cigarettes, with many substances found in e-cigarettes believed to be carcinogenic. A 2018 study tested urine and saliva samples from vaping teens and found the levels of carcinogens present to be significant and concerning (7). In general, the belief that vaping is a low-risk alternative to cigarettes is grossly erroneous.

Self Quiz
Ask yourself...
- Based on the presented evidence, what is the cause of EVALI?
- What are the overall effects of nicotine on the body?
What Can Healthcare Providers Do?
Screen for Vaping Use
One of the best ways to prevent vaping related health issues is to ensure that patients do not start vaping in the first place. Pediatric providers or those working with children and teens 11 years and older are in a particularly advantageous position to start the conversations early and often. Ask questions about what they know about vaping, if they have any friends who vape, and if they themselves have tried vaping. Try to maintain a non-judgmental attitude and allow them to lead the conversation. Provide education to patients and their parents about the dangers and health risks of vaping. Talk about the strengths of the student (academics, sports, arts) and discuss how a nicotine addiction or disciplinary action for vaping at school could negatively impact these enjoyable activities. For any patients who are already vaping, create a plan for cessation (discussed below). Adult patients and established cigarette smokers should also be screened for vaping and health risks discussed (2).
Early Detection of Vaping Related Lung Injury
Screening for vaping is not only important at routine wellness visits, but also for acutely ill patients in the outpatient, inpatient, and emergency room settings. Any patient presenting with cough, chest pain, or other respiratory symptoms should be questioned about current or recent vaping habits, including the use of THC pods. Chest x-ray should be strongly considered in the workup for anyone with respiratory symptoms and a history of vaping, particularly those with a pulse oximetry <95%. Flu and pneumonia should be considered in the differential diagnosis, as vaping increases the risk of both illnesses. In patients hospitalized or treated outpatient for a suspected EVALI, close follow up for the first few weeks is recommended (2).
Cessation
For patients with or without acute lung injury related illness, vaping cessation should be counseled. For adults, many employers will offer smoking-cessation incentive programs which have been shown to be effective. Encourage your patients to ask their employer if this is offered and if they qualify. There are multiple nicotine products designed to help wean slowly from nicotine with the ultimate goal of cessation such as gum, patches, and lozenges. Either gain familiarity with prescribing these yourself or find a local provider who you can refer your patients to for these products (5). Psychotherapy or counseling can be beneficial for patients trying to break an addiction and there are typically addiction counselors available at mental health facilities. There is a Substance Abuse and Mental Health Services Treatment Locator tool that can be found at https://findtreatment.samhsa.gov/ or patients can call 1-800-662-HELP (4357) to find the nearest resources (1). Finally, if you have patients using vaping as a method of stopping cigarette smoking, you should counsel that this is not a long-term solution and has no current supportive evidence as an effective smoking cessation tool. The risks of vaping far outweigh any perceived benefits and vaping should not be counseled as a method of smoking cessation.

Self Quiz
Ask yourself...
- What tools can providers give vapers to help with cessation?
Case Study
Austin is a 19-year-old male presenting to the ED with 6 days of coughing, fever, lethargy, decreased appetite, and (in the last 2 days) increasing chest pain, particularly with deep inspiration.
He is a student at the local university with a history of ADHD for which he takes 20mg of Adderall XR daily. No other pertinent medical history and no other medications. He reports drinking socially on the weekends.
Vital signs are as follows: Temp: 100.9, HR: 147, BP: 134/85, RR: 20, SPO2: 87%. Physical exam reveals pallor, diaphoresis, diminished air exchange in all lung fields with crackles in the bases. Deep inspiration results in coughing fits with no improvement or clearance of crackles and rhonchi. He is most comfortable in the tripod position, but overall is restless. CBC with differential is normal, flu swab is negative. Chest x-ray reveals bilateral infiltrates.
The nurse notices a Juul device in the clear plastic bag of the patient’s belongings and when asked, he admits to vaping ¾-1 cartridge per day for 2 years. He also states he will use a THC cartridge 2-3 times per week with friends.
He is diagnosed with EVALI and admitted for treatment with corticosteroids and supplemental oxygen. He is discharged in stable condition after 2 days with scheduled follow up in 1 week. He is counseled on vaping cessation, particularly of THC cartridges, and makes a full recovery over the next 2 months.
Conclusion
Vaping is a fairly new trend and health risks are still emerging as the number of people using e-cigarettes grows. Staying abreast of trends in vaping and the growing information about symptoms, treatment, and causes of EVALI are important responsibilities of healthcare providers. Early detection of vaping related illnesses is key to best treatment outcomes and screening for vaping should become a routine part of all healthcare exams, both preventive and acute.
LGBTQ Cultural Competence
Introduction
Lesbian, gay, bisexual, transgender, and questioning (LGBTQ) individuals represent a rapidly growing segment of the U.S. population [1]. This rapid growth brings with it risk for stigmatization [1]. Implicit physician biases may result in LGBTQ patients receiving a lower standard of care or restricted access to services as compared to the general population [2]. Even when institutions and providers make commitments to equitable care explicit, implicit biases operating outside of conscious awareness may undermine that commitment. There is an urgent need to ensure that health care providers are prepared to identify and address their own implicit biases to ensure they do not contribute to the health care disparities experienced by LGBTQ and other vulnerable populations. Only by addressing their own implicit biases will health care providers be able to provide patient care in accordance with LGBTQ cultural competence.
LGBTQ individuals face significant disparities in physical and mental health outcomes [3]. Compared to their heterosexual counterparts, LGBTQ patients have higher rates of anal cancer [4], asthma, cardiovascular disease [5,6,7,8], obesity [6], substance abuse [8,9,10], cigarette smoking [11], and suicide [12]. Sexual minority women report fewer lifetime Pap tests [13,14,15], transgender youth have less access to health care [16], and LGBTQ individuals are more likely to delay or avoid necessary medical care [17] compared to heterosexual individuals. These disparities are due, in part, to lower health care utilization by LGBTQ individuals [3, 18,19,20]. Perceived discrimination from health care providers and denial of health care altogether are common experiences among LGBTQ patients and have been identified as contributing factors to health disparities [21,22,23,24]. Disparities in health care access and outcomes experienced by LGBTQ patients are compounded by vulnerabilities linked to racial identity [25,26,27] and geographic location [28].
Biases among health care professions students and providers toward LGBTQ patients are common [29, 30] despite commitments to patient care equality. These biases, also known as negative stereotypes, may be either explicit or implicit [31]. These biases contribute to a lack of LGBTQ cultural competence in patient care. A large study of heterosexual, first-year medical students demonstrated that about half of students reported having negative attitudes towards lesbian and gay people (i.e., explicit bias) and over 80% exhibited more negative evaluations of lesbian and gay people compared to heterosexual people that were outside of their conscious awareness (i.e., implicit bias) [29]. Research in social-cognitive psychology on intergroup processes defines explicit biases as attitudes and beliefs that are consciously accessible and controlled; they are typically assessed via self-report measures and are limited by an individual’s awareness of their attitudes, motivation to reveal these attitudes, and ability to accurately report these attitudes [32, 33]. In contrast, the term implicit bias refers to attitudes and beliefs that are unconscious (i.e., outside of conscious awareness) and automatic [34, 35]. Implicit bias can be assessed with the Implicit Association Test (IAT) [36], which measures the strength of association between concepts [37].
Health care provider biases are correlated with poorer access to services, quality of care, and health outcomes [31, 38,39,40]. Explicit biases held by health professionals towards racial/ethnic minorities, women, and older adults are known to affect clinical assessments, medical treatment, and quality of care [41]. Importantly, implicit bias measures are more strongly associated with real-world behaviors than explicit bias measures [42] and are linked to intergroup discrimination [43]. Health care provider’s implicit biases towards vulnerable patient groups may persist despite an absence of negative explicit attitudes [44], resulting in preconceived notions about patient adherence, poor doctor-patient communication, and micro-aggressions, all of which can interfere with optimal care. With less time and limited information processing capacity, provider’s decisions are increasingly governed by stereotypes and implicit biases [45]. Medical student and provider biases may contribute to health disparities in vulnerable populations by negatively impacting communication with patients and decisions about patient care [33, 35]. Taken together, these findings suggest that medical students and healthcare providers are likely to underestimate or to be unaware of their implicit biases towards LGBTQ patients, particularly when they are rushed or fatigued, which could impact their behavior and judgments in ways that contribute to health disparities experienced by LGBTQ populations. By learning about and addressing their implicit biases, health care providers can work towards demonstrating LGBTQ cultural competence and providing optimal care (Introduction section courtesy of Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P.- reference 45).

Self Quiz
Ask yourself...
- What are some cultural misconceptions regarding the LGBTQ community and providing medical care?
- How can you demonstrate LGBTQ cultural competence in everyday practice?
Terminology
Understanding the standard terminology utilized is pivotal to treating and interacting with LGBTQ patients. Below are listed some of the common terms and how they should be referenced.
Ally – A person not identifying as LGBTQ, but who promotes equality and support of LGBTQ peoples in a variety of ways.
Androgynous – Identifying as neither masculine nor feminine.
Bisexual – A person who is emotionally, romantically, or sexually attracted to more than one sex, gender, or gender identity.
Cisgender – A person who identifies with their gender which as assigned at birth. For example, a person assigned female gender at birth who identifies as female.
Gay – A person who is emotionally, romantically and/or sexually attracted to those of the same gender.
Gender-fluid – A person who identifies as a fluid or unfixed gender identity.
Lesbian – A woman who is emotionally, sexually, and/or romantically attracted to other women.
LGBTQ – Acronym for “lesbian, gay, bisexual, transgender, and queer.”
Non-binary – Adjective describing person(s) who do not identify exclusively as man nor woman.
Pansexual – A person who has the potential for romantic, emotional, and/or sexual attraction to people of any gender.
Queer – Often used interchangeably with “LGBTQ,” or to express fluid identities or orientations.
Sexual orientation – An inherent or enduring emotional, romantic, or sexual attraction to other people.
Transgender –Umbrella term for people whose gender identity and/or expression is different from cultural expectations based on the sex they were assigned at birth. It does not imply any specific sexual orientation and transgender persons may identify as straight, gay, lesbian, bisexual, etc.
*Definitions largely derived from (46).

Self Quiz
Ask yourself...
- Which of the above definitions have you heard used interchangeably?
Best Practices
Below we will list and discuss the best practices for ensuring a positive, equitable healthcare experience for LGBTQ persons, according to the Joint Commission (this is not a comprehensive list, just highlights).
Create a welcoming environment that is inclusive of LGBT patients and demonstrates LGBTQ cultural competence.
- Prominently display the hospital nondiscrimination policy and/or patient bill of rights.
- Waiting rooms and common areas should be inclusive of LGBTQ patients and families.
- Unisex or single-stall restrooms should be available.
- Ensure that visitation policies are fair and do not discriminate (even inadvertently) against LGBTQ patients and families.
- Foster an environment that supports and nurtures all patients and families.
Avoid assumptions about sexual orientation and gender identity.
- Refrain from making assumptions about a person’s sexual orientation and/or gender identity.
- Be cognizant of bias, stereotypes, and other communication barriers.
- Recognize that self-identification and behaviors do not always align.
Facilitate disclosure of sexual orientation and gender identity but be aware that disclosure is an individual process.
- Honor and respect patient’s decisions to provide or not provide sexual and/or gender information.
- All forms should contain inclusive, gender-neutral language that allows patients to self-identify.
- Use neutral and inclusive language when communicating with patients.
- Listen to and respect patients’ choice of language when they describe their own sexual orientation.
- Conduct confidential patient satisfaction surveys that include questions regarding sexual orientation and gender identity.
*Information largely derived from Joint Commission field guide, reference 47.
For more information on best-practices in the workforce, visit the Joint Commission website by clicking here.

Self Quiz
Ask yourself...
- Have you ever misused a pronoun, or overheard a co-worker misuse a pronoun in practice?
- How can you make sure this doesn’t happen again?
Establishing Relationships with LGBTQ Patients
When interacting with patients, one should not assume gender or sexuality. Addressing a patient who identifies as a female as a male can cause grave harm to the relationship. Instead, nurses should use open-ended questions. For example, rather than saying “Hi sir, what brings you to the hospital,” a nurse might say, “Welcome, what brings you to the hospital today (48)?”
If a nurse uses the incorrect pronoun, the best practice is to apologize and ask the patient what pronoun and name they prefer. For example, a nurse may say, “I apologize for assuming your gender. How would you like to be addressed? (48).
In conversation, the nurse should use the name and/or pronoun the patient prefers without drawing special attention to the subject (48). For example, if a male patient prefers to be identified as his partner’s wife, you should follow suit.
The core of relationship-building with LGBTQ patients is no different than any other patient, fundamentally. If nurses have a basic understanding of best practices and a healthy dose of respect and compassion for LGBTQ patients, a positive relationship is likely to develop.

Self Quiz
Ask yourself...
- Do you have any biases which may affect the care you provide to LGBTQ patients?
- Have you worked for someone who did NOT demonstrate LGBTQ cultural competence?
- In what ways could they improve their practice?
Health Disparities of LGBTQ Patients
LGBT Americans are at higher risk of substance use, sexually transmitted diseases, cancer, cardiovascular disease, obesity, bullying, isolation, anxiety, depression, and suicide when compared to the general population (49). LGBT youth are frequently bullied at schools (49). In fact, early victimization and subsequent emotional distress accounted for 50% of the disparities between LGBT youth (49). In other words, LGBT Americans are discriminated against and disadvantaged from a very young age.
When home life also reflects a lack of LGBTQ cultural competence, more problems arise. A major cause of LGBT distress is family rejection. Disclosure of gender identity or sexuality can cause very significant interpersonal conflicts among family and friends of LGBT persons (49). This explains some hesitancy and should help nurses understand the importance of respecting privacy, while giving options to patients about disclosing sexuality and gender.

Self Quiz
Ask yourself...
- Are there any circumstances in which your current hospital’s policies could discriminate against LGBTQ families?
- If so, how would you begin to work with leadership to change those policies, so they reflect LGBTQ cultural competence?
Providing an Inclusive and Accepting Care Environment
LGBTQ patients often experience difficulty in finding healthcare environments in which they feel accepted and understood (48). Past negative experiences, lack of knowledge among healthcare providers, and limited access to healthcare in general may become major barriers for LGBTQ persons when seeking care (48).
The core tenant of providing an inclusive environment is understanding the needs of LGBTQ patients and working diligently to create an environment which does not disadvantage or discourage them from seeking care.
Policies and procedures at institutions should be designed to reflect a non-discriminatory environment. For example, many hospital policies dictate that only legal family spouses or partners can visit in specific circumstances. Policies such as this are inherently discriminatory toward LGBTQ patients, as they may not have legal spousal status due to social, legal, or personal reasons.

Self Quiz
Ask yourself...
- Have you ever had an experience where a colleague made a derogatory remark about a patient, based on sexual orientation or gender status? If this happened to you, how would you handle that situation differently?
- Think about the structure of your facility. Does it create an environment which minimizes friction and discrimination of LGBTQ patients?
- Do you feel there are any biases among healthcare staff?
- If so, how would begin addressing those?
Exercises on LGBTQ Cultural Competence
To help solidify your learning, please complete the following exercises at your own pace. The answers/guidance for each are provided below.
Scenario 1
A patient enters your emergency department, and you assume the patient identifies as a female. You introduce yourself and say, “Ma’am, how can we help you? What brings you in today?”
The patient appears dismayed but answers the question. The nurse is confused and does not understand why the patient appears distressed. What is the best course of action?
Answer: The nurse should apologize to the patient and ask the patient how they would like to be addressed. Then, the nurse should update the patient’s records to reflect such, to reduce further confusion.
If the nurse does not address the issue, the patient may feel uncomfortable and develop a negative association with healthcare, which can lead to disparities in the future.
Scenario 2
A patient in your ICU has had a deterioration while his husband was in the room. After a family meeting, a member of the healthcare team makes a derogatory remark about the patient’s sexuality. What is the next best action for the nurse?
Answer: Pre-conceived phobias and stigmatizations can cause significant distress to LGBTQ patients, even if not stated directly to them. These types of remarks are abusive and should not be tolerated. The nurse should confront the co-worker (if safe) and consider reporting the comments to the Human Resources department.
Scenario 3
A LGBTQ patient is being admitted and prefers not to disclose their sexuality. However, the nurse is unable to proceed with the admission process without this information. What could be done to rectify this system-level issue?
Answer: The nurse should work with administration to ensure that all charting and paperwork allows individuals to self-report sexuality and/or gender if they want. However, healthcare systems should not force patients to “come out” unless it is absolutely medically necessary.

Self Quiz
Ask yourself...
- What information from this course can you take to your facility to encourage a positive change of LGBTQ patients, and create an environment for LGBTQ cultural competence?
Conclusion
LGBTQ cultural competence must be ingrained in our healthcare systems in order to foster excellent relationships between members of the LGBTQ community and medical staff. Hospitals and healthcare systems have a great deal of work to do in becoming LGBTQ-friendly. The efforts must continue until LGBTQ patients and families do not feel disadvantaged, anxious, or frustrated when interacting with healthcare systems. As the patient’s ultimate advocate, nurses are at the front-line and should advocate for patients both individually and from a policy perspective. Nurses should work with and spearhead efforts to ensure that healthcare policies reflect best-practice and do not discriminate against LGBTQ patients in any way.
Coronavirus: Nursing Considerations
Introduction
The outbreak of the Coronavirus and its slow spread into the United States have caused panic throughout the world over the course of a year. This has caused stress, panic, worry, isolation, and death, leading to many structural breakdowns within the healthcare system, government, and families throughout the world and, more specifically, the United States.
As a healthcare provider, it is imperative to stay informed and up to date on the latest trends, evidence-based practice, and protocols relating to the COVID-19 pandemic as it continues to evolve. As healthcare providers, we are burnt out—mentally, physically, and emotionally—however, it is still our duty to remain steady, and deliver high-quality care to every patient, every time.
What is the Coronavirus? Specifically, what is SARS-COV-2?
Coronaviruses are a group of viruses that have been known to cause moderate to severe respiratory symptoms that may mimic influenza. These symptoms include cough, runny nose, sore throat, body aches, and pneumonia.
Coronaviruses have been affecting humans for several years, but there has not been an outbreak of epidemic proportions since the SARS epidemic of 2003. Coronaviruses are aptly named for the crown-like appearance the virus takes on when examined under a microscope (“corona” is Latin for “crown”) (1). Coronaviruses can range from asymptomatic, to causing symptoms of the common cold, to more severe disease such as severe acute respiratory syndrome (SARS).
In late December of 2019, several cases of unknown origin were reported out of China, which in early January 2020 were announced to have been caused by a novel coronavirus. This virus was later deemed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Despite attempts to contain the disease within its country of origin, the virus has now spread globally, and COVID-19 was declared a pandemic by the World Health Organization in March of 2020.
Signs and Symptoms
The coronavirus disease affects each person differently. Many patients will experience mild disease, while others may develop more severe respiratory symptoms that require hospitalization. Patients present to the emergency department with a variety of symptoms. Nurses have the responsibility to appropriately triage patients, based on severity of the illness, to assist in the efficiency of managing a higher influx of patients, while simultaneously preventing the viral spread of the infection to those patients who have not yet been exposed to COVID-19.
The prevention of an overwhelmed healthcare system includes highly skilled clinical assessment in conjunction with various laboratory and imaging testing, including chest x-ray, blood analysis, and testing for the identification of SARS-CoV-2.
Symptoms include:
- Fever
- Cough
- Shortness of breath
- Headache
- Sore throat
- Nausea/vomiting
- Runny nose
- Myalgia
- Abdominal Pain

Self Quiz
Ask yourself...
- Have you, a friend, family member or patient been diagnosed with COVID-19?
- How did your signs and symptoms compare or differ to each other’s and to the “general” symptoms listed?
Preventative Actions
There are several ways to contribute to the prevention of the spread of COVID-19, including per the Centers for Disease Control and Prevention (CDC, 10):
- Avoid touching eyes, nose, and mouth.
- Avoid close contact with people who are sick.
- Stay at home when you are sick.
- Cover your cough or sneeze with a tissue, then dispose of it properly.
- Use a face covering when physical distancing.
- Clean and disinfect frequently touched objects and surfaces.
- Perform hand hygiene with soap and water or use alcohol-based sanitizer.
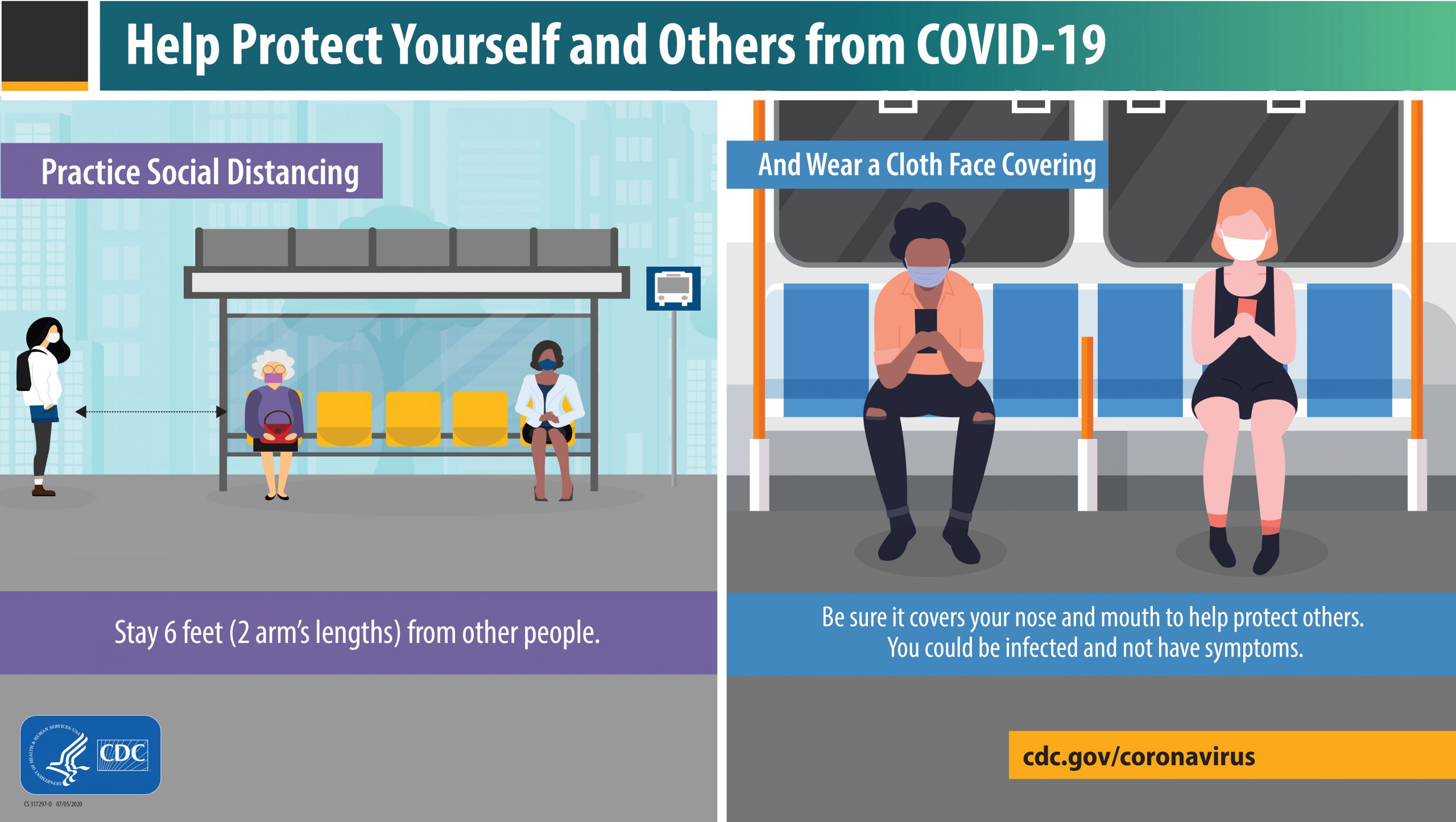
What is Considered Close Contact?
Understanding the distinction of close contact is important in the context of triaging and discharging patients; not all exposures are considered close contact.
Please see the criteria below for determining a high-risk exposure (10):
- Patient was within 6 feet of a person with confirmed COVID-19 for a total of 15+ min within a 24-hour period.
- Patient has cared for someone at home who is sick with COVID-19.
- Patient has shared food or drinking utensils with a person with confirmed COVID-19.
- Patient had direct physical contact with a person with confirmed COVID-19 (hugging or kissing).
If someone who has tested positive within the last three months for COVID-19 and recovered has been in close contact with a patient who has suspected or been diagnosed with COVID-19, they do not have to re-test unless they develop new symptoms.
*Those awaiting test results should self-quarantine.
Quarantine vs. Isolation. What is the Difference?
Quarantine: refers to keeping someone who has been exposed away from others to prevent potential spread.
Isolation: refers to keeping those actively infected away from other individuals to reduce spread. This keeps someone infected with the virus away from others, even in their home (10).
Current Guidelines for Quarantine and Isolation
Who Should Quarantine?
Patients should quarantine at home if they have been in close contact with someone who has tested positive for COVID-19, excluding those who have had COVID-19 in the past 3 months (10).
Ideally, patients should stay home and monitor for symptoms for 14 days after their last exposure to a close contact. Recognizing that this can be difficult, the CDC allows options for reducing quarantine time (see below).
If possible, instruct patients to stay away from those at high risk of severe illness from COVID-19.
Options to Reduce Quarantine
These guidelines have been released by the CDC, giving the authority to reduce quarantine to the local health departments (10). The theory behind reducing quarantine is that it will increase compliance and minimize the burden on society, while balancing a reduction in virus spread. However, it is important that patients understand the importance of proper quarantine.
Patients who are exposed and do not develop symptoms may end quarantine 10 days after exposure if no test is administered.
Patients who are exposed and do not develop symptoms may end quarantine 7 days after exposure and after receiving a negative test (test must occur on or after day 5).
*If patients develop symptoms during quarantine, even with a negative test, they should be considered COVID-19 positive.

Self Quiz
Ask yourself...
- Have you heard the terms “quarantine” and “isolation” being used interchangeably?
- Have you been told similar or different protocols in managing your personal or family’s COVID diagnoses?
Options for Testing
There are several different tests available for COVID-19. They can be used for diagnosing acute infection, to guide contract tracing, and in some cases to determine if a patient has previously been infected by the SARS-CoV-2 virus. It is important for nurses to understand the limits of testing.
Testing for active infection (symptomatic or asymptomatic) is an important strategy for controlling the spread of the virus. It is important to know when it is appropriate to test a patient.
In general, testing should be considered for the following:
- People with symptoms of COVID-19
- People who have close contact with someone who is COVID-19 positive.
- People who are asked or referred by their healthcare provider or local health department.
*Patients with recent COVID-19 disease (past 3 months) do not require testing for subsequent exposures unless symptoms are present.
**Based on CDC data (3).
Viral Test
Viral tests are diagnostic and use samples from the respiratory system, such as nasal or oral swabs, to determine the presence of infection with SARS-CoV-2.
- This type of test tells you if a patient is currently infected with the disease.
- Recommended to diagnose acute infection in symptomatic and asymptomatic patients.
There are currently two types of authorized SARS-CoV-2 viral diagnostic tests that use different technological principles: molecular and antigen. Each of these detects a different part of the SARS-CoV-2 particle.
Antibody Test
- This type of test can show you if a patient was previously exposed or infected with SARS-CoV-2 and carries the antibodies.
- Detects the presence of IgG or IgM against SARS CoV-2.
- Not authorized by the Food and Drug Administration (FDA) to diagnose SARS-CoV-2 infection.
- Used to support a clinical assessment of persons who present in the later stages of illness when used in conjunction with viral testing (2, 3, 4).

Self Quiz
Ask yourself...
If you tested positive for COVID-19 two months ago, but were exposed to a positive patient, within 6 feet without a mask on, is the current recommendation
to get a COVID test?
Pharmacologic Treatment
For pharmacological treatment, it is important to understand that we are in our infancy of understanding SARS-COV2-2 and COVID-19 infection. Though there are a plethora of low-quality studies demonstrating benefit for some agents, most experts feel that we should wait for more conclusive data before utilizing agents on a large scale.
- Remdesivir is currently the only drug approved by the FDA for the treatment of COVID-19. It is recommended for non-intubated hospitalized patients requiring supplemental oxygen.
- Dexamethasone is the only recommended treatment in patients requiring increasing amounts of supplemental oxygen and in intubated patients.
Diagnosis and Management
Imaging can be useful in the diagnosis and prognosis of COVID-19 but is not required for a clinical diagnosis. Early in the disease, imaging may not correlate with the severity of the disease.
Because COVID-19 usually manifests itself as pneumonia, radiological imaging has a profound role in assisting the diagnosis of the disease, management, and follow up. In the early stages of the disease process, the results can be un-impressive and assumed as negative findings (5). In the advanced stages, radiological findings typically reveal patchy ground-glass opiates, with infiltrates favoring the bases and periphery of the lung fields. The infiltrates are typically bilateral, and pleural effusions can be present (6). Lung inflammation may progress to the level of fibrosis in respiratory failure (5).
Patients with COVID-19 experiencing hypoxia should receive supplemental oxygen with a target oxygen saturation of 92% to 96% (18). Patients requiring oxygen fall into the category of moderate-critical illness of COVID-19. Severe illness in COVID-19 patients typically occurs one week after symptom onset. The most common symptoms presenting in these patients are dyspnea accompanied by hypoxemia (9). These patients with severe disease usually require supplemental oxygen and should be monitored closely for respiratory status because these patients may be at risk for progressing to critical illness with acute respiratory distress syndrome (ARDS).
COVID-19 Vaccines
Currently, three vaccines are authorized and recommended to prevent COVID-19 in the United States
- Pfizer/BioNTech’s COVID-19 vaccine (mRNA)
- Moderna’s COVID-19 vaccine (mRNA)
- Janssen Covid-19 vaccine (adenoviral vector)
Many people have questions related to the new COVID vaccines. As healthcare providers, you play a critical role in helping patients to understand the vaccine and the varying risks and benefits.
All vaccines are recommended for intramuscular injection into the deltoid.
The mRNA vaccines are recommended for two doses one month apart.
The adenoviral vector vaccine is recommended as a single dose administration.
Effects of Long COVID
Although it may feel like COVID-19 has been around for quite a long time, the reality is that our understanding of the disease is just getting underway. As the pandemic continues to progress, there is a growing recognition that people are experiencing the long-term repercussions of the SARS-CoV-2 virus, which may persist for months or even years.
Contrary to widespread belief, health status is not protective against developing Long COVID. Current data shows that young, healthy patients experience Long COVID at similar rates to those with advanced age and poor health status. Even those with mild to moderate illness not hospitalized are showing delayed or long-term symptoms (7).
We are slowly learning more about how COVID-19 is chronically affecting patients. The long-term effects are not limited to the lungs and have been reported to affect all organ systems. The most common symptom reported is crippling fatigue. You can find a list of the common Long COVID symptoms in the chart below (7).
COVID-19 Variants
All viruses mutate over time—some mutate more than others. A new strain occurs when there is a mutation in the genes of the virus. There have been three new strains of the virus seen throughout the world to date since September of 2020. The mutations in the new strains are affecting spike proteins, which are on the surface of the SARS-CoV-2 virus, which gives it its “spiny” appearance. These proteins allow for the virus to attach to human cells and invade the body, leading to illness (8).
One of the main concerns is whether any of the variants could affect treatment and prevention. Mutations may allow the coronaviruses to escape the antibodies in currently available therapies and those induced by vaccines. There is new evidence from laboratory studies that some immune responses driven by current vaccines could be less effective against some of the new strains. It is not yet known if those who have already received the COVID-19 vaccine could get sick with the new variants (8).

Self Quiz
Ask yourself...
What are the three different types of COVID-19 vaccines approved by the Food and Drug Administration for COVID prevention?
Have you, a family member, or patient experienced lasting symptoms of COVID-19 or other symptoms that can be categorized as a long-term effect of COVID-19?
Conclusion
As time continues, and we as a country and world try to manage our day to day lives with the current and aftereffects of the pandemic, it is imperative that nurses be up to date and armed with the latest knowledge of the virus in order to manage and care for their patients efficiently and effectively. Improving patient outcomes and saving lives of patients experiencing current or long-term effects of the SARS-CoV-2 virus.
Effective Communication in Nursing
Introduction
Communication in nursing is key, and the ability to communicate effectively can be our lifeline. We depend on ourselves and others to be fluent and effective in the art of communication in order to perform our role as nurses successfully. When any link in our communication chain fails, we immediately see poor outcomes, wastage of resources, reductions in patient and staff satisfaction as well as a decline in the quality of patient care (1).
Types of Communication
In order to master effective communication in nursing, it is important to understand the various types of communication, their definitions, and the impact they can make.
Non-Verbal
This form of communication relies solely on the utilization of body language, including body and facial mannerisms, and completely lacks spoken words or sounds (2). We perform and identify non-verbal communication in nursing daily without giving it a second thought. We may see a newborn sucking on their hands, providing us a non-verbal cue that they are hungry. When assessing a patient holding their abdomen, we would look to initially target that area because they have communicated (non-verbally) that this is where they are experiencing discomfort. Smiling when the next shift nurse is walking in the door communicates to them that you are happy to see them, and that it’s about time for you to go home!
Since we perform non-verbal communication so often, it can become an incredibly powerful tool or an extremely negative one. This form of communication in nursing can be used positively to show our patients and co-workers that we have compassion, and we are engaged. Negative forms can make patients uncomfortable with sharing their medical history and result in a lower quality of patient care. Additionally, it can lead to dysfunctional teamwork among staff.
Verbal
Verbal communication occurs when we use words or sounds to discuss concepts with others (2). This form of communication in nursing has the conception to be a very easy notion, but it can create unfavorable consequences when used ineffectively. In order to produce clear verbal messages, we should always speak concisely and with confidence. As health care professionals, we have our own language, and understanding when to incorporate our medical jargon into conversations versus when to not is crucial in providing care. When communicating among co-workers, our medical knowledge can display professionalism and it is evident that they can follow along. However, when speaking with patients and their families, this may not always be the case and we must be able to effectively gauge our audience and ensure that they have a clear understanding of what we are teaching or explaining; this is an extremely valuable tool.
Written
This form of communication can be either a formal or informal transcription of words that are intended to serve as a direct communication form (2). Written communication in nursing is used daily and incorporates one of our most important duties, documentation. Throughout our nursing practice, we have learned the importance and necessity of our documentation; it can be useful for legal protection or provide critical data to other health care professionals. Written communication can also be accessed through the policies and procedures we employ to perform various tasks. Having sound, written communication, and interpretation skills is vital to the overall success of our nursing career.

Self Quiz
Ask yourself...
- What type of communication is being interpreted while watching a patient walk to the bathroom?
- Upon admission of a female patient for a fall, you are performing normal intake questions and a physical assessment. The patient is quiet and uses minimal verbal communication and looks down at the floor while you are in the room. What communication types are you interpreting?
Receiving Communication
The most common communication perception is usually directed to producing communication through non-verbal, verbal, or written forms. While the production of communication is important, the reception of it potentially holds even greater value. In nursing, ensuring our communication is received correctly affects every clinical, orientation, or job experience we have encountered thus far. Think about it…
- Taking notes in class or during a shift.
- When a preceptor or instructor educates you on a brand-new skill or piece of equipment.
- Teaching your patient, family, or student about a new diagnosis.
- Watching your patient breathe for rate, depth, and effort.
We must provide and receive communication in nursing through verbal, non-verbal, or written forms successfully. If communication fails, we will experience extremely negative effects throughout our entire nursing system.
Hearing & Listening
Hearing describes the process or act of perceiving sounds or spoken words (2). We hear sounds upon auscultation, varying frequencies of alarms, and patient concerns when they are voiced. Hearing all these sounds are heavily dependent on how they are used. To achieve successful implementation of these sounds, we must also listen to these sounds and words. To listen, we must hear and then interpret these sounds carefully (2). We interpret these sounds and words by asking additional questions, performing additional assessments, or paraphrasing the information presented.

Self Quiz
Ask yourself...
- What is the best way to ensure a patient was actively listening while performing patient education?
- Which type of scenario requires active listening skills?
a. Putting blood tubing into a pump.
b. Watching an EKG monitor.
c. Performing a pain assessment. - What techniques show others you are actively listening?
a. Reading a document while being talked to.
b. Making eye contact.
c. Making noises while someone is talking.
Communication Transmission Threads
Communication in nursing occurs multiple times a day between a wide range of communication threads. The type of communication through non-verbal, verbal, and written communication produced and received, must be effectively performed. Success and implementation are heavily dependent on the communication between the nurse and the communication thread.
Nurse-Nurse
Communication among nurses is continuous throughout a shift while working within a team environment. Whether it is us passing our documentation on to another nurse for review or vice versa, there is consistent communicative flow of all variants (non-verbal, verbal, and written) between the team in order to provide care for patients.
Nurse-Ancillary Staff
Your team members will vary depending on your nursing career setting, but some items will remain consistently important despite wherever you are. We must provide clear verbal communication when delegating or reporting critical information from the nurse to ancillary staff participating in patient, client, or resident care.
Charge Nurse-Team
When stepping into a charge nurse role, there will always be unexpected tasks, staff conflicts, or emergent situations. In this position, you will be taking all the communication skills you have acquired and putting them into practice at an all-time high. As the charge nurse, you will be viewed as a leader, meaning that you are a role model for your fellow team members. Now, in addition to producing and receiving communication effectively, you will now be identifying poor communication and assisting with its correction.
Nurse-Patient
The nurse-to-patient communication thread is one of the ultimate and most important exchanges in the nursing profession. Patients need us, so we must be able to keep consistent and effective communication flow with them because any assessment, report, and administration of medication is contingent upon it.
Nurse-Family
The thread between the nurse and the patient’s family can be the foundation for your nurse-to-patient communication and its effectiveness. The family could be the responsible party or guardian for your patient and could potentially serve as your sole historian for patient information if the patient is unable to communicate at the time of data collection. Ensuring that the family is aware of and understands discharge instructions can further help them to recognize any potential signs or symptoms that could result in calling a physician or visiting the emergency room in the future.

Self Quiz
Ask yourself...
- Which of the following is a beneficial way to ensure effective communication throughout multiple threads?
a. One to one conversation.
b. Reviewing a policy.
c. Bedside report.
Barriers & Improvements to Communication
Barriers of communication in nursing happen frequently and are sometimes out of our control. These barriers include:
Language Barriers
Utilizing available resources for language barriers through interpreter staff members or interpretation devices can ensure effective communication pathways between two individuals.
Cultural Differences
Identification of cultural differences during admission and cultural awareness will allow for effective communication management throughout each culture you are presented with.
Patient Acuity, Staffing Levels, Time Constraints
Patient acuity, staffing levels, and time constraints can be improved by utilizing staff huddles and working together with administration in order to overcome conflicts.
Emergent Situations
Emergent situations that arise during your shift can be relieved through adequate knowledge of the policies and procedures and by performing debriefs after the situation resolves. Debriefings hold valuable insight into reflections of the emergent situations we face as nurses, especially on communication performance.
In each thread and form of communication in nursing, we must remember the following items to receive information. While producing communication, we must always be clear, concise, and accurate with the correct corresponding tone when expressed to others. When we are receiving the information, we must ensure we are understanding, investigating, and acting according to the communication presented to us. Utilizing various communication platforms, including emails, boards, and group messaging apps, can help to assist in ensuring education is received.
Benefits of Effective Communication in Nursing
When we achieve effective and therapeutic communication between both our team and patients, it will create opportunities for enhancements throughout our practice. Fostering a unity of teamwork with co-workers will increase satisfaction and reduce burnout rates. Reduced health care costs through reduced readmissions or emergency room visits will be established by successful patient education and understanding. Our quality of patient care will be heavily influenced by the nursing communication threads created through their care.
Flu Treatment, Symptoms, and Red Flags
Introduction
Every year, emergency waiting rooms, outpatient clinics, and inpatient hospital beds fill up with patients seeking treatment for the miserable symptoms brought on by the influenza virus. This illness does not discriminate and afflicts all ages, from young babies to the elderly, and everyone in between. Symptoms can range in severity from several days of fever, chills, and cough in bed at home, to weeks of hospitalization, respiratory distress requiring mechanical ventilation, and even complications resulting in death.
Starting in October and often lasting well into spring, flu season tasks healthcare workers everywhere with promoting prevention, quickly and efficiently identifying those infected, and appropriately managing symptoms and any secondary complications that may arise.
An illness affecting the population on such a large scale requires healthcare professionals to stay up to date on disease trends, diagnosis and treatment protocols, and “red flags” of more serious cases in order to minimize the impact of flu season and keep complications and mortality as low as possible.
This course will review disease trends in recent years, common and more insidious symptoms to help identify flu infections, available testing methods and their accuracy, pharmacologic treatments and the importance of their timing, supportive treatments and symptom management, and the “red flags” of dangerous secondary infections and complications.
Upon completion of the course, the reader should be comfortable participating in prevention, identification, and management of the seasonal influenza virus.
Current Practice, Barriers and Need for Continued Education
Influenza is a serious global issue that has been affecting humanity since the beginning of recorded history. Despite medical advances in recent years, flu remains a major public health concern, with up to 20% of the US population being affected annually (13).
Over 200,000 people are hospitalized nationally each year, with around 36,000 deaths. This issue increases on a global level, with 3 to 5 million infections and over half a million deaths each year (14). Those most at risk are young children, those over age 65, and those with other chronic or underlying conditions such as asthma, diabetes, immunosuppression, etc.
Despite high rates of infection and risk of complications, the estimated annual vaccination rate amongst the general population remains low, around 37.1% for adults (3) and 57.9% for children for the 2017-2018 flu season (4). There is an increased rate of vaccination amongst healthcare workers (78.6%), but as these are the people most likely to encounter and spread the virus, even that number could be improved upon (6).
Further complicating the situation, influenza virus has several strains and possesses the ability to change its DNA (referred to as “drift and shift”) as it replicates, making it difficult to produce a highly accurate vaccine (2). Because of this, vaccines cannot be created far in advance if the most current strain is to be targeted. Vaccine shortages can result if new vaccines are not created at a fast enough rate throughout flu season (6).
There are antiviral medications available for prevention and treatment of flu, however this requires proper identification of those infected or most at risk for infection, and the administration of these medications is typically time-sensitive (5). Health care professionals should be familiar with common symptoms of flu and be comfortable assessing patients, testing for and diagnosing flu.
All these considerations for flu illustrate the intense need for educated, proactive health care workers to promote vaccines, quickly identify those most at risk or with active infections, and treat effectively to keep the impact of flu minimalized.
The National Institute of Health has ongoing projects to keep available resources robust (14), but this research is only as strong as the health care professionals who implement it and are on the front lines of patient care. Staying up to date on current practice is paramount for national and global management of this resilient pathogen.

Self Quiz
Ask yourself...
- Do you think that the current rate of vaccinations among healthcare providers (78.6%) could be improved?
- With up to 20% of the US population being affected annually, do you think enough resources are utilized in the prevention, recognition, and treatment of influenza?
- What could be done from a national, state, and local level to promote increased prevention, recognition, and treatment of influenza?
What is Influenza?
Viruses are small pathogens containing genetic material that infect host cells and replicate within that host. They can exist for short periods of time outside of a host as an infectious virion and are spread between hosts through a variety of ways. Influenza is a specific group of RNA viruses that replicate within the epithelial cells of the respiratory tract (15).
There are three main types of flu viruses (A, B, and C). Viruses B and C typically only exist in humans, but A has been found in other mammals such as pigs and horses (15). There are also subtypes of each virus, depending on specific structure of the virus; these are labeled as H1-16 and N1-9 for hemagglutinin and neuraminidase, however, further discussion of these is beyond the scope of this course (15).
As the virus replicates within host cells, there can be subtle changes to the RNA over time, eventually adding up to more noticeable changes and resulting in these different subtypes. These slow changes are referred to as antigenic “drift” and are part of why creating a highly accurate flu vaccine is so difficult (2).
Typically, viruses that have drifted some are still susceptible to the current vaccine or there is some acquired immunity within the population. However, there is sometimes a more dramatic structural change referred to as antigenic “shift” that results in a completely new viral subtype and a population with virtually no immunity to this new agent (15). This can result in serious infection of pandemic proportions, such as the 2009 H1N1 outbreak (15).
Influenza viruses are typically spread through droplet transmission, when an infected person spreads microscopic drops of bodily fluids, typically through sneezing or coughing, which then encounter another susceptible person (8). These droplets usually only travel across air distances of 6 feet or less, however they can be transferred further via indirect contact such as handshaking or by vectors (surfaces or objects where virions survive temporarily while waiting on contact with the next host) (8).
Once a host touches a contaminated vector and then touches their own mucous membranes (nose, mouth, eyes, etc.), they can become infected. Other bodily fluids such as loose stools, vomit, and sputum can contain viral RNA and contribute to disease spread (8).

Self Quiz
Ask yourself...
- The typical point of replication for influenza is upper respiratory tract, more specifically the nares.
- How does this correlate with influenza symptoms?
- As you can see, influenzas are spread via many modes. How will you use this information to better protect yourself and patients from influenza infection?
Prevention: Flu Vaccines
Once pathogenicity is understood, providers are better able to prevent spread of infection. The primary and most effective way to help prevent the spread of flu is through a high rate of vaccination in the general population. Current recommendations are for all individuals 6 months of age and older to receive a vaccine unless otherwise contraindicated (8).
It is especially important that those most at risk (children under age 2, adults older than 65, and those with comorbid conditions) and those working with high-risk individuals (healthcare and childcare workers) receive vaccines.
For the optimum protection, the goal for vaccine timing should be by the end of October, keeping in mind that full antibody production takes about two weeks after the vaccine is received. Though early vaccination is ideal, a flu vaccine can be administered at any point during flu season and patients requesting immunization later in the season should still be vaccinated (8).
The first-time children between 6 months and 8 years of age receive a flu vaccine, they will need 2 doses, 4 weeks apart (8). After receiving 2 doses, children only need 1 dose for all subsequent flu seasons (8).
There are some individuals who should not receive a flu vaccine, but this group is typically small. Among those who are absolutely contraindicated are infants under 6 months of age and anyone with a previous life-threatening reaction to a flu vaccine (6).
It was previously thought that anyone with an egg allergy should not receive the vaccine, since the viral components are grown in an egg medium, however most recent recommendations suggest that this does not cause a reaction for most people and should be reviewed on an individual basis with one’s own primary care provider (6).
Anyone with a history of Guillain-Barré Syndrome should also consult their provider and may be advised to omit the vaccine. Patients with a current cough or cold accompanied by fever may be advised to postpone the vaccine until their symptoms have resolved (6).
Each year, the Centers for Disease Control and Prevention (CDC) study two factors of the current flu vaccine, efficacy and effectiveness. Randomized controlled trials are used to study efficacy, or the intended result, of the vaccine in optimal conditions with healthy participants (6). Less formal observational studies are used to study effectiveness, or how well the vaccine is working in the “real world.”
As previously discussed, antigenic drift and shift mean that the annual vaccine is imperfect and does not always prevent illness as well as intended. For a general idea of the typical effectiveness, we can look at data from recent years: the vaccine was shown to be 48%, 40%, and 38% effective in 2015-2016, 2016-2017, and 2017-2018 flu seasons respectively (6).
Regardless of the lower levels of effectiveness compared to other vaccines, such as MMR, vaccination against flu can still prevent substantial numbers of illness and death when considering the population of the United States.
There are a few side effects to be aware of and to include in patient education with administration of flu vaccines. The most reported side effect is local soreness around the injection site. This occurs in about 65% of patients vaccinated, does not typically interfere with activity, and resolves within a week (6).
More systemic symptoms such as fever, headache, and malaise are sometimes reported, but interestingly these symptoms are reported at similar rates in patients who received a placebo vaccine (6). Rarely, an allergic reaction can occur, ranging from urticaria to anaphylaxis.
Children under age 2 are at a slightly increased risk of febrile seizures, particularly if a flu vaccine is given in combination with Prevnar and DTaP vaccines, therefore timing of routine vaccines in conjunction with a seasonal flu vaccine should be discussed with parents of young children (6).
Though the actual correlation is unclear, there is also a suggested link between flu vaccines and the extremely rare condition of Guillain-Barre Syndrome (GBS). This often-life-threatening paralytic condition occurs in about 1-2 people per 100,000 each year, regardless of flu vaccine status.
Ongoing research indicates it is unlikely flu vaccines directly cause GBS and that other triggers such as recent viral illness are more likely to be the culprit, but the CDC estimates there may be a 2 per 1 million chance of experiencing this complication after receiving a flu vaccine (6).

Self Quiz
Ask yourself...
- How would you react if a patient refused the influenza vaccine due to potential side effects?
- What education would you provide?
Standard Precautions
In addition to vaccines as the front line of disease prevention, there are multiple ways to help slow or prevent the spread of disease once flu season starts.
Hand hygiene and cough etiquette are amongst the most effective measures to prevent spread of illness (1). These steps are easy and can be followed by anyone, regardless of if they are ill or not.
Avoid touching your mouth and nose. When coughing or sneezing, use a tissue to cover your nose and mouth and then dispose of the tissue and wash your hands. Handwashing should be done with soap and water or alcohol-based hand sanitizer (9). In addition to standard precautions, anyone with respiratory symptoms and/or fever is encouraged to wear a surgical mask.
Hospitals and clinics can help stop the spread of infection by separating well patients from those with respiratory symptoms (1). People who are ill should not attend work or school and should limit their contact with well people as much as possible while symptoms are present (9).
Infected individuals are considered contagious 1-2 days before showing symptoms and up to a week after illness begins; they should be fever free for 24 hours before returning to work/school (9).
Recognition and Treatment of Flu: Symptoms
Despite prevention efforts, hundreds of thousands of people nationwide will contract the influenza virus each season.
When prevention efforts fail, the next major step is early identification. It is important for all healthcare workers to be familiar with the symptoms of flu and be able to identify quickly and accurately those with a probable diagnosis of flu.
Typical influenza infections start suddenly with a combination of fever, headache, sore throat, fatigue, nasal congestion or runny nose, body aches, and chills.
Fever and acute symptoms can last more than 7 days, with fatigue and weakness lingering for weeks. While fever is typical of influenza infection, not all who are infected present with a fever (15).
Testing for Influenza
It should be noted that patients with suspected flu can be treated purely based on clinical presentation and regional flu trends at that time; rapid flu tests do not have the highest sensitivity and therefore should not be the determining factor in regard to the necessity of treatment. However, there are several methods of testing for flu that can help confirm a suspected diagnosis of flu.
There are two main types of testing for flu, molecular assays and antigen detection tests. Molecular assays work by identifying viral nucleic acids or RNA in a respiratory specimen (7). They are sensitive and specific, meaning they can detect the virus at extremely low levels and the risk of false positive is very low.
There are rapid molecular assays that can result in as little as 15 minutes, identifying flu A or B, and there are also Reverse Transcription-Polymerase Chain Reaction (RT-PCR) and nucleic acid amplification tests available which take closer to 45 minutes to an hour for results and can identify specific subtypes of flu for a more in-depth diagnosis (7). Antigen detection tests are typically used in outpatient settings due to their cost effectiveness and rapid results (10-15 minutes) These rapid tests are up to anywhere from 50-70% sensitive and have specificity >90% (7).
While more accessible to the clinic setting, antigen detection tests are less accurate, and a negative result does not exclude a diagnosis of flu. In cases where flu is highly suspected and a rapid test result is negative, the result can be confirmed with a molecular assay or treatment can be started based on clinical presentation and a presumed false negative test result (7).
In fact, where high risk populations are concerned, such as asthma, heart disease, immune disorders, and other comorbid conditions, prompt treatment when flu is suspected is recommended regardless of testing results (7).
Viral cultures are also available for the most in-depth results. While not practical for the clinical setting due to long result windows (3-10 days), viral cultures offer extremely detailed and useful information about the genetic details of current flu strains which is helpful when developing the next year’s vaccine (7).

Self Quiz
Ask yourself...
- Influenza testing is nuanced, and rapid testing cannot be relied upon for diagnosis.
- Does this mirror what you see or do in clinical practice?
- How could improved education of healthcare providers lead to more accurate diagnosing and treatment of influenza?
Treatment
Once flu has been identified clinically and laboratory confirmation is obtained (if desired), treatment of flu should be started as quickly as possible to maximize benefits of treatment and minimize potential complications of untreated illness.
Three antiviral medications known as neuraminidase inhibitors are available by prescription in the US (oseltamivir, zanimivir, and peramivir). These medications work by blocking neuraminidase, an enzyme that allows newly replicated influenza viruses to be released from host cells (5). Another antiviral, baloxavir, works by stopping replication of the virus within the host cells (5).
Treatment should ideally be started within 48 hours of symptom onset, however there may still be benefits for severely ill patients or those who are young, elderly, suffering from comorbid conditions, or already hospitalized, and treatment initiation after 48 hours may be considered (5). Treatment should also never be delayed while awaiting laboratory results (5).
Treatment may be initiated based on clinical symptoms alone if symptoms are highly suggestive of influenza during an endemic period. The decision to treat is based on many factors, including risk of complications and time since symptom onset.
The most common side effects of these medications include nausea, vomiting, headache, dizziness, and sometimes a skin reaction. Typically, these medications are well tolerated, and prompt initiation of treatment should be encouraged (5).
In addition to antivirals, supportive care is a mainstay of treatment. Rest, hydration, cool mist humidifiers, antipyretics, and throat lozenges have all been shown to provide comfort and help with symptoms. Multiple studies have shown honey to be an effective cough suppressant and 1 tbsp in warm tea or water can work well to provide some relief.
Patients should be monitored for signs of dehydration, including dry mucous membranes and reduced urine output. Ill patients should also isolate themselves as best as possible to prevent further spreading the illness (12).

Self Quiz
Ask yourself...
- Which patients are at highest risk of influenzas complications, including death?
- Is it justified to treat these individuals based on positive clinical symptoms even with a negative rapid test? Is it justified to treat them after 48 hours?
“Red Flags” – Potential Complications and What Not to Miss
Most flu cases make a full recovery after 1-2 weeks of illness, however there are some more serious complications that can develop, including life-threatening symptoms and even death (11). Flu can sometimes trigger systemic inflammation, leading to myocarditis, encephalitis, rhabdomyolysis, or multi-organ failure.
These conditions can be difficult to diagnose if suspicion is not high. Flu infections attack the usual defenses of the respiratory tract and predispose the body to secondary bacterial infections like pneumonia.
The body’s initial inflammatory response is beneficial to help the body fight off a flu infection but increasing inflammation or prolonged inflammation puts too much stress on the body and this extreme response can result in autoimmune disorders or sepsis (13). Those with asthma, heart disease, or other chronic conditions are at an increased risk of complications, as are young children and the elderly (11).
Post-influenza pneumonia is a well-described phenomenon, and the most common causative pathogen is Methicillin-resistant Staphylococcus Aureus (MRSA). This secondary infection should be considered in patients with respiratory symptoms and/or sepsis after a recent resolution of flu followed by returning or new/acute symptoms. It is important to consider MRSA as a causative agent when prescribing antibiotics to patients with post-influenza pneumonia (15).
“Red Flags” or warning signs that the body is working too hard to deal with the flu virus or is not compensating well include fast respiratory rate or difficulty breathing, cyanosis, tachycardia, hypotension, chest pain, dizziness, confusion, decreased urine output (>8 hours), severe muscle pain, or seizures. In children, fever >104 (or any fever in children <12 weeks of age) and retracting are concerning signs.
Any other signs/symptoms that are concerning or seem to be worsening warrant further workup and hospitalization to prevent further decline (11).

Self Quiz
Ask yourself...
- Have you ever seen a patient who displayed “red flags”?
- How would this change the patient’s management and what type of treatment / monitoring would they need?
Case Study 1
This case study involves a real patient’s experience with seasonal flu. Names, genders, ages, and some details have been changed to protect patient information.
Jennifer is a 35-year-old female who presents to an urgent care clinic in mid-February with 2 days of rhinorrhea, cough, sore throat, body aches, and tactile fever. She has not received a flu vaccine this season. Following triage, her vitals are recorded as: HR: 110, RR: 22, Temporal temperature: 101.3, SPO2: 97%, BP: 110/76.
She is visibly uncomfortable but sitting up on the exam table and able to cooperate and carry on a conversation. She is breathing a little shallowly and has a frequent, coarse sounding cough, but is overall not in any respiratory distress. She is congested and has clear rhinorrhea, eyes are watery, she has some posterior pharynx erythema, no cervical lymphadenopathy, and some faint rhonchi to her lungs that she can clear when coughing.
Rapid strep and rapid flu swabs are collected, and the results are negative. She is given a prescription for 5 days of 75mg BID TamifluⓇ (oseltamivir) which she fills and begins taking that afternoon. A viral culture is collected from her via nasopharyngeal swab for confirmation of suspected influenza.
Within 3-4 more days, Jennifer is fever free and beginning to feel better despite some persistent fatigue. She works from home until her fever has resolved and cough is improving. She makes a full recovery without sequelae. Three days later her viral culture indicates she has type B influenza, despite her negative rapid influenza test. This is a typical case of influenza, and the Tamiflu may have hastened her recovery and prevented severe illness. It also illustrates that rapid influenza testing has a low sensitivity and per CDC guidelines treatment may be based on clinical signs and symptoms.
Case Study 2
This case study involves a real patient’s experience with seasonal flu. Names, genders, ages, and some details have been changed to protect patient information.
Braxton is a 9-year-old male who presents to his PCP’s office with sudden onset of high fever (tmax 103), headache, and cough that started that morning. It is December and he has not received a flu vaccine. His vitals are stable.
Exam reveals clear rhinorrhea, erythematous and enlarged tonsils, and frequent barky cough. Rapid strep is negative and rapid flu is positive for Influenza A. He is given a prescription for Tamiflu (oseltamivir); however, his parents have some reservations about the medication due to an article they read on social media and decide not to give him the medicine.
They manage his symptoms with analgesics, Gatorade, and rest. About 11 days later he follows up in the office with complaints of persistent fatigue and new complaints of dizziness and abdominal pain. Parents report a syncopal episode at home that morning, prompting today’s visit.
His cough is still present, but better than it was, and he has been afebrile for about 5 days now. He looks very pale and complains of some dizziness as he gets up onto the exam table, his behavior is sluggish. He has some abdominal bloating and tenderness with mild spleen enlargement. He has lost 4 lbs. since his previous visit. Vitals are somewhat concerning: HR: 145, RR: 27, Temporal temperature: 98.8, SPO2: 98%, BP: 90/54.
He seems poorly hydrated, and his overall appearance is concerning so you order some stat labs. Multiple abnormal lab values return, the most critical of which is a hemoglobin of 3.4. He is admitted to the local children’s hospital PICU and treated for hemolytic anemia secondary to viral infection as well as multisystem organ failure.
After multiple blood transfusions and aggressive steroid therapy, he is discharged home after over two weeks of hospitalization with no permanent organ damage.
This case illustrates one of the rare (but potential) complications of the viral influenza infection. It is possible that early antiviral treatment may have avoided this complication and/or minimized it.
Summary
While influenza is an annual problem and can often seem routine, it is of utmost importance that healthcare professionals stay vigilant in their knowledge of flu and treat each case on an individual basis.
As the front lines for promotion of flu prevention, early identification, and treatment of flu, and maintaining alertness for potential complications, health care workers can have the biggest impact on the severity of the current flu season.
Staying up to date on current practice can help reduce overall numbers of infection, rate of complications, and mortality.
Nursing Documentation
Introduction
“I just love charting,” said no nurse, ever. If you ask most people why they want a career in healthcare, their response is that they wanted to help people. They did not want to spend hours in front of a computer clicking boxes. This time-consuming task of documenting in the medical record, or charting, is dull, repetitive, and sometimes disconcerting. It takes time away from being able to provide care for the patient. Yet documentation in the medical record is truly a vital part of patient care.
Nursing documentation fills a significant portion of the medical record. Nurses need make sure what they are adding is accurate and complies with the guidelines set by their facility and the state board. This principle is the same, even though there are differences to be aware of now that the electronic medical record has become the standard.
The Who, What, When, Where, Why, and How
Who:
There are approximately 2.9 million working RNs in the United States, with about 1.6 million working in hospitals (1). Nurses on a med-surg unit typically spend about one-third of their total working hours documenting (2). Considering a nurse on a med-surg floor spends about 2.5 hours per shift charting, that roughly translates into 7 billion hours spent charting each year. And that is only for the nurses!
Every discipline of the healthcare team contributes to the patient’s medical record. These different clinicians may not have the opportunity to report off to one another, and they must refer to the medical record to gather the information they need in order to care for the patient. Even kitchen staff responsible for preparing meals for patients must be able to see the dietary order for the patient. The following are a few examples of the clinicians who contribute to or review the patient’s medical record:
- Medical Team: physicians, nurse practitioners, physician assistants, surgeons, specialists, residents
- Nurses and LPNs
- Medical Assistants, CNAs, patient care assistants or technicians
- Specialty technicians: radiology, anesthesia
- Therapists: physical, speech, occupational, respiratory
- Pharmacists
- Dieticians
- Case managers or social workers
- Coding and billing specialists
- Researchers
What:
The primary purpose of the medical record is to communicate data about the patient and care provided between different members of the healthcare team. The bulk of the medical record is a collection of assessment data obtained from the patient. Details concerning assessments and results from lab tests or radiology comprise a large portion of the data. Assessment data is usually collected on a flow sheet system. Progress notes are written by the medical team or therapists help to guide the intended plan of care for the patient. This is considered narrative charting. The medical record also includes orders for prescribed medications and treatments from the medical team. The following are typical components found in a patient’s medical record.
- Patient demographics: name, age, gender, contact information, language, insurance information.
- Past medical history: surgeries, chronic conditions, family history, allergies, home prescriptions.
- History and Physical (H&P): this can contain information about admitting diagnosis or chief complaint and narrative of the story leading to admission.
- Flowsheet of assessment data: vital signs, head-to-toe assessment, intake and output record
- Laboratory test results.
- Diagnostic test results: from radiology or procedures.
- Clinical notes: progress notes from the medical team, procedure notes, notes from consulting clinicians, education provided, discharge planning.
- Treatment Orders.
- Medication Administration Record (MAR).
When:
The medical record should document every interaction the patient had with a member of the healthcare team. An encounter is created upon admission and everything occurring during a particular admission becomes part of the medical record. Phone calls made to patients and/or families may also become a part of the medical record.
Where:
Medical records are stored in various ways depending on their format and the facility. Paper records from small outpatient offices may be kept onsite. Records are now largely kept electronically. This is referred to as the electronic medical record (EMR) or electronic health record (EHR) and consists of Protected Health Information (PHI). They will be stored on a secure server, typically only accessible by authorized personnel.
Why:
The medical record is essential for several reasons. The primary reason for the medical record is that it allows members of the healthcare team the ability to review and analyze data in order to deliver appropriate care. It allows clinicians to keep track of all the care that has already been completed for the patient. It also provides the patient with a record of the treatment they received for as part of their lifetime medical history. The medical record is used for coding and creating a bill for the services the patient received. Medical records may also be used for process review and research. Ultimately, it is also a legal document and may be used in a court of law as applicable.
How:
Medical records are in the final stages of evolution from a paper chart to an electronic medical record system (EMR). By 2017, 96% of acute care hospitals and over 80% of physician offices possessed certified health IT (3). This migration of medical records from paper to electronic format was made possible with advances in technology in the last 30 years. The EMR allows members of the healthcare team to access the medical record instantaneously and improves continuity of care. Utilization of the EMR ultimately reduces costs in healthcare (4) and increases efficiency.
While EMR does have some drawbacks, the benefits that it provides are substantial enough that the government has encouraged its adaptation. The Health Information Technology for Economic and Clinical Health (HITECH) Act was enacted in 2009. This program provided tens of billions of dollars in financial incentives for healthcare facilities to adopt an EMR system (5,6).
Privacy and Security
Since 1996, HIPAA, The Healthcare Information Portability and Accountability Act, has been the governing legislation that provides for the privacy protection of medical records. Compliance with HIPAA mandates that anyone who interacts with patients receives training that will ensure that they will maintain privacy for the patient. Part of the HIPAA legislation also allows the patient to request their medical records.
The patient also has the right to request to amend their medical record. Patient permission must be given prior to a third party’s access to their medical record (7). HIPAA legislation was introduced at the advent of EMR technology. A provision of HIPAA provided a framework to ensure privacy of electronic health records (8). However, breaches in security by hackers or cyberterrorists remains a potential threat.
Benefits of EMR:
- Immediate data accessibility and communication of patient status.
- Clinicians can view records remotely, analyze the findings, and place orders immediately for faster patient treatment.
- Multiple clinicians can view the chart at one time.
- Records can be viewed from previous admission and/or outpatients visits easily.
- Records can be instantly shared between facilities (in instances of shared systems).
- Reduction in errors.
- Errors due to misinterpretation of handwriting are eliminated.
- Allows for increased safety checks. The EMR can be set to flag missing components of information, tasks that were not yet completed or are overdue, recognize duplicates, and present warnings if documentation has not yet been validated or “signed.”
- Scanning medications is possible with EMR systems to reduce the risk of medication administration errors.
- Assists with appropriate billing by capturing charges of services provided to the patient.
- The EMR can provide reminders for necessity of certain preventative health screenings or vaccines.
- Automatic “signature” of data is completed simply by the user logging in with a unique ID and password. All entries are date and time stamped. If a correction is made, the original data can be accessed.
- Accessing patient EMR is tracked and can be audited to protect patient privacy from unnecessary viewing.
Downsides of EMR:
- It is expensive to convert records system to an electronic system.
- The initial cost of the EMR software is very expensive.
- More workhours must be paid for staff training and coverage of patients during initial implementation of the program.
- Maintaining appropriate encryption and cybersecurity technology against viruses and hacking are also a costly component.
- Computer systems can be temporarily inaccessible, for example when updates and reboots are required. Paper charting is still necessary in the interim.
- Template charting has limitations (9)
- Templates may not exist for a specific problem and does not accurately reflect the patient’s condition. Atypical patients may have multiple problems or extensive interventions that must be documented in detail.
- Templates may also encourage cloned or copied documentation. It creates unnecessary redundancy and at times inaccurate information in the EHR. Some EHR systems are designed to facilitate cloning with such popular features as:
- “Make me the author” to assume the content of another person’s entry,
- “Demo recall” of “Duplicate Results” to copy forward vital signs or assessment data.
- “Smart phrases” pulls in specific identical data elements.
- Automated insertion of previous or outdated information through EHR tools, when not modified to be patient-specific and pertinent to the visit, may raise significant quality of care and compliance concerns.

Self Quiz
Ask yourself...
- Think about your current charting system.
- How does your medical record system facilitate accurate charting?
- Do you believe that your system is efficient?
- What are some issues with your system that make it difficult to accurately and timely chart nursing care?
The Legal Requirements
If it wasn’t documented, it wasn’t done. Every healthcare practitioner has had this mantra ingrained in them from the very beginning of their career. Nurses are trained to document defensively, that is, if they are taught at all.
In a 2014 study, only 20% of new graduate nurses had received electronic medical record training as a part of their nursing school curriculum (6). It is not uncommon for clinicians to have the tendency to view the medical record as a defense tool against potential legal problems, rather than its more significant role as a communication tool for patient care.
Regardless, accurate and complete documentation is an essential. Your career, and more importantly, patient care, depends on it.

Self Quiz
Ask yourself...
- Did you receive proper training on documentation in your nursing program?
- How can programs be improved to better prepare nurses?
When Documentation Becomes Your Defense
In the dreaded event of a legal problem, medical record will be scrutinized to every detail. It is usually the primary source of evidence for the case. A malpractice lawsuit requires four elements to be proven (10):
- That a medical professional assumed a duty to provide care for the patient.
- The clinician failed to provide appropriate care within their scope of practice for the patient.
- The failure in appropriate care caused an injury to the patient.
- The injury resulted in damage to the patient.
Potential legal problems that may arise include the following (11):
- Administrative liability – Professional licensure discipline, discharge (firing) from position.
- Civil Liability – Malpractice lawsuit, failure to provide necessary care.
- Criminal liability – Misdemeanor or felony charges for cases of gross negligence.
The Cost
Fortunately, medical malpractice claims have begun to drop since 2001. In 2004, the medical practitioners involved, the defendants, won the case 83% of the time. The legal fees can still amount to $18,000 if the case is dropped, to as much as $93,000 even when the case is won (12,13).
In 2018, there were 8,718 malpractice cases that resulted in payments to injured patients (14). Of those events, 310 reports of malpractice suits that resulted in payments related to nursing care.
However, 180 of those, about 60% of those had payments to the injured patient that were over $50,000 (14). However, there were nearly 15,000 adverse action reports filed against nurses, which was more than the number combined filed against physicians, NPs, and PAs combined.
The majority of medical malpractice cases primarily target the physician and the facility. However, anyone who made an entry into the patient’s medical record may be required to participate in legal proceedings.
Most common malpractice claims against nurses include failure to (15):
- Follow standard of care.
– Follow safety protocols.
– Perform procedures according to guidelines. - Use equipment properly.
– Use or operate equipment within the manufacture’s details. - Failure to correctly document.
– Communication with the provider.
– The care you completed. - Follow assess and monitor.
– Report a change in status of the physician.
– Assess a patient with change in status. - Communicate pertinent data.
– Provide appropriate discharge education and information.
– Communicate properly and completely between shifts.

Self Quiz
Ask yourself...
- Think about the last difficult shift you had. Did you properly document?
- How would you prioritize documentation differently after reading this module?
What is Required for Nursing Documentation?
Necessary medical record documentation can vary significantly depending on the care area. For example, the documentation a circulating nurse in the operating room completes will be very different from what is documented on an emergency room patient. While the basic principles of documentation stay constant, the nurse needs to be familiar with the documentation requirements for that area based on requirements of the state board of nursing, the facility, and the unit.
There are standard requirements for medical record documentation that are applicable in all patient care settings, and in both paper and EMR systems. These standards include the following (16):
- Accurate: Clinicians must be careful to proofread documentation to make sure it is free from errors. A small typo can have serious repercussions, as it is more likely to be misinterpreted by others.
- Relevant, concise, organized, and complete: It is important to keep the information concise and relevant so that other care providers can quickly find the pertinent information that they need. Assessment data should be entered in a systematic way. Complete documentation ensures all of the unit policies for documentation are addressed.
- Free of bias: Clinicians should only include information that is pertinent to the care of the patient and remain free from personal bias. Direction quotations should be utilized with proper context.
- Factual: Clinicians should not exaggerate or minimize findings. Charting is to be completed after completing a task, not before. Do not speculate data. Observations need to include exact times and measurements. Avoid approximations. Make sure to chart on the correct patient.
- Timely: What occurred during the shift should be documented during the shift. Documentation should be done as soon as possible after task completing. If something needs to be added in after the shift was completed, it should be denoted as a late entry with a reason as to why. Your facility likely has strict requirements regarding late entries.
- Legible/decipherable and clearly written: Paper documentation must be clearly legible. Writing must clearly convey meaning.
- Standardized: Clinicians must use appropriate medical terminology and approved acronyms and abbreviations.
- Labeled and Auditable: Paper documentation must be signed with credentials and must include date and time of the entry. When charting in the EMR, all entries and corrections are recorded, and time stamped. Password sharing or having another clinician assist in documenting under incorrect username is fraudulent.

Self Quiz
Ask yourself...
- Do you currently incorporate all of the above principles in your documentation?
- If not, how can you change your practice to improve your documentation?
Examples of Good and Bad Charting
The following will show some examples of these principles in action. These are based on the scenario of a patient admitted in the Emergency Department for chest pain.
| Example of Good Documentation | Example of Poor Documentation | |
| Accuracy | Patient stated she took 800mg of Tylenol at 4pm, an hour after she began to feel chest pain. | Patient reports she took pain med for chest pain. |
| Relevant | Patient stated she has never experienced chest pain prior to this event and does not have a history of cardiac problems. | Patient was a competitive athlete 20 years ago and used to be in great shape. Patient thinks she is still pretty healthy. |
| Concise | Vital signs taken, telemetry monitor applied, lab samples collected, and PIV started per the chest pain protocol. | Patient was triaged and immediately brought to exam room. In accordance with the chest pain protocol, vital signs were taken first. Then the patient had a telemetry monitor applied. Next, the patient had blood samples drawn through the inserted PIV catheter. |
| Organized | Pt reports no allergies. Prescriptions include hormone replacement therapy. Past medical history includes hysterectomy and foot surgery from a few years ago. Patient family history includes cardiovascular disease on her father’s side of the family. Pt denies smoking, illicit drug use, but does drink 3 times a week. Pt reports feeling fine until 1 hour after lunch when chest pain began. | Patient was feeling fine until one hour after lunch, when she started to feel chest pain. Patient has no history of cardiac problems. However, there is family history of cardiovascular disease on the father’s side. Patient had a hysterectomy and foot surgery a few years ago. Patient denies smoking and illicit drug use. Patient does take hormone replacement therapy prescription. Patient does not have any allergies. Patient reports drinking alcohol x3/week. |
| Complete | Patient complaining of 8/10 chest pain, described as “stabbing.” Pain has been experiencing this pain for three hours. She has taken Tylenol, but nothing is able to alleviate the pain. | Pt is complaining of chest pain. |
| Free of Bias | Education provided per chest pain protocol. Patient was instructed to call 911 immediately if experiencing chest pain in the future. Patient verbalized understanding. | Patient was given needed education about chest pain since she clearly didn’t understand that chest pain cannot wait 3 hours and she need to call 911 right away because she can die of a heart attack. |
| Factual | Patient reports last meal was around 1300 which consisted of spicy foods. Her chest pain onset was 30 minutes after. She waited an additional three hours before seeking emergency care. | Patient presented to ER after lunch. |
| Legible/Decipherable | Patient was instructed to call for assistance with ambulation and how to utilize call light. | Patient cannot safely walk by she self. Call light assistance. Bathroom walk with me. |
| Standardized | Morphine Sulphate 2mg IV push, once PRN for 8/10 pain per chest pain protocol. | MSO4 2.0 mg, IV push, x1. |
| Timely | Documentation is completed in real-time, all documentation completed before transferring patient to telemetry. | Nurse documents three days later due to high volume of patients. |
Common Documentation Errors
- Falsification of a record. This can happen from charting an action was never done, or from charting information before the action was completed.
- Fraudulent charting is the act of knowingly making a false record. Criminal charges of forgery can result if the misrepresentation was done for personal gain. An example of this would be a nurse documenting administration of controlled substance but was instead diverting the medication.
- Inappropriate use of cloning features. Information “copied and pasted” from a different patient’s record or that was completed by another provider. Data copied from previous shift assessments that isn’t updated to reflect current status is also a false record (9).
- Fail to document communication. Notification of the medical team of a change in patient status or critical lab values should always been included. Clarification or confirmation of orders should also be documented (17). Include notification of other providers who assisted with patient are. This includes failure to document transfer of care to another nurse.
- Failing to document a reason why something wasn’t done. If a patient doesn’t receive a prescribed medication, the reason why the medication wasn’t given needs to be described. If you communicate with the provider, this should also be included.

Self Quiz
Ask yourself...
- Have you ever failed to document or failed to document a critical portion of care?
- If you could alter your documentation, how would you better document in this situation?
Conclusion
Including all of the necessary information into each patient’s medical record is a daunting task. The nurse must make sure that they have included all of the relevant and accurate information that is required by their facility guidelines. It must usually be done in a loud environment and is frequently interrupted by actually having to provide care to the patients.
It is not only a tedious chore, but it also tends to cause a lot of apprehension. There is usually a worry of “did I chart enough?” or “did I chart everything I needed to?” This is due to the defensive practices and attitudes healthcare workers have adapted to protect against malpractice lawsuits. In this way, charting is a lot like paying taxes. No one likes it, but it still has to be done.
Perhaps a way to develop a healthy perspective toward charting is to change the focus back to its original purpose: to communicate care about the patient. The purpose of charting is to relay to the other healthcare team members what is going on with the patient. With this objective in mind, the nurse will inevitably cover all the necessary details. It may also be a bit more satisfying to know that even though they are in front of the computer, they are still doing something important for the patient.
End of Life Process
Introduction
Have you ever cared for someone who was dying, known someone who was on hospice, or just wondered what happens as we die? Hospice involves caring for the terminally ill as they begin the end-of-life process and is utilized by healthcare facilities around the country. Hospice care can be a short or long journey, with many ups and downs. For some, the prognosis might be obvious, but for others, it might be filled with many questions and much uncertainty. Both caregivers and patients seek to understand just what the end-of-life process and its care entails. Hospice clinicians should spend time providing education on end-of-life process to those involved in caring for the patient.
Oftentimes, caregivers have little to no experience in caring for a patient experiencing the end-of-life process and can easily find themselves feeling overwhelmed, confused, and burned out. Understanding what to expect during the final weeks of life is imperative in order to cope with the changes as they occur. The end-of-life process can vary from person to person. Although patients progress through the end-of-life process differently, there is usually a recognizable pattern of decline that occurs. In order to provide the best possible care and prepare both the hospice patient and their family members, it is important for the nurse and caregiver to be able to distinguish the phases of the end-of-life process: transitioning, actively dying, and final moments.
Transitioning
This phase of the end-of-life process, otherwise identified as the pre-active phase, usually signals that a person is approaching the last two-to-three weeks of their life. During this time, caregivers might start to notice obvious changes, an increase in sleeping, for example. A transitioning person can sleep upwards of twenty hours per day. This significant increase is part of an overarching decrease in the patient engaging with the world and day-to-day life.
Beyond sleeping, examples of this disengagement include interacting less with friends and family, less desire to do one’s usual activities, and a lack of interest in things that were once pleasurable. Additional signs of a patient transitioning include increased weakness and decreased mobility. These changes typically include a decline in function, becoming non-ambulatory, chairbound, and ultimately, bedbound. Progressively, the patient will become more dependent on their caregivers to assist them with activities of daily living (ADL), which include bathing, eating, transferring, toileting, and continence.
Another indicator that someone may be transitioning is a change in nutrition and intake. Eating and drinking less is an expected part of decline during this time. Many patients will report a lack of appetite, taste changes, and an overall lack of interest in food and liquids. Changes in swallowing may further complicate a person’s ability to eat and drink.
It is not uncommon to downgrade a person’s diet during the transition phase. This might include going from a regular diet, down to soft, and finally, to pureed. Liquids are usually given in small amounts and with an added thickener. These changes are necessary to prevent choking and aspiration.
Increased agitation, anxiety, and restlessness may also arise during the transitioning phase of the end-of-life process. Terminal agitation and terminal restlessness are both unique to the last week or so of someone’s life and are often caused by physiological changes that occur during the end-of-life process but can also be a result of medication or emotional changes. Despite if the patient had lived peacefully and calm in the past, it is important to note that these symptoms may still occur.
Signs of terminal agitation include an inability to remain still, picking at items in the surrounding environment, and increased confusion. Fortunately, there are medications that can be given at the end of life to promote comfort and stop these symptoms when they arise. Lastly, it is not uncommon for the transitioning patient to have visions of and talk to deceased friends and family – both are normal and could sometimes be interpreted as a welcoming sign from loved ones.

Self Quiz
Ask yourself...
- What would you say to someone you knew was dying?
- What do you know about hospice care?
Active Dying
Following the transition phase, most patients will then enter the final phase of the end-of-life process, the active dying period. This phase usually last only two to three days and showcase significant signs of patient decline that differ from the previous phase, including a decrease in alertness and responsiveness. For example, a patient may go from a semi-comatose state to comatose or obtunded and minimal reaction should be expected. Their eyes may be open or shut, and there is little movement in all extremities. This period can be described as a deep sleep.
Caregivers often describe it as a time of waiting. Cognitive changes, in combination with the previous changes in swallowing, make the intake of food, liquids, and medications unsafe. The patient is at high risk for aspiration. Mouth swabs can be used to hydrate the oral cavity and to do mouth care. Medications that are liquid or can dissolve under the tongue are safe and can be used to manage symptoms at the end of life. Hospice patients are provided a comfort kit of medications to use should symptoms arise.
Additionally, changes in vitals are expected during this phase, and they typically do not cause the patient any discomfort. For example, temperature fluctuation is common at the end of life. It is not abnormal to have an elevated temperature during the active phase of the end-of-life process. This can be remedied with cooling measures such as a cool towel on the forehead or a fan to cool down the room. The skin may feel clammy as well.
Following, changes in blood pressure and heart rate may also occur. Blood pressure begins to trend lower during the pre-active phase and can become very low during the last few days of life. The heart rate will usually trend upward and can be well over 100 beats per minute, however, this is just something for the hospice nurse to note and is not usually treated.
Pain can also be an area of concern for someone who is actively dying, and of course, no one wants to see their loved one in pain during their final days of life. The body becomes very sensitive to the slightest movement or touch, which can present challenges for caregivers when considering that the patient still needs to be cleaned, changed, and repositioned. When the patient is no longer verbalizing their comfort, verbal pain cues must be assessed. These include grimacing, a furrowed brow, frowning, and possibly moaning. In some cases, repositioning can be an effective pain-relieving measure.
Decreased urination is also common during the active phase of the end-of-life process. This is completely normal and expected. Caregivers may find that they do not need to change diapers as often. Urine may also appear darker in color, appearing a deep amber color due to more concentrated urine.
Excessive secretions can lead to something commonly known as the “death rattle.” This term is almost synonymous with the last days of life. It can be described as a moist sound that is audible when someone breathes and is a good indicator that death is near. The secretions collect in the throat due to a lack of coughing and the inability to clear them out. Turning the patient on his or her side may help the secretions drain, and there are medications that can be administered to help dry them out. It is important to note that not everyone will experience this, and by the time it occurs, there is a disconnect within the patient, and he or she is not likely to experience any discomfort.

Self Quiz
Ask yourself...
- What is a caregiver likely to feel while experiencing these changes?
- What does comfort mean to you?
Final Moments
It can be hard to imagine the final moments of someone’s life. This is especially true for caregivers and families who have witnessed steady decline throughout both phases of the end-of-life process. It is the role of the hospice clinician to provide education regarding what to expect during this time. There are likely to be signs that death is possible at any moment. A patient can be expected to be comatose with little to no response when death is imminent.
In addition to changes in vitals described previously, changes in respirations usually occur. Patterns can vary from shallow and fast to deep and slow. Periods of apnea are also normal. Cheyne-stokes breathing may also be present. Skin changes are also expected; pallor, cyanosis, and mottling are signs that death is near. The body may begin to feel cool, especially in the hands and feet. Comfort medications can still safely be used up until death occurs. As mentioned before, foods and liquids should not be given at this point. Caregivers should continue to talk to the patient, as their hearing will remain until the end.

Self Quiz
Ask yourself...
- Have you been present when someone died? How did it make you feel to witness this?
Conclusion
Hopefully, this has been an informative piece on what to expect for end-of-life care. Hospice can be a great resource for both the patient and caregiver. Most people do not have experience in caring for a dying person and need education and assistance throughout the journey. Not everyone who is dying will experience all the symptoms mentioned in this course, and it is important to note that everyone experiences the end-of-life process in their own way and own pace.
Alzheimer’s Nursing Care
Introduction
Alzheimer’s disease is a destructive, progressive, and irreversible brain disorder that slowly destroys memory and thinking. Alzheimer’s is the most common cause of dementia in older adults (1). For most people who have Alzheimer’s disease, symptoms first appear in their mid 60’s (1). Studies suggest more than 5.5 million Americans, most 65 or older, may have dementia caused by Alzheimer’s (1). It is currently listed as the sixth leading cause of death in the United States. It is important to understand the signs and symptoms of Alzheimer’s dementia and how to manage the care of a patient, family member, or friend suffering from the disease.
Dementia is the loss of cognitive functioning-thinking, remembering, and reasoning- and behavioral abilities to such extent that it interferes with activities of daily living (1). The severity of dementia ranges from mild to severe. In its mildest stage, it begins with forgetfulness, with its most severe stage consists of complete dependence on others for general activities of daily living (1).
History of Alzheimer’s
Alzheimer’s disease is named after Dr. Alois Alzheimer. In the early 1900’s, Dr. Alzheimer noticed changes in the brain tissue of a patient who had died of an unknown mental illness. The patient’s symptoms included memory loss, language problems, and unpredictable behavior. After her death, her brain was examined, and was noted to have abnormal clumps known as amyloid plaques and tangled bundled fibers, known as neurofibrillary or tau tangles (1). These plaques and tangles within the brain are considered some of the main features of Alzheimer’s disease. Another feature includes connections of neurons in the brain. Neurons are responsible for the transmissions of messages between different parts of the brain and from the brain to other parts of the body (1).
Scientists are continuing to study the complex brain changes involved with the disease of Alzheimer’s. It seems that the changes in the brain could begin ten years or more before cognitive problems start to surface. During this stage of the disease, the people affected seem to be symptom-free; however, toxin changes occur within the brain (1). Initial damage in the brain occurs within the hippocampus and entorhinal cortex, which are the parts of the brain that are necessary in memory formation. As the disease progresses, additional aspects of the brain become affected, and overall brain tissue shrinks significantly (1).
Signs and Symptoms & Diagnosis of Alzheimer’s Disease
Memory problems are typically among the first signs of cognitive impairment related to Alzheimer’s disease. Some people with memory problems have a condition called Mild Cognitive Impairment (MCI) (4). In this condition, people have more memory problems than usual for their age; however, their symptoms do not interfere with their daily lives. Older people with MCI are at increased risk of developing Alzheimer’s disease. The first symptoms of Alzheimer’s may vary from person to person. Many people display a decline in non-memory related aspects of cognition such as word-finding, visual issues, impaired judgment, or reasoning (4).
Providers use several methods and tools to determine the diagnosis of Alzheimer’s Dementia. To diagnose, they may conduct tests of memory, problem-solving, attention, counting, and language. They may perform brain scans, including CVT. MRI or PET to rule out other causes for symptoms. Various tests may be repeated to give doctors information about how memory and cognitive functions change over time. They can help diagnose other causes of memory problems such as stroke, tumor, Parkinson’s disease, and vascular dementia. Alzheimer’s disease can be diagnosed only after death by linking clinical measures with an examination of brain tissue in an autopsy (4).

Self Quiz
Ask yourself...
- Have you experienced a patient in your practice with dementia or Alzheimer’s disease? What did their symptoms look like?
- What are some common diagnostic tools that healthcare providers use in the diagnosis of this disease?
- What is the definitive diagnosis of Alzheimer’s disease?
Stages of Disease
Mild Alzheimer’s
As the disease progresses, people experience significant memory loss along with other cognitive problems. Most people are diagnosed in this stage (1).
- Wandering/getting lost
- Trouble handling money or paying bills
- Repeating questions
- Taking longer to complete basic daily tasks
- Personality/behavioral changes (1)
Moderate Alzheimer’s
In this stage, damage occurs in the area of the brain that controls language, reasoning, sensor processing, and conscious thought (1).
- Memory and confusion worsen
- Problems recognizing family and friends
- Unable to learn new things
- Trouble with multi-step tasks such as getting dressed
- Trouble coping with situations
- Hallucinations/delusions/paranoia (1)
Severe Alzheimer’s
- Plaques and tangles spread throughout the brain and brain tissue shrinks by a significant amount
- Cannot communicate
- Completely dependent on others for care
- Bedridden – most often as the body shuts down

Self Quiz
Ask yourself...
- What are some of the signs and symptoms that differentiate each stage of Alzheimer’s disease?
- A person is in what stage of Alzheimer’s disease when they struggle recognizing family members and friends?
Prevention
As a person ages, many worry about developing Alzheimer’s disease and dementia. Especially if they have had a family member who suffered from the disease, they may worry about genetic risk. Although there have been many studies on the prevention of the disease, and many are still ongoing, nothing has been proven to prevent or delay dementia caused by Alzheimer’s disease (2).
A review led by experts from the National Academies of Sciences, Engineering, and Medicine, found encouraging yet inconclusive evidence for three types of interventions related to ways to prevent or delay Alzheimer’s Dementia or age-related cognitive decline (2):
- Increased physical activity
- Blood pressure control
- Cognitive training
Treatment of the Disease
Alzheimer’s disease is complex and is continuously being studied. Current treatment approaches focus on helping people maintain their mental function, manage behavioral symptoms, and low the symptoms of the disease. The FDA has approved several prescription drugs to treat those diagnosed with Alzheimer’s (3). Treating symptoms of Alzheimer’s can provide patients diagnosed with comfort, dignity, and independence for a greater amount of time, simultaneously assisting their caregivers. The approved medications are most beneficial in the early or middle stages of the disease (3).
Cholinesterase inhibitors are prescribed for mild to moderate Alzheimer’s disease; they may help to reduce symptoms. Medications include Rzadyne®, Exelon ®, and Aricept ® (3). Scientists do not fully understand how cholinesterase inhibitors work to treat the disease; however, research indicates that they prevent acetylcholine breakdown. Acetylcholine is a brain chemical believed to help memory and thinking (3).
For those suffering from moderate to severe Alzheimer’s disease, a medication known as Namenda®, which is an N-methyl D-asparate (NMDA) antagonist, is prescribed. This drug helps to decrease symptoms, allowing some people to maintain certain essential daily functions slightly longer than they would without medication (3). For example, this medication could help a person in the later stage of the disease maintain their ability to use the bathroom independently for several more months, benefiting the patient and the caregiver (3). This drug works by regulating glutamate, which is an important chemical in the brain. When it is produced in large amounts, glutamate may lead to brain cell death. Because NMDA antagonists work differently from cholinesterase inhibitors, these rugs can be prescribed in combination (3).

Self Quiz
Ask yourself...
- Is there a cure for this disease?
- What are some of the treatment forms that have been used for the management of Alzheimer’s disease?
- Can medications be used in conjunction with one another for the treatment of the disease?
Medications to be Used with Caution in those Diagnosed with Alzheimer’s
Some medications such as sleep aids, anxiety medications, anticonvulsants, and antipsychotics should only be taken by a patient diagnosed with Alzheimer’s after the prescriber has explained the risk and side-effects of the medications (3).
Sleep Aids
They are used to help people get to sleep and stay asleep. People with Alzheimer’s should not take these drugs regularly because they could make the person more confused and at a higher risk for falls.
Anti-Anxiety
These are used to treat agitation and can cause sleepiness, dizziness, falls, and confusion (3).
Antipsychotics
They are used to treat paranoia, hallucinations, agitation, and aggression. Side effects can include the risk of death in older people with dementia. They would only be given when the provider agrees the symptoms are severe enough to justify the risk (3).
Caregiving
Coping with Agitation and Aggression
People with Alzheimer’s disease may become agitated or aggressive as the disease progresses. Agitation causes restlessness and causes someone to be unable to settle down. It may also cause pacing, sleeplessness, or aggression (5). As a caregiver, it is important to remember that agitation and aggression are usually happening for reasons such as pain, depression, stress, lack of sleep, constipation, soiled underwear, a sudden change in routine, loneliness, and the interaction of medications (5). Look for the signs of aggression and agitation. It is helpful to be able to prevent the problems before they happen.
Ways to cope with agitation and aggression (5):
- Reassure the person. Speak calmly. Listen to concerns and frustrations.
- Allow the person to keep as much control as possible.
- Build in quiet times along with activities.
- Keep a routine.
- Try gently touching, soothing music, reading, or walks.
- Reduce noise and clutter.
- Distract with snacks, objects, or activities.
Common Medical Problems
In addition to the symptoms of Alzheimer’s disease, a person with Alzheimer’s may have other medical problems over time. These problems can cause confusion and behavior changes. The person may be unable to communicate with you as to what is wrong. As a caregiver, it is important to watch for various signs of illness and know when to seek medical attention for the person being cared for.
Fever: Fever could be a sign of potential infection, dehydration, heatstroke, or constipation (4).
Flu and Pneumonia: These are easily transmissible. Patients 65 years or older should get the flu and Pneumonia shot each year. Flu and Pneumonia may cause fever, chills, aches, vomiting, coughing, or trouble breathing (4).
Falls: As the disease progresses, the person may have trouble with balance and ambulation. They may also have changes in depth perception. To reduce the chance of falls, clean up clutter, remove throw rugs use armchairs, and use good lighting inside (4).
Dehydration: It is important to remember to ensure the person gets enough fluid. Signs of dehydration include dry mouth, dizziness, hallucinations, and rapid heart rate (4).
Wandering
Many people with Alzheimer’s disease wander away from their homes or caregiver. As the caregiver, it is important to know how to limit wandering and prevent the person from becoming lost (5).
Steps to follow before a person wanders (5)
- Make sure the person carries a form of ID or wears a medical bracelet.
- Consider enrolling the person in the Medic Alert® + Alzheimer’s Association Safe Return Program®
- Alert neighbors and local police that the person tends to wander and ask them to alert you immediately if they are seen alone.
- Place labels on garments to aid in identification.
Tips to Prevent Wandering (5)
- Keep doors locked. Consider a key or deadbolt.
- Use loosely fitting doorknob covers or safety devices.
- Place STOP, DO NOT ENTER< or CLOSED signs on doors.
- Divert the attention of the person away from using the door.
- Install a door chime that will alert when the door is opened.
- Keep shoes, keys, suitcases, coats, and hats out of sight.
- Do not leave a person who has a history of wandering unattended.
Conclusion
Alzheimer’s is a sad, debilitating, progressive disease that robs patients of their life and dignity. As research continues on the causes, treatment, and prevention of the disease, it is important for healthcare workers and caregivers to know the signs and symptoms of a patient with Alzheimer’s disease and potential coping mechanisms and management strategies of the disease. More information on the disease is available through several various resources, including:
Family Caregiver Alliance
800-445-8106
NIA Alzheimer’s and related Dementias Education and Referral Center
800-438-4380
PTSD in Nurses
Introduction
Nursing can be high stress, demanding, and unpredictable. In some cases, nurses are exposed to potential physical, psychological, and mental hazards for upwards of 12-16 hours a day. Each person reacts and responds to extreme stress and trauma in various ways, and because there are so many variables to consider, it has been challenging to diagnose PTSD in nursing.
It is natural for individuals to experience fear, heightened senses, and avoidance after experiencing a traumatic event. Nurses are aware of our body’s natural defense to danger or fear, commonly identified as the “fight or flight” response. There are many scenarios that define a traumatic event, and not everyone identifies them the same. For example, some may say losing a loved one is traumatic for them, whereas others may define life-threatening situations or witnessing one as being traumatic for them – all of which are valid.
The question now stands, “when do these traumatic events turn into PTSD?”
In order to fully answer this, we must first define PTSD.
Definition
Post-traumatic stress disorder is defined as a psychiatric disorder that can occur in people who have experienced or witnessed a traumatic event (1).
The DSM-5 diagnostic criteria for PTSD include:
- Stressor (one required):
– Personally experiencing trauma or watching someone endure it.
– Learning that a traumatic event(s) may have occurred to a close family member or friend.
– In cases of life-threatening instances, or the death of a family member/friend, the event(s) must have been violent or accidental.
– Experiencing repeated excessive exposure to adverse effects of a traumatic event (e.g. nurses working in critical care units, caring for COVID-19 patients, etc.) (2).
- Intrusion symptom (one or more required):
– Recurrent and distressing memories or dreams of the trauma experienced.
– A dissociative reaction in which the person is completely unaware of their surroundings.
– Intense, prolonged psychological exposure to internal or external cues that may resemble the traumatic event.
– Distinct physiological reactions of internal or external reminders that may represent any aspect of the traumatic event (2).
- Avoidance (one or both required):
– Avoiding any memories, thoughts, or feelings related to the traumatic event on a continuous basis.
– Avoidance or efforts to avoid instances or items that resemble or remind the person of the traumatic event. Examples include (2):
– People
– Places
– Activities
– Conversations
– Familial objects
- Negative alteration in cognition and mood (two required):
– Inability to remember specifics of the traumatic event due to dissociative symptoms.
– Persistent and over-exaggerated negative belief about oneself, others, or the world (e.g. “the world is completely dangerous” or “my whole nervous system is shot”).
– Persistent negative emotional state (e.g. fear, anger, guilt, or shame).
– Persistent distorted perception about the cause of the traumatic event leads an individual to blame his or herself.
– Distinctive or diminished interest or participation in any significant activities. Feelings of detachment from others. Continuous inability to experience positive emotions (2).
- Alterations in arousal and reactivity (two or more):
– Angry outbursts and irritable behavior without provocation, leading to physical aggression toward people or objects.
– Self-destructive reckless behavior.
– Hypervigilance.
– Exaggerated startle response.
– Problems with concentrating.
– Sleep disturbance (2).
- Duration of the disturbance (Criteria B, C, D, and E required):
– More than a month.
- Functional Significance (required):
– Clinically significant distress caused by the traumatic event(s) or impairment in social, occupational, or other areas of functioning.
– The functional disturbance is not attributable to the psychological effects of a substance or any other medical condition (2).
Case Study
Laura is a 26-year-old nurse of five years who has decided to take a traveling nursing job to help with the overwhelming demand to care for COVID-19 patients. She is given a wonderful opportunity to make a difference. The staffing agency offered Laura a critical care staff nurse position, where she is expected to care for two patients and work 36 hours weekly on night shifts for 13 weeks. Her pay would be $5,000 per week plus a non-taxed stipend for lodging and meals.
She accepts the job and immediately takes leave from her full-time position in Tennessee. She packs her belongings, says goodbye to her family, and begins her venture to California.
Upon her arrival to the hospital, Laura reports to the critical care department to meet with the nurse manager. Following, she is told by her superior that her contracted assignment has changed and that she will now be taking care of at least seven COVID-19 patients due to short-staffing. Laura is confused and feels as though she cannot say no due to her being under contract, so she attempts to reach out to her agency; no one is available to take her call. She leaves a message in hopes that someone will get back to her as soon as possible, however, she is expected to start her first shift that same evening.
Following, Laura’s first night is horrific; she is caring for seven COVID-19 patients that are all on ventilators, and she has no resources available to her if she has any questions. The environment is overwhelming; patients are lined against the wall, people are crying, a code red is being called every 10-to-15 minute, and most of the time, the patient dies. The morgue is overflowing, and some of the deceased patients are placed in body bags and lined against the wall or piled into a single room.
After only three shifts, Laura decides she cannot fulfill this contract because she has no support, is experiencing nightmares, feels extremely agitated, anxious, and seems to be crying all the time. As a result, she reaches out to her agency and informs them of her decision to end the contract.
The agency tells her that she will be reported to both the Tennessee (her home state) and California Board of Nursing for job abandonment, meaning she cannot practice if she breaks her contract.
Upon receiving this ultimatum, Laura decides to stay to fulfill the contract.
Over the next few weeks, Laura notices that some of her co-workers are manifesting a change in behavior. They have become increasingly sad, detached from others, displaying anger toward other staff members, and anxious. Laura feels as though her work environment is toxic, and she wishes she were anywhere else in the world but there, however, she cannot leave.
This is a prime example of PTSD in nurses.

Self Quiz
Ask yourself...
- Have you experienced perceived trauma that can be categorized as PTSD in nurses?
- Can a person experience PTSD without having a clinical diagnosis?
- Think of Laura’s current work environment:
- When you are having a stressful day, what do you think she is feeling or thinking?
- How are her co-workers relating to her actions?
Sign and Symptoms of PTSD in Nurses
There are many signs and symptoms of PTSD in nurses. Symptoms may develop immediately, or within three months of the traumatic event(s). On some occasions, a person can suppress their feelings for up to a year before remembering a traumatic event. Many of the signs and symptoms are grouped into four categories: intrusive memories, avoidance, negative changes in mood and thinking, and negative changes in physical and emotional reactions (3).
Intrusive memories include:
- Recurrent distressing memories of the traumatic event
- Flashbacks
- Nightmares
- Severe emotional distress
- A physical reaction to something that reminds the person of the traumatic event.
Avoidance: includes any memories, thoughts, or feelings related to the traumatic event on a continuous basis. For examples, see “The DSM-5 diagnostic criteria for PTSD include” section above.
Negative changes in mood and thinking includes:
- Feelings of hopelessness about the future
- Not remembering certain aspects of the traumatic event
- Difficulty in maintaining close relationships
- Feeling of detachment
- Lack of interest in activities once enjoyed
- Difficulty experiencing positive emotions
- Feeling emotionally “numb”
- Alcohol or drug abuse
- Having negative thoughts about yourself, other people, or the world (3)
Changes in physical and emotional reactions include:
- Heightened senses, fight or flight
- Insomnia, trouble concentrating
- Overwhelming feelings of guilt or shame
- Increased irritability, aggressive behavior, outbursts with no provocation
- Chronic illnesses, gastrointestinal problems, sweating/shaking
- Angina
- Self-destructive behavior, depression, hallucinations, anxiety, and feelings of constant sorrow (3)

Self Quiz
Ask yourself...
- Take a mental moment. Do you feel like you are experiencing any of these symptoms or have experienced them in the past?
- As a nurse can you identify any of these symptoms in your co-workers?
- Does Laura or her co-workers display any of these symptoms?
- As nurses, we are trained to perform assessments on our patients not ourselves. Because you experience any of these symptoms could it mean you have PTSD?
- How many times have you brushed off any of these symptoms as just isolated events?
Types of PTSD
Since we know that the American Psychiatric Association describes PTSD as a psychological disorder, we know there are different types and severity levels of PTSD. As previously mentioned, everyone can experience the various types, however, we are going to focus on the commonly diagnosed types of PTSD in nurses.
Overall, there are five types of PTSD, which include: normal stress response, acute stress disorder, uncomplicated PTSD, complex PTSD, and comorbid PTSD (4).
Normal Stress Response
The normal stress response, the “fight or flight,” is the precursor to PTSD in nurses, and it does not always lead to full-blown PTSD. Any event that causes our natural stress response, such as surgery, an injury or pending thoughts of danger, all initiate a normal stress response; the problem occurs when this response is not alleviated within a short amount of time.
Acute Stress Disorder
A life-threatening event such as job loss, illness, natural disaster, or death of a loved one can initiate this early form of PTSD in nurses. While the individual may experience this type of disorder, they will typically overcome the initial stressor. If it becomes prolonged and untreated, it can lead to full-blown PTSD.
Uncomplicated PTSD
This type of PTSD in nurses is associated with one major event, making it the easiest form of PTSD to treat. The individual will want to avoid everything that could remind them of the event.
Complex PTSD
Complex PTSD is just as the name implies. This type of PTSD in nurses is associated with multiple traumatic events and is usually associated with various types of abuse, violence, war, and traumatic losses. The unfortunate problem with diagnosing this type of PTSD is that some professionals confuse it with a borderline or antisocial personality disorder or dissociative disorders (4).
Comorbid PTSD
This type of PTSD in nurses is associated with a person with more than one mental health concern and substance or narcotic abuse issues at the same time. This condition is extremely common because most people have more than one problem. PTSD makes this more complicated to treat because individuals try to self-medicate because they are in denial, but this only leads to self-loathing and self-destructive behaviors (5)

Self Quiz
Ask yourself...
- Take a moment and review the types of PTSD. Can you identify with any one of the types listed?
- Which type is Laura experiencing if any? What type is her co-workers experiencing?
- How difficult would it be to recognize the difference between the five types of PTSD within yourself or your co-worker?
Phases of PTSD in Nurses
There are four phases of PTSD identified by Pyramid Health. The phases are impact (emergency), rescue, intermediate recovery, and long -term reconstruction (5).
Impact Phase (Emergency)
The impact phase consists of the initial reaction such as anxiety, helplessness, guilt, shock, or fear. This occurs immediately after the individual experiences the traumatic event. The duration of this phase depends on the severity of the event (5).
Rescue Phase
The rescue phase involves the individual being able to come to terms with what has happened. This is closely related to the acceptance phase in grieving. The individual may experience flashbacks, confusion, anxiety, denial, or feelings of despair.
Intermediate Recovery Phase
The intermediate recovery phase is associated with the individual making the adjustment to return to everyday life. In this phase, the individual can begin to look at other issues within their life. While addressing new issues, they may have the feeling of altruism, in which they feel the love and support from others, causing them to believe that they can also help others.
Additionally, they may also develop the feeling of disillusionment, in which they feel overwhelmed because they are not receiving love and support that they think they should, or when the level support ends, they realize they are on their own.
This phase is closely related to the acceptance phase in grieving. As with the grieving phase, the individual may go back and forth between phases.
Long-Term Reconstruction Phase
The long-term reconstruction phase is characterized by the individual being able to rebuild while continuing to deal with the trauma’s aftermath. Their main concern is about their future and how they can maintain healing.
Causes of PTSD
Defining the causes of PTSD in nurses can be quite tricky because physicians have not been able to determine why some individuals may have a different response to the same traumatic event. Many nurses have experienced stressful experiences that did not cause PTSD. Some causes or increased risk for developing PTSD in nurses could include inherited mental health risk, an individual’s temperament, and how our brain regulates chemicals and hormones that release stress in our bodies.
The hippocampus is a component of the brain that works to consolidate information from short- to long-term memory, links these memories to sensations, and enables our ability to navigate through spatial memory (6). The hippocampus is located under the cerebral cortex in the allocortex, and there are two hippocampi, one on each side of the brain that have very distinct roles.
PTSD is associated with abnormal hippocampal activity (6). It has been noted that PTSD is mainly associated with functional and structural changes in the amygdala, medial prefrontal cortex, and the hippocampus (6). The main role of the posterior hippocampus is in memory retrieval and spatial cognition, whereas the role of the anterior hippocampus is mainly associated with the amygdala, hypothalamic-pituitary-adrenal (HPA) axis, and limbic prefrontal circuitry (6).
The anterior hippocampal-amygdala connections are thought to underlie atypical memory processes in PTSD, including flashbacks, intrusive thoughts, and nightmares (6). There are current theories of PTSD that identify hippocampal dysfunction as a key contributor to hallmark symptoms of PTSD in nurses (7).
One common denominator for causes of PTSD is the actual stress an individual goes through when they experience or learn about a life-threatening event, serious injury, sexual assault, childhood physical abuse, being threatened with a weapon, an accident, being exposed repetitively to death, violence, or sickness.
The Effect on Nurses
The COVID-19 outbreak has been a severe impact on the healthcare industry. Professionals are working tirelessly to care for patients who are experiencing health issues caused by COVID-19, leading to a significant spike in PTSD in nurses.
Professionals in critical care, trauma, and emergency room departments are continuously witnessing death on top of working within a crowded, high-stress environment that often faces short-staffing.
Factors relating to development of PTSD in nurses:
- Age
- Work experience
- Previous psychiatric history
- Marital status
- Family support
- Coping styles

Self Quiz
Ask yourself...
- From the information in the case study, what do you think the causes are for Laura’s symptoms?
- Who do you think would be more susceptible to PTSD, the senior nurse, or the junior nurse?
Prevalence of PTSD in Nurses
Based on the current U.S. population (223.4 million), around 7 to 10 of every 100 people will have experienced some traumatic event in their lifetime. 20% of the population (44.7 million) suffer from PTSD. The chances of experiencing traumatic events and receiving a PTSD diagnosis within the nursing profession are very high (8).
In most instances, nurses are trained to put their patients’ needs over their own when they walk in the door. When their shift starts, they attempt to suppress their emotions so they can get through their shift. A nurse may experience a rush of feelings such as anger, guilt, confusion, sadness, sorrow, and grief and sometimes, in extreme cases, suicidal or homicidal ideations. To mask their emotions, they may turn to drinking, drugs, or destructive behaviors to cope with the day-to-day trauma from their job.
A 2009 nursing study covering depression and anxiety revealed a high prevalence of burnout syndrome and PTSD in nurses. The 810-person study revealed that 22% of participants experience symptoms of PTSD, and 18% met the diagnostic criteria for PTSD. Additionally, the results determined that while 86% met the criteria for burnout syndrome, 98% fulfilled the diagnostic criteria for PTSD and were positive for burnout syndrome. The study concluded that nurses with burnout syndrome and PTSD were significantly more likely to have difficulty in their outside life from work (13).
An additional study that evaluates the results of over 24 publications regarding PTSD in nurses between 1999 and 2019 determined that a majority of nurses with PTSD had the following:
- Leadership roles
- Negative outlook on patient care
- Lack of supportive relationships, staffing, and organizational support
- Internalized both short- and long-term patient suffering
As they continue to push through global pandemics, natural disasters, and continuous tragic events, PTSD in nurses is a prevalent issue that we must address.

Self Quiz
Ask yourself...
- Would Laura’ symptoms or actions lead you to think she was experiencing PTSD?
- What about her co-workers, would their actions lead you to think they were experiencing PTSD?
- Based on the statistics in the section above, does that make a difference on your assessment of Laura’s symptoms?
Current Therapy
PTSD will continue to worsen without treatment. The Veterans Health Administration and Department of Defense (VA/DoD) and the American Psychological Association (APA) in 2017 each established treatment guidelines for PTSD (10). Both guidelines recommend the use of prolong exposure (PE), cognitive processing therapy (CPT), and trauma-focused cognitive behavioral therapy (CBT). Another trauma-focused therapy is eye movement desensitization and reprocessing (EMDR) therapy (10).
Non-trauma-focused treatments include medication, relaxation therapy, and stress inoculation training (SIT).
Trauma-Focused Therapies
Prolong Exposure (PE)
Prolong exposure (PE) therapy is strongly recommended by both the APA and VA/DoD as a successful treatment of PTSD. PE is based on the emotional processing theory, which stipulates traumatic events are not emotionally processed at the time of the event.
PE therapy consists of two main components: in vivo and imaginal exposure (10).
Cognitive Processing Therapy (CPT)
CPT utilizes the social cognition theory and the informed emotional processing theory. Following a traumatic event, usually, a survivor attempts to make sense of what has happened and leads to distorted cognitions regarding themselves, the world, and others. The main goal of CPT is to shift an individual’s unhelpful beliefs related to their trauma toward more accommodating, positive and helpful beliefs to promote new learning (10). Sessions usually take 12 weeks, and they incorporate psychoeducation about the cognitive model and exploration of the patient’s conceptualization of the traumatic event (10).
Cognitive Behavioral Therapy (CBT)
Trauma-focused CBT is based on behavioral and cognitive models drawn from cognitive behavior theories, including PE and CPT. This type of therapy includes modifying negative appraisals, correcting the autobiographical memory, and removing the problematic behavior and cognitive strategies.
It is believed that guilt-associated appraisals tend to evoke negative effects and are usually paired with images or thoughts of the trauma, thus causing a repeated and reconditioned memory of the trauma; Ultimately producing distress, leading to tendencies to suppress or avoid the trauma-related stimuli in individuals (10).
The techniques associated with CBT include exposure and cognitive restructuring. The exposure technique for a traumatic memory utilizes imaginal exposure, writing about the trauma, and reading the traumatic memory out loud (10). The most important aspect of cognitive restructuring is teaching the patients to identify the various dysfunctional thoughts and erroneous thinking, replace them with rational alternative thoughts, and having them reconsider their beliefs about themselves, the trauma, and the world (10).
Eye Movement Desensitization and Reprocessing (EMDR) Therapy
EMDR therapy requires healthcare professionals to help a patient move their eyes back and forth while imagining or recalling their traumatic event. This technique allows the individual to reprocess the memory while addressing the past, present, and future aspects of the traumatic memory.
Medication Therapy
The current medication therapy recommended by the APA for PTSD treatment is sertraline (Zoloft), paroxetine (Paxil), fluoxetine (Prozac), and venlafaxine (Effexor). Although all medications must be customized for each individual, it is important to note that Zoloft and Paxil are the only FDA-approved medications for the treatment of PTSD (11).
In some cases, taking antidepressants in conjunction with PTSD medication treatments can serve as beneficial. Those medications include:
- Clonidine and Guanfacine, Risperidone for agitation
- Clonidine, Prazosin and Trazodone for trauma-related nightmares
- Beta-blockers such as Propanol are used to decrease hyperarousal symptoms but it has not been approved by the FDA (12).
Non-Trauma Focused Therapies
Relaxation Therapy
Relaxation therapy is a form of psychotherapy that utilizes breathing techniques, progressive muscle techniques, and meditation to illicit a voluntary relaxation response of the individual. Sometimes, guided imagery is utilized to have the individual focus on positive images in their mind. This technique helps lower the individual’s blood pressure, relieves tension in their muscles, and lowers their stress.
Progressive Muscle Relaxation has been utilized to help reduce fatigue and relieve PTSD in nurses. This technique involves sequential tensing of major muscles in the body. This form of relaxation therapy reduces feelings of tension, lowers perceived stress, and can be performed anywhere at any time. This technique has the positive effect of decreasing the pulse rates, increases the individual’s oxygen saturation and is sometimes used in conjunction with other forms of psychotherapy (13).
Stress Inoculation Training (SIT)
SIT is a form of psychotherapy used for the treatment of PTSD. This training is a type of cognitive-behavioral therapy that teaches the individual coping skills and helps them find new ways to deal with their PTSD symptoms. SIT teaches individuals to react differently in stressful situations and is performed in phases (14).
In the first phase, the individuals learn about their PTSD symptoms, and they identify the traumatic stress that they experienced. Following, the individual learns how to monitor their stress level. In the second phase, they learn new problem-solving strategies and coping skills that help them relax their bodies, control their breathing, interrupt the upsetting thoughts, and help the individual stay in the current moment. Research shows that SIT is one of the most effective forms of therapy for PTSD (14).

Self Quiz
Ask yourself...
- Which therapy option would you choose for Laura and her co-workers and why?
Coping Mechanisms
It is sometimes difficult for individuals experiencing PTSD to cope with the mountain of symptoms that they may encounter. For nurses experiencing PTSD, it is critical that they seek treatment and develop coping mechanisms. If their symptoms go untreated, their work performance and quality of patient care may decrease.
Nurses have resources available to help them cope with PTSD. Some workplaces have elicited the help of psychiatrists or psychologists to provide drop-in services at the worksite. Various positive coping mechanisms include:
- Spiritual guidance in prayer
- Having a strong support system to lean on such as a sponsor that the individual can all when feeling overwhelmed
- Including their family in the healing process
- Performing mindful meditation or yoga
- Performing guided imagery to focus on positive thoughts when the stressors resurface
- Prescription medication
- Peer support at work
- Professional counseling
- Group therapy

Self Quiz
Ask yourself...
- Think of your work environment. Do you know what resources are available to you if you experience PTSD?
- How can you help your colleagues cope with the day-to-day pressures of working in a high-stress environment?
- Looking back at the case study. Perform a complete assessment of Laura and her work situation and develop a plan of care for her and her co-workers.
Conclusion
PTSD can be a very debilitating condition and affects millions of people every year. Nurses are on the front lines serving the public during a health crisis, and we now know that for them to do their jobs effectively, their mental health must be a priority.
Many organizations now offer counseling, time off, peer support, and incentives for nurses to take care of themselves. With proper treatment, we can alleviate or control PTSD in nurses. Our goal for the future is to continue to make the physical, spiritual, and mental health of all health care workers a top priority so that they can continue to provide the best care to patients.
Ethics in Nursing
Introduction
Ethics is an important aspect of all professions, but in this case, we are going to touch on its role in nursing. From the beginning, Florence Nightingale was a strong advocate and initiated nursing ethics and morals. For the 19th consecutive year, nursing has been ranked number one by the Gallup Poll as the most honest and ethical profession (1). The designation creates a larger responsibility to understand the American Nurses Association (ANA) Code of Ethics and how to apply to practice. Daily, nurses face ethical challenges and are confronted with situations with competing values and interests (2). How do we identify the issues? How do we respond to them? To understand our responsibilities as nurses, one must be aware of the details and applications of the ANA Code of Ethics with Interpretive Statements that give voice to nursing’s social mandate (3).
History
Did nursing exist before Nightingale? Yes, but not in an organized fashion, as the formalization of an ethical model began in the mid-1800s with Nightingale. Prior to her development of a formal training program, nursing was thought to be disreputable, and many persons providing caregiving services were prostitutes. Nightingale was the first to instill morals and ethics into education and practice. In 1889, the Trained Nurse and Hospital Review journal was published, including a six-part series on ethics (3).
Following, in 1893, the Nightingale Pledge was written by Listra Gretter to be used at the Farrand Training School for Nurses in Detroit, Michigan (4). The Pledge is as follows:
“I solemnly pledge myself before God and in the presence of this assembly, to pass my life in purity and to practice my profession faithfully. I will abstain from whatever is deleterious and mischievous and will not take or knowingly administer any harmful drug. I will do all in my power to maintain and elevate the standard of my profession and will hold in confidence all personal matters committed to my keeping and all family affairs coming to my knowledge in the practice of my calling. With loyalty will I endeavor to aid the physician in his work and devote myself to the welfare of those committed to my care.” (4)
The Pledge was written 128 years ago; the changes and challenges in nursing over these years are immeasurable.
Professional Ethics
Each profession has its own board with specific rules of ethical standards and principles; these standards and principles include honesty, respect, adherence to the law, avoidance of harm, integrity, and accountability. The specifics may differ per profession, but the basics are the same.
Nursing Ethics, Principles and Values
Although nothing had yet been formalized, the idea of ethics in nursing began to spread during the early 1900s. The ANA developed the first Code of Ethics in 1950, and did not revise it until 2015. The principles of ethics rely on several terms, defined as follows:
Autonomy
This can be as simple as listening to a patients’ individual rights for self-determination, including informed consent and patient choices. How this is viewed depends on the situation (5). It is important to note, in cases of endangering or harming others, for example, through communicable diseases or acts of violence, people lose this basic right (5).
Beneficence
This term refers to doing good and is part of the Nightingale Pledge and the Hippocratic Oath. Showing acts of kindness and facilitating wellbeing are great examples. However, it is important to understand that we as nurses, may think that we know what is best for our patient, but it is never a guarantee if they will agree with us; this is referred to as paternalism (5).
Justice
This is including the principle that covers normative aspects that are often discussed in terms of solidarity and reciprocity. Fair distribution of resources and care is an important aspect of this principle (5).
Non-Maleficence
This term almost directly translates to ‘do no harm,’ and can be part of confidentiality or other acts of care that can involve possible negligence. Additionally, it is used in end-of-life situations and decisions of care with terminally or critically ill patients (5).
Fidelity
This is the basic principle of keeping your word, and can be included in providing safe, quality care (5). If you tell a patient that you will be back to check on their pain level, and you in fact, do check back, that is fidelity – you have kept your promise.
Veracity
This term requires that you be truthful, accurate, and loyal to not only your patients and their families, but your co-workers as well. Are we telling our patients the truth? Are we holding back information about their conditions? Things to think about include pain medication and dosages (5). Placebos are an example of veracity.
Accountability
This is your responsibility of judgment and actions. To whom are you accountable? Examples include yourself, your family, colleagues, employer, patient, and the nursing board. One must take responsibility for their own actions (5). The following are components of accountability:
- Obligation: a duty that usually comes with consequences.
- Willingness: accepted by choice or without reluctance.
- Intent: the purpose that accompanies the plan.
- Ownership: having power or control over something.
- Commitment: a feeling of being emotionally compelled (5)
When examining nursing ethics, one must consider that the profession has three entry levels: diploma, Associate’s, and Baccalaureate degrees. This can affect what each nurse learns about, including values and ethics as well their real-life application.

Self Quiz
Ask yourself...
- When did ethics begin to develop in nursing?
- How do you define ethics?
- What are the six principles of ethics?
- How do you view patient autonomy?
- Do you think the different entry levels for nursing make a difference in ethics?
Foundations of Nursing Ethics
Nightingale was the first to teach ethics in nursing and set strict codes for those under her supervision; today, the ANA Code of Ethics serves as a concise statement of ethical obligations and duties of every person that enters into the profession.
The first three provisions of the ANA Code of Ethics describe the most fundamental values and commitments a nurse must make. The following three include boundaries of duty and loyalty, and the last three demonstrate aspects of duties beyond individual patient encounters.
Values are an important provision that remind us as individuals that we all have morals. As young children, we begin developing these values as we developmentally progress and learn from our families. What happens when your personal values are different from the values of the profession? This can also be a part of spiritual, ethnic, and cultural differences (5).
The Worldview is inclusive of ethical and moral discussions, as well as dilemmas for nurses around the world and primarily focuses on four elements: people, practice, profession, and co-workers (6). The International Council of Nurses (ICN) is more directed toward the Worldview. Not all are included in the ANA Code of Ethics.
An interesting factor to note is that the ICN Worldview focuses on co-worker relationships: “Nurse bullying occurs in almost all care settings and units, from the patient floor to the executive suite. In fact, 60% of nurse managers, directors, and executives in one 2018 study4 said they experienced bullying in the workplace, and 26% considered the bullying “severe” (7). Workplace intimidation is any intimidating or disruptive behavior that interferes with effective healthcare communication and threatens patient safety; it is often categorized as horizontal or relational aggression. Improving how management addressed such issues in nursing may be critical not only for staff turnover, but for patient outcomes.
There is some reluctance to specify the sorts of behavior that will not be tolerated, but effective anti-bullying practices must include a statement of exactly what constitutes bullying. From an ethical perspective, the acceptance of nurses who “eat their young” should no longer be tolerated.

Self Quiz
Ask yourself...
- What is the background of the ANA Code of Ethics?
- Have you read the ANA Code of Ethics?
- Evaluate and review horizontal aggression in the workplace. Have you experienced it?
- How does your personal culture and background affect your practice?
- What workplace behaviors should not be tolerated?
Application
As patient advocates, nurses work as part of an interdisciplinary team to provide patient care. Nursing ethics have kept pace with the advancement of the profession to include a patient-centered focus rather than a physician-centered focus. Due to its main focus of providing care, nursing ethics are often different than medical ethics; and it is important for us to understand the differences.
As we discuss application, one must take into consideration the workforce of nurses today. In many facilities, nursing staff may encompass at least three and maybe even four generations. This also applies to our patients. Those generations are identified as follows:
- Traditionalists or Silent Generations (1922- 1946):
- Respect authority, are hardworking, and are sacrificial for their work.
- Many have delayed retirement (8).
- Baby Boomers (1946- 1964):
- Possess a belief that workers must pay their dues, are a workaholic, and typically rely on traditional learning styles (8).
- Generation X (1965-1977):
- Independent, a skeptic of authority, and self-reliant (8).
- Generation Y (1978-1991):
- Team-oriented, tech-savvy, entrepreneurial, and has a desire to receive feedback (8).
- Generation Z (1992- 2010):
- Tech savvy, understand the power of text and social media. (8)
No matter what generation you fall into, it is important to understand the different personality and learning styles of everyone.
A prime example of the generational learning styles differing and potential issues that may arise is the usage of electronic health/medical records (EMR) and various other health information technologies that are often incorporated into daily nursing practice. Nurses that come from older generations may struggle with these more, as they have experienced its transition and had to adapt.
Following, as the prevalence of social networking platforms continue to rise, it is important for nurses to understand the ethics of social media. Issues of privacy confidentiality and anonymity are ethical concerns when mixing personal and professional information on a social media platform; it is also important to note that most healthcare facilities have strict policies regarding social media.
End-of-Life
End-of-life issues are filled with nursing ethics and dilemmas. If the advanced directive is not clear, family issues and other complications trigger many of the ethical principles. Self – determination (the right to stop or refuse treatment) is complicated, the patient may not always have their wishes on paper, and often, families often do not want to let go. Nurses are the backbone of allowing the patient’s wishes to be known. It is important that nurses know that they can request an ethics committee review for their patients if they feel their wishes are being violated.
Additionally, physician-assisted suicide can be extraordinarily complex issue. For both the Hippocratic Oath and the Nightingale Pledge, there are ethical issues. Currently, the following states have made physician-assisted suicide legal: California, Colorado, Hawaii, Maine, New Jersey, Oregon, Montana, The District of Columbia, and Washington (9). With the ever-expanding ability to both prolong and end life, nurses must be cognizant and prepared for all repercussions associated with life and death situations (10).
With recent societal and technological advancements in science and medicine, choices involving both life and death are seeming to become more complicated. As a result of this worldwide controversy in healthcare, many nurses nation-wide are now forced to deal with this ethical dilemma head on (10). There are and will be many debates as to the ethical issues involved in physician -assisted suicide and something on the forefront for nursing to consider.

Self Quiz
Ask yourself...
- Evaluate your work environment and the differences in generations.
- Think about what ethical dilemmas you face daily.
- Has technology increased the ethical dilemmas in your practice?
- Do you know how to access your facilities ethic committee?
- What are your thoughts on physician-assisted euthanasia?
The ANA Code of Ethics
The ANA Code of Ethics serves to guide nurses in maintaining ethical standards and in ethical decision-making. Additionally, it outlines the obligations nurses must have for their patients and the nursing profession. The provisions focus on the following as stated by Lockwood (11):
1. Respect for Human Dignity
The nurse must show respect for the individual and consider multiple factors (belief systems, gender/sexual identification, values, right to self-determination, and support systems) when planning and providing care. The nurse ensures patients are fully informed and prepared to make decisions about their healthcare and to carry out advance healthcare planning.
2. Commitment to Patients
The nurse must always remember that the primary responsibility is to the patient and help resolve conflicts between the patient and others and avoid conflicts of interest or breach of professional boundaries.
3. Protection of Patients’ Rights
The nurse must be aware of legal and moral responsibilities related to the patients’ rights to privacy and confidentiality (as outlined by HIPAA regulations) and research participation.
4. Accountability
The nurse bears primary responsibility for the care of the patient and must practice according to the Code of Ethics and the state nurse practice act and any regulations or standards of care that apply to nursing and healthcare.
5. Professional Growth
The nurse must strive always to promote health, safety and wellbeing of self and others. The nurse must, in all circumstances, maintain personal integrity and report violations of moral standards. The nurse has a right to refuse to participate in actions or decisions that are morally objectionable but cannot do so if this refusal is based on personal biases against others rather than legitimate moral concerns.
6. Improvement of Healthcare Environment
The nurse must recognize that some virtues are expected of nurses, including those associated with wisdom, honesty, and caring for others, and that the nurse has ethical obligations toward others. The nurse is also responsible for creating and sustaining a moral working environment.
7. Advancement of the Profession
The nurse must contribute to the profession through practicing within accepted standards, engaging in scholarly activities, and carrying out or applying research while ensuring the rights of the patients are protected.
8. Health Promotion Efforts
The nurse recognizes that health is a universal right for all individuals and collaborates with others to improve general health and reduce disparities. The nurse remains sensitive to cultural diversity and acts against human rights violations, such as genocide, and other situations that may endanger human rights and access to care.
9. Participation in Goals of the Profession
The nurse must promote and share the values of the profession and take action to ensure that social justice is central to the profession of nursing and healthcare.
Conclusion
In conclusion, nurses face ethical dilemmas in practice almost every day, which is why it is so valuable for nurses to understand the philosophy of nursing ethics and its application in practice.
Ensuring Patient Confidentiality in Nursing
Introduction
In order to provide the best care possible to patients, there must be a foundation of trust that the patient-provider relationship is built on. If the foundation is not stable, the rest of the relationship is at risk for crumbling. One way that trust is built is by maintaining patient confidentiality or privacy.
When it comes to the medical field, the wrong medicines or treatments may be administered or performed. This could result in further complications. Medical conditions, treatments, and results can often be sensitive topics things patients do not necessarily want shared with society for a variety of reasons. Patients rely on their providers to keep the information they communicate in confidence, and only sharing it under certain circumstances.
With the ever-growing platform of social media and advancements in technology, there is a grey area that exists when it comes to patient confidentiality and what can and cannot be shared. The purpose of this course is to educate on the aspects of patient confidentiality and its importance.

Self Quiz
Ask yourself...
- What do you already know about patient confidentiality?
The Privacy Rule
The Health Information Portability and Accountability Act of 1996 (HIPAA) became the groundwork for the Standards for Privacy of Individually Identifiable Health Information (Privacy Rule) issued by the U.S. Department of Health and Human Services (HHS). It was designed to meet the requirements set by HIPAA regarding how healthcare providers used and disclosed a patient’s private health information. It also addressed patients having the right to know and dictate how their health information is utilized. Overall, the Privacy Rule’s goal was to set clear boundaries when it came to properly protecting health care information while allowing the exchange of pertinent information to protect the health and well-being of the public (2).
Many groups are included under HIPAA’s term of “covered entities.” These entities have connections to personal health care information on a variety of levels. Groups such as healthcare providers, health plans, healthcare clearinghouses, and business associates are all covered entities. The protected information they encounter is anything that can or is believed to identify an individual: name, date of birth, address, and Social Security Number. Any past, present, or futured mental or physical health, condition, or payment and health care provisions for an individual are also classified as protected information (4).

Self Quiz
Ask yourself...
Think of where you work.
- What type of facility do you work in?
- What does your work consider patient identifiers?
- Is there anything you think should be added to that list when it comes to what can identify a patient?
De-Identifying Patients
There are many steps involved in de-identifying a patient for those who use or share patient information, as it applies to HIPAA. De-identifying a patient is the act of removing as many identifiers as one can in order to eliminate the chances of an individual being recognized through the scenario or situation (3).
There are two methods to de-identifying:
Formal evaluation by a qualified expert.
A qualified expert must be a person with significant knowledge and experience with knowing scientific and statistical standards or methods to ensure patient information is not identifiable. They do this by determining if the risk of using the information is very small. They often document what methods they use to make the determination (3).
The act of removing individual identifiers.
Many of these identifiers are things one would expect to be removed when identifying a patient, such as a name, age, date of birth, home address, Social Security Number, full-face photos, and phone numbers. However, some of them include any form of vehicle identifier—serial or license plate numbers—internet protocol (IP) addresses, biometric identifiers like finger or voiceprints, serial numbers or device identifiers, and web universal resource locators (URLs). An entire list of the 18 identifiers is located on the Department of Health and Human Services website (3).
Neither of these methods are 100% perfect in their goal, but they decrease a patient’s chance of being identified significantly. Once the patient has been de-identified, the information is no longer restricted by the Privacy Rule since all patient identifiers have been removed. This means that the information can be used without worry of violation (3).

Self Quiz
Ask yourself...
- Which version of de-identifying a patient do you think is better?
- Have you ever had to de-identify a patient or patients?
- What was it for?
- Did you expect some of the listed identifiers to be on the list?
Professional Statements
Over the years, professional medical organizations have released statements regarding patient confidentiality and how it pertains to their target audience. Many medical organizations such as the American Nurses Association (ANA) and the American Medical Associations (AMA) often create position statements to reflect the organization’s overall stance and thoughts on a specific topic. These positions may be used to guide education, policies, or individual opinions on the topic.
The ANA released a statement regarding patient privacy and confidentiality. As mentioned before, the ANA believes that the patient-provider relationship is important, and confidentiality is essential in that relationship. The organization supports legislation, standards, and policies that protect patient information. In the professional statement document, the ANA goes on to give recommendations regarding the protection of patient information. These recommendations support the patient’s right to have protected information and to select who is the recipient of medical information. They encourage that patients be given information regarding HIPAA and the Genetic Information Nondiscrimination Act—an act passed in 2008 to prohibit individuals’ discrimination based on genetic information (5). They acknowledge that the patient has the right to access their information and use it to make healthcare decisions. They note that patients should be notified when and how their information may be used. There is a heavy emphasis on not using patient information if consent has not been given unless there is an extenuating circumstance regarding legal requirements. This will be discussed in the next section (1).
Since patient confidentiality is extremely important, the ANA supports healthcare organizations in creating safeguards to protect patient confidentiality. They also support the that the organizations enforce ways to alleviate violations done by health care workers and protect them from retaliation (1).

Self Quiz
Ask yourself...
- Have you read the ANA’s statement on patient confidentiality before?
- Are you in any professional organizations?
- Do these organizations have any statements about patient confidentiality?
- Are there any differences between them and the ANA’s statement?
Disclosure
Overall, patient information is discouraged from being shared; however, there are several instances where the sharing of information is allowed. The patient may give the provider(s) or healthcare organization permission to share the information with whoever the patient decides. By providing consent, the patient is essentially waving the right to keep that information confidential but determines who can receive the information. This can be done through written or verbal consent, though most facilities require a written one. This written form is placed in the patient’s medical records (6).
If another healthcare agency or provider is going to be involved with the patient’s care, medical information can be exchanged on a “need to know” basis. For example, if a patient is being transferred to another facility, the accepting nurse and care team would need a thorough report to ensure that they knew the patient and what had already been done for them regarding medical care (6).
While protecting patient information is important, there are a few circumstances—called extenuating circumstances—that allow healthcare providers to share information regarding a patient without permission outside of the above reasons. Certain information is required to be reported to public health departments or authoritative organizations: communicable diseases, suspected child or elder abuse, gunshot wounds, release to insurance companies for payment, or worker’s compensation boards after a claim has been submitted are allowed (6).
In the case of protecting the public, healthcare providers can report patient information to a specific organization if it comes down to the health of the public. As mentioned above, testing positive for communicable diseases can be reported to public health departments.
It should be noted that one important exception applies to this rule. Making assumptions, especially about if a spouse has the right to know the medical history of a patient just because they are married, is not advised. Patients should be encouraged to inform their spouse about the information that may put the spouse at risk, such as sexually transmitted infections. If the individual’s direct safety is threatened, then the provider can tell them (6).
In order to protect society, healthcare providers have the duty to warn if they have detailed and documented proof that the patient is targeting a select individual or group. Providers are encouraged to document instances of threats, whether it be against them, another provider, or another individual outside of the healthcare setting. Often this is a legal or ethical duty to report the threat to the authorities or possibly warn the potential victim (6).
If a provider is concerned about what can or cannot be disclosed at any time, it is encouraged that the provider consults hospital policies before releasing any information (6).

Self Quiz
Ask yourself...
- What policies does your facility have when it comes to disclosing information?
- How do you obtain consent for sharing information?
- Have you ever shared information outside of the “need to know” basis with other providers when it comes to a patient?
- Have you ever had to report a patient to another organization such as Child Protective Services or the county Department of Health?
- What was it for?
Consequences of Disclosure Violations
Healthcare providers may be subjected to a variety of consequences when it comes to the violation of HIPAA or the Privacy Rule. The healthcare provider and the facility in which they work may be subjected to civil suits in a variety of ways. Disclosing sensitive information or photos about the patient are a breach of legal duty—intentional or unintentional—are both forms of civil suits that can occur. Nurses may face disciplinary action from their state’s board of nursing. With the ever-growing form of social media, boards of nursing have been cracking down on improper use of social media and breaches in patient confidentiality. Job loss and fines are other consequences that may occur by themselves or in addition to any of the others listed above (6).

Self Quiz
Ask yourself...
Think back to your hospital policies.
- Do you recall any consequences listed in the policy?
- Are you required to take education regarding patient confidentiality through work?
- What kinds of consequences do you think would be appropriate for violating patient confidentiality?
- What do you think of healthcare providers using social media at work?
Patient Confidentiality in the Technology Era
There are many forms of technology today and there are many ways patient confidentiality can be violated by using it. Cell phones have become a staple in nearly everyone’s day-to-day life, so it would make sense that both healthcare providers and patients alike have them. While they are useful, cell phones can also cause problems. Unintentional or intentional filming or recording of patients or medical information can happen by staff, family members, or other patients. Family members or friends may call to ask about a patient, and it is important for the nurse to know hospital policy when it comes to verifying the identity of those calling and what information can be given over the phone. Verifying with the patient who can be told what information is important as well (6).
Since charting has become electronic, many nurses are using computers, laptops, or tablets to complete their charting. Healthcare providers need to ensure that privacy is always maintained when utilizing these devices.
Even though most things can be transferred via email, call, or secured text message, some information still needs to be transmitted via fax machine. Since there is room for human error, coversheets should be used along with a clear identifier that the information being sent is confidential. If a number is used often, it is encouraged that it is preprogrammed into the fax machine to help decrease the chance of the number being mistyped (6).

Self Quiz
Ask yourself...
- What types of devices does your facility to use to chart?
- What steps has the facility taken to protect patient information when it comes to these devices?
- What steps do you take to protect patient information?
- Think of your work area.
- What things could be improved on when it comes to securing patient information?
Best Practices of Patient Confidentiality
Overall, healthcare providers must make decisions on how to protect private information. Despite recommendations from professional organizations and policies from facilities, it is the provider’s responsibility and decision on how to go about it. Sometimes there are several ways to solve the same problem. Best practices, like the ones listed below, can be used with hospital and Board of Nursing policies and rules (6).
- Utilize coversheets for person notes regarding patient care or when faxing sensitive information.
- Be mindful of what is said in semi-private rooms or rooms that have visitors. Curtains and walls are not soundproof.
- Verify callers before providing any patient information as determined by hospital policy. Remember to also verify with the patient if able to do so. Some patients may not want family or friends to know about their condition.
- Do not leave patient information in a place where it can be easily seen by others. This includes personal notes, electronic or printed medical records, unlocked communication devices, etc.
- Ensure that all patient information is properly disposed of or destroyed prior to leaving work.
- Be mindful of what is posted on social media and be aware of possible unintentional disclosure.
- Provide education to staff regarding potential areas of misuse when it comes to patient information. Policies regarding improper use should be implemented. These policies should include areas of email, personal electronic data devices, and transmission of data electronically.
- Have staff and others who may need access to patient information such as students sign confidentiality agreements.
- Refrain from speaking about patients or their private information in areas where information can be overheard, such as cafeterias, hallways, elevators, waiting rooms.
- Ensure that policies are reviewed and updated periodically or as needed to reflect current healthcare laws and guidelines.
This is not a comprehensive list, and healthcare providers must use common sense and caution when sharing private patient information.

Self Quiz
Ask yourself...
- From this list what do you already do to protect patient information?
- From this list what would you add to your own list?
- What would you add to this list regarding protection of sensitive information?
Summary
The topic of patient confidentiality is very important to the patient-provider relationship. Without it, the entire relationship can deteriorate, leading to significant emotional and possibly physical damage. This can be detrimental to the patient and provider. It is important to follow hospital policy and healthcare laws regarding sensitive information. All healthcare providers are strongly encouraged to stay up to date on new legislation that may affect patient confidentiality.
A Nurse’s Guide: How to Deal with Difficult Patients
Introduction
Being in the business of caring for people when they are at their worst means we often come face-to-face with patients amid emotional outbursts of anger. We can improve patient outcomes and our work-life satisfaction by putting the abilities to understand anger, learn and become aware of what goes on in others’ brains when they are upset, and adopt optimal techniques for handling these tough situations under our belt. Learning how to deal with difficult patients and being able to resolve conflict in a positive manner is one of the most valuable skills a nurse can possess.

Self Quiz
Ask yourself...
- Think of an interaction you’ve had with a patient who was angry.
- What was the outcome?
- Was it positive, or could it have gone better?
Consider Anger
Depending on your personal life, you will likely have your own opinion about anger as an emotion. Generally, it does not feel good to experience it in ourselves, nor is it pleasant to be around others who are feeling this way. Becoming angry is a part of being human, and as a healthcare professional, we must learn more about it so we are aware of how to deal with difficult patients. Perhaps approaching this from a philosophical standpoint will further help us to see beyond our patient’s immediate anger and we can work to develop a plan to resolve the conflict.
Anger as a Motivator
First off, anger can be motivating.
Oftentimes, when we perceive that there is a problem that is causing harm or injustice – whether it is affecting ourselves, a patient, the barista at the corner coffee shop, the planet, whatever – it is often anger that pushes us to act. As a very basic (and optimistic) example, a patient might be angry about being stuck in the hospital. Optimally, the experience will bother them enough to want to follow all of the steps their physician provides them so that they do not have to be readmitted.
Catharsis
For some, the act of being angry can be cathartic. For example, when we feel angry and begin to shout or slam a door, it is actually a way of releasing that built up, negative energy. Some people achieve catharsis and release their anger in productive ways, such as exercising, talking with a friend or therapist, journaling, or cleaning. Once you have completed the action and released the anger that you had, you slowly begin to calm down (1).
If we don’t release this energy over long periods of time, it can unfortunately cause physical harm. Anger increases heart rate, blood pressure (think MI or CVA), blood sugar, and intraocular pressure; lowers our immune function and increases incidents of cancer; affects the digestive system; decreases bone density, and can be the cause of headaches and migraines. Being angry also negatively impacts our short-term memory as well as the ability to make rational decisions (2). Applying therapeutic techniques can be a beneficial method of how to deal with difficult patients, as this can provide the opportunity to help them release some of the pent-up emotion they have before it causes physical harm.
Control
When learning how to deal with difficult patients, we must consider the relationship anger has with control. When a person is in our care, there is undoubtedly at least one major thing going on with them that they cannot control; otherwise, they would be at home. Being in a hospital setting removes all of the controlled variables that the patient has been accustomed to from their daily life (i.e. foods, who they come in contact with and at what time, etc.) and a common response to this change is anger in an attempt to regain control of the situation (1).
Stress & Trauma
There is a strong correlation between people who carry a lot of anger inside of them and stressful life events, particularly childhood trauma such as neglect and physical abuse. There’s also an association between anger and psychiatric disorders such as bipolar disorder and borderline personality disorder. This is not surprising since many people with these and other psychiatric disorders experienced extreme stress and trauma in their youth (3).
I find that keeping these tidbits of information about anger in mind helps me with how to deal with difficult patients and allows me to maintain my own composure.
Explore Your Thoughts/Feelings/Opinions/Triggers
Self-awareness is extremely important when learning how to deal with difficult patients. Allowing ourselves to be aware of our own experiences, feelings, and triggers because can dictate how we respond to others in heated situations. For example, suppose you are someone who grew up in a household where you frequently experienced violence — in that case, you might respond in an unexpected, unhelpful, and unprofessional way when exposed to angry behavior from others, such as shouting back. On the flip side, perhaps you grew up in a household where there was little to no conflict and you are unsure of how to properly respond when someone behaves angrily towards you. Maybe you have been judged harshly for your feelings and/or resulting actions, and consequently, judge others the same in turn.
Oftentimes we aren’t aware of our own tendencies until we step back and intentionally evaluate them. Considering your own experiences, thoughts, judgments, and things that trigger you can help you to become aware of why you react to situations the way that you do. You’ll then be more prepared to respond in a deliberate way when you next find yourself in a scenario with a disgruntled patient.

Self Quiz
Ask yourself...
- Have you ever gotten so upset that you made a bad decision?
- Has anger ever motivated you?
- What is your opinion of anger? How do you respond to others when they are angry?
- Think of at least three benefits of getting anger out.
Common Practice
“Calm down!” and, “It’s not okay to yell!” yelled the nurse. We’ve all heard the countless ways healthcare professionals respond when figuring out how to deal with difficult patients who are angry. Maybe we have even found ourselves yelling similar statements as well, and that’s okay – we are all human, and being yelled at can be very triggering, Don’t be too hard on yourself, evaluate how you should respond next time and prepare for it as best as you can because dealing with difficult patients is inevitable.
Often, clinicians become triggered – in other words, we get angry or irritated ourselves when confronted with an angry patient. If we aren’t mindful of our own tendencies and subsequently give in to that trigger, we inadvertently make what’s going on with the patient about ourselves when the patient is the one who needs our care. How is it helpful if we become upset as well? When learning how to deal with difficult patients, keep in mind that by responding with anger or with words that are seeking to control, the patient will miss an opportunity to release their pent-up, intense energy which can result in physical harm.
I am reminded of a time when my daughter was an infant. She always had a terrible time facing backward in her car seat. We were riding with a friend of mine and her six-year-old son when my daughter began to cry. The young boy covered his ears, saying, “Why does she have to be so loud?” My friend’s golden response was, “I know, honey, it’s no fun, but think how much worse it must be for her.”
Even though this scenario is quite different from a healthcare environment, I think those same words whenever I hear one of my patients yelling or are upset about something. All I want to do is cover my ears, but by thinking of how much worse it must be for them, I’m able to avoid making it about me.
Distraction
Another common approach to dealing with difficult patients during an angry episode by utilizing distraction techniques. There are times when this application is going to be the best choice, particularly, when dealing with patients who are cognitively impaired (4). However, there are other instances where this technique may come off as insulting with otherwise oriented people and could exacerbate the issue.
An example of an appropriate time to utilize this technique would be when dealing with a patient who has dementia and gets increasingly (and repeatedly) worked up over her belief that her loved one – who hasn’t seen the patient in recent history – is stealing from her. In this case, distraction might be the only way to calm her down.
Giving Advice
I work in a psychiatric setting, and when I was new to my position, I learned first-hand one technique that was not effective.
A 40-year-old, physically tall and sturdy male patient became so upset that he started punching our walls. Staff intervened and ending up having to take him down to the carpet for everyone’s safety. Other than his increase in rate and depth of breathing, he was lying quietly, prone on the ground. I kept a safe distance and asked if he was alright: he didn’t respond. I wasn’t sure what to do or say. I was new, undoubtedly nervous, and hadn’t yet learned the value of what one of our psychiatrists refers to as “therapeutic silence.” I had learned in the past from my education and own personal experiences that breathing techniques were calming, so I tried saying, “it’s okay, just breathe.”
Subsequently, he began yelling at me. He was saying not to tell him what to do, that he hated me, and to go away. By suggesting something to him in that intense moment, he took offense. If I’m honest with myself, if I were upset and someone had said something similar to me, it might not have gone over much better.
Threatening
Although this should only be used when absolutely necessary, nurses must be able to learn and understand how to deal with difficult patients through utilizing threatening tactics. Where I work, some patients simply live for the three smokes a day that they’re allowed. An example of this threatening tactic sounds something along the lines of, “if you don’t do what I say, you’re not going to get your cigarette.” Please note that this approach should not be utilized all the time, but in some cases, it can seem like the only way to get through to your difficult patients. However, keep in mind that it is a way of trying to control the other person and is also a missed opportunity to increase trust between the patient and the nurse.

Self Quiz
Ask yourself...
- Can you think of other ways of handling patients who are angry?
- What techniques have you employed?
- How effective have they been?
Benefits of Learning How to Deal with Difficult Patients When They are Angry
As caregivers, we experience more job satisfaction when we can adequately learn to care for people who are angry. Imagine how rewarding it is to successfully manage situations and achieve positive outcomes for our patients that could’ve gone badly otherwise. Not only that but, we potentially run the risk of losing our jobs if we don’t learn this essential skill (see Case Study #2 below). Rapport increases when appropriately utilized techniques are applied in practice because they foster trust and show respect for what the patient has to say (8).
For patients, these situations serve as great opportunities for them to release some of their anger. If we can be facilitators, assisting them to come to a more even-keeled place, they will undoubtedly experience better outcomes. Additionally, a situation involving a an angry patient can become dangerous quickly, so it is critical that we learn these skills for our own safety, and that of our patients.

Self Quiz
Ask yourself...
- Can you think of other benefits?
- Can you think of a time when you experienced first-hand or observed a situation involving a patient who was angry become worse because of how it was handled?
Anatomy Review
The amygdalae are a couple of bunches of neurons found deep in each temporal lobe that play an important role in our emotions, including triggering the fight or flight response (5). The hypothalamus is near the base of the brain right under the thalamus, and is attached to the pituitary gland (6). Among many other things, it’s responsible for controlling the secretion of hormones from the pituitary gland, which is located behind the nose (7). Finally, our adrenal glands sit on top of our kidneys and put out different kinds of hormones, particularly, stress hormones (2).
The Hormone Cascade
Something triggers us (i.e. we’ve just sat down to chart, and the call light goes off for what seems like the hundredth time, and we haven’t eaten or used the bathroom all day). Our amygdalae, like canaries in a coal mine, sound the alarm by signaling the hypothalamus and release a corticotropin-releasing hormone — causing the pituitary gland to release adrenocorticotropic hormone. This chain of hormone releases tells the adrenals to drop big stress bombs: adrenaline, noradrenaline, and cortisol (2).
When there’s too much cortisol, increased calcium is allowed to get into our neurons, which can end up leading them to die. Our prefrontal cortex (PFC) and hippocampus suffer the most from this unfortunate outcome. The function of the PFC becomes suppressed, which affects our ability to have good judgment. For example, saying something hurtful or that you do not mean to someone you care about during an argument. Following, when neurons die in the hippocampus, this is where our memories are stored. So if it’s not working well, our short-term memory and ability to store new ones are affected most (2).
The presence of too much cortisol will also result in a lack of serotonin – the happiness neurotransmitter. With less serotonin, we feel more sensitive to pain, anger, increase in aggression, and more prone to depression (2).
Consider every time you’ve ever tried to reason with a person who was already upset. How did it go? Did they immediately come to see the error of their ways? I can think of several occasions where a patient was so enraged about something that fixing whatever the issue was did nothing to quell the tirade. When trying to figure out how to deal with difficult patients, understanding what is going on in their brain during these episodes of rage can help us to make sense of it all and how to plan a deliberate, appropriate, and effective way to resolve the conflict.

Self Quiz
Ask yourself...
- Have you ever experienced being so angry that you experienced an amygdala hijack?
- If so, would you have called yourself “reasonable” when you were in that state?
- Consider the last time you dealt with someone who was angry in light of the above cascade of events. Does it make more sense now (if you weren’t already aware of what happens)?
Tips for Handling Patients When They are Angry
Beyond this lesson, you will find several publications that discuss in-depth how to manage de-escalation during potentially dangerous situations. De-escalation involves maintaining a calm demeanor and avoiding attempts to control the patient. As a result, they feel respected, and the trust between the two of you builds. Every person and situation is different, so a certain amount of intuition is also essential in order to creatively develop solutions (9).
Safety First
Since we now know that during escalated, angry situations, our patient’s brains are not exactly functioning at full capacity so try your best to expect the unexpected. One moment, a patient can seem like the calmest, and most collected person in the world — then they get triggered, and who knows what could happen?
With this in mind, the first thing we always have to consider is safety – for ourselves, the patient, and others nearby. Here are some recommendations for keeping everyone as safe as possible:
- Be aware of what’s around you and your patient. Are there things that could be thrown or used as a weapon? Do you wear necklaces or long earrings that can be pulled?
- Always maintain a safe distance. If you don’t feel safe, get to safety. It’s okay to walk away from a situation if you feel that you are in danger, but never turn your back.
- Bring a co-worker if you need to go into an angry patient’s room – never go alone.
- Observe for signs of aggression. If your patient exhibits balled fists, getting too close to you, pacing, tense shoulders, glaring, tense jaw, facial flushing, shouting, or heavy breathing, be prepared.
- Try to keep the area clear of others who might be put in danger or exacerbate the situation. This might be a challenge when you’re focused on engaging with your patient. However, it is helpful if you and your coworkers are all on the same page. Consider working with management to train everyone to be on alert for potentially dangerous situations with patients and their loved ones.
What to Say or Not to Say
When I’m upset, the thing that helps me the most is feeling like I am being heard. For my patients, I have found that listening is one of the tactics that works best, but remember that in some instances, patients may have a hard time listening to others because they may become triggered. If that occurs, it can become difficult to maintain a calm demeanor that is necessary for de-escalating tense situations. If we can find a way to keep the focus on the other patient (who is coming to us with the issue), we can become better listeners and remain calm.
Listening is a skill that not everyone excels in but it can make a huge difference when figuring out how to deal with difficult patients.
Tips to improve listening skills:
- Do not interrupt.
- Give your full attention rather than getting distracted by inner thoughts or environmental stimuli.
- Repeat back what you’ve heard to affirm you got it right.
- Ask related questions to show you’re concerned and want to deepen your understanding.
- Convey a sense of empathy by using your body language, and making brief statements like, “That’s understandable.”
Since there is not a specific prescription or solution for dealing with all angry patients, we need to stay tuned and be creative to reach a mutually beneficial goal. By staying calm and truly listening, we’re better able to understand what is going on so that we can attempt to remedy whatever the problem is when the time is right. After listening, affirming, and giving the patient time to calm down, we can begin to work toward a solution. For example, I might say, “I hear that you’re upset about what happened, and that’s totally understandable. What can I do for you right now to help?” By approaching the situation this way, it affirms that I heard the patient, respect their feelings, and genuinely want to help them. When learning how to deal with difficult patients, this is an extremely valuable tool to possess.
Additionally, body language is extremely important – it conveys so much! Simple adjustments like squaring ourselves to whomever we’re listening to and conveying accurate facial expressions depending on the situation ensures in the patient that we are giving them our full, undivided attention and that we truly care about what they’re saying.
Boundaries
A word about maintaining boundaries; these are key! Just because I aim to listen and convey kindness actively does not mean that I am a pushover, and that my patients will get everything they want.
For example, as nurses, we all know that we often don’t have the time (or energy) to have deep, confiding conversations with each and every patient. However, being kind can be done swiftly, and without caving to demands. A simple “no” can be said in a respectful manner. For example, we can briefly say in a kind tone, “I know it’s frustrating, and I get it, but unfortunately, I can’t talk with you right now because I’m in the middle of passing meds. Can we talk in half an hour or so?”
There are also times when we have to set boundaries because we can see that we can’t do any good in that moment. I have a patient who shouts so loudly when she’s upset that I have to cover my ears for fear of damage! Sometimes she’s able to convey her feelings in a way that I can actively listen to, and these times seem to be helpful for her, but when she can’t, I give her boundaries. I say, “*Pema, I want to listen to you, but you’re hurting my ears.” If she’s unable to control her volume, I gently remove myself, stating, “I hear that you’re having a hard time, but I have sensitive ears, and your shouting is hurting them. Let’s talk later.”
We all have to figure out where our boundaries lie. If you are someone who gets triggered by the angry behavior of others, you might do best to excuse yourself early on to catch your breath and ask someone else to help with the situation. If you are triggered, it’ll be tough for you to make the best decisions when figuring out how to deal with difficult patients.
Not Taking Things Personally
As nurses, I am sure we have all learned early on to not take anything personally, especially when dealing with difficult patients. In most cases, an angry patient yelling in your face will not be your fault. Remember, we are not responsible for other’s feelings and reactions; those are about them, not us. As we mentioned previously, we are all probably guilty of saying something that we didn’t mean when we were upset and we wish we would have given it a second thought, and in some scenarios, this could be the case. However, there are other instances where the angry behavior of a patient then results in them wanting to speak with your manager regardless of whatever the reason is being your fault or not.
It’s helpful to recognize when a behavioral response is not in proportion to what actually happened because this can be a clue into possible long-standing issues. Of course, knowing all of this doesn’t mean we shouldn’t always do our best, but it can help us refrain from beating ourselves up too much when our best seems to fall short.
Attempt to be aware of the things we have reviewed here so you can effectively handle and devise a solution on how to deal with difficult patients who are angry. Bear in mind how challenging it can be not to have control, especially during situations where we are unable to make rational decisions.
What to Do if You’re the One to Lose Your Cool
As we discussed earlier, when we become triggered, our prefrontal cortexes (PFCs) don’t work properly, and that is when our decision-making becomes poor. The good news is that, since we know what’s going on in our brain, we can work on reactivating that precious (and potentially life-saving) PFC. At first, we might not be able to look at ourselves clearly until after an episode, but we can learn to recognize the signs of becoming triggered by examining what happened. Once we can do that in real-time, we can intentionally work toward becoming calm again.
Take Care of Yourself
Nurses are used to taking care of others all the time, but what about themselves? This is crucial. You must take care of and be kind to yourself. Our best is different every moment of every day, and that’s all just part of being human. Some days, we might be having a tough time, struggling with any number of things, just like our patients. Our temper might be shorter, our tone may be a little more on edge, but rather than judging ourselves too harshly, we should recognize our own humanity and just do our best.

Self Quiz
Ask yourself...
- What kind of training have you received where you work on safety?
- If none, is there an opportunity for growth in this area?
- List three things that help calm you if/when you get upset.
- Think of when you’re listening to a patient. What do you do to show you’re actively listening?
- What are some phrases you would feel comfortable saying that would show that you care and are actively engaged? (For example, “That sounds frustrating.”)
Case Studies
Case Study #1
A 46-year-old female patient received an IM injection in her right glute this morning. It is afternoon shift change, and she is complaining that her right hip has been hurting since receiving this injection. She has repeatedly been approaching the nurse’s station about this issue. The off-going day shift nurse calls over his shoulder as he’s frantically attempting to finish documenting, “I’ve already assessed you, and I don’t see anything wrong. I talked to the doctor, and he ordered Ibuprofen which you received. I have let her know that you would like to speak with her; you’ll have to wait until she rounds next.”
The patient begins yelling, stating, “None of you care about me! My doctor doesn’t care about me! Otherwise, she wouldn’t make me get these injections that hurt me!” The evening shift nurse arrives, sees that the patient she knew from the evening before is upset and that the off-going nurse is busy. The evening nurse steps behind the station desk so that there’s a barrier between her and the patient (in case she becomes more agitated and aggressive) and turns to face the patient with a concerned expression in place. “*Fiona, I see that you’re upset. How can I help?” The nurse listens, not interrupting the patient as she relays her issue. At a natural lull in the patient’s speech, the nurse responds, “It sounds like you’re frustrated about this situation. I get it; that’s totally understandable.” The patient goes on to express her feelings of not being cared for by the staff or the doctor, tearfully raising her voice. The nurse looks at the patient with concern and considers the possibility that this woman might have some history of not being cared for. She continues to listen as the patient goes on venting. Eventually, the patient shouts one last time, turns away, and stomps down the hall to her room. An hour later, she returns looking tired, a little embarrassed, but calm, and apologizes then thanks the nurse for listening.
The above is based on an episode that I experienced about a year ago. This patient is still at the facility I work at, and I have not seen any such outbursts from her since. I can also attest to experiencing very good rapport with her since this event.
Case Study #2
A 70-year-old male patient rings the call bell. The nurse answers and the patient shouts loud enough to be heard without the aid of the speaker, “Get over here! You people are useless! Because of you, I’m swimming in a puddle of my own urine.” The nurse responds, “Okay, but you don’t have to be so rude.” She slams the phone down, muttering expletives to herself. She takes her time, finishing up what she was working on, still ruminating over the patient, while he gets increasingly upset.
She walks into the patient’s room, and she sees that he’s standing next to his bed, naked, leaning precariously on his IV pole. She says, “What are you doing? You’re going to fall.” The patient responds, “Well, you’re not doing your job!” “I shouldn’t have to deal with this,” the nurse mutters under her breath as she begins to gather the soiled sheets. The nurse, whose back is turned to the patient, doesn’t see that his face has gone the color of a bag of packed RBCs, his eyes are bulging, and his knuckles are white as they grip the IV pole. The patient attempts to use the pole as a weapon to hurt the nurse but ends up slipping on his urine-wet feet, striking his head against the wall, resulting in a concussion. He files an official complaint regarding the nurse, considers suing her for damages, and gets written up for the second time. Next time, she’ll be out of a job.

Self Quiz
Ask yourself...
Think of one example from your practice that you have experienced or observed that went well and another that did not.
- What were the key elements that you think made the difference?
Conclusion
People get angry – it’s just a fact of our existence. Some, unfortunately, misbehave when they feel anger whether it’s out of frustration, stress, feelings of loss of control, or unmanaged old triggers coming to the surface. As nurses, we often have to figure out how to deal with difficult patients while being able to remain calm and composed. By understanding more about people who experience excessive anger and learning to apply the techniques discussed in this course, you will be able to form flexible and creative solutions that can result in making the best out of very challenging situations.
How to Reduce New Nurse Turnover
Introduction
Before graduating from nursing school, I was accepted into a six-month program to train for the cardiac medical ICU. I took the initial competencies and classroom trainings and was assigned an experienced preceptor on the ICU floor. My preceptor very quickly informed me that I was bothering patients by being too attentive. Soon after, she let the rest of my colleagues know that she would be retiring because the job had become dangerous now that so many new nurses were joining our unit. That was just the first week on the floor.
Throughout my first year of nursing, I was anxiety-ridden and questioned staying. Despite my rough start, I made it through and have enjoyed over 20 years as a nurse; however, many of my classmates not only resigned before their first year was over, but a few left nursing altogether.
During my tenure as a nurse, I have learned that incivility and bullying are all too common. In a 2017 report, Nurses Eat Their Young: A Novel Bullying Educational Program for Student Nurses, the author references research that indicated bullying and incivility among peers occurred to at least 30% of nurses. Among new nurses, 73% reported experiencing incivility or bullying in their first month in practice (3). Below, I have listed just one example from a nursing blog that showcases how bullying and incivility haven’t changed much from my experiences with it over 20 years ago.
“I have an orientation with a nurse educator. And she’s kind of a bully; I have to say. She puts me in uncomfortable situations. She dismisses anything I say; she gives me ridiculous and menial assignments while excluding me from doing tasks with her directly related to my new role, that I could learn better. Yet, she talks over and over about the things I already know. She gives me contradicting information. At this point, my self-esteem has got even lower than when I started” (15).
In response: “This is the issue I have with the profession… more than likely, they pounced on you because you’re new, and they’re asserting their dominance/reinforcing cliques (them vs. us). Either behavior making for toxic workplace culture… And I say this from experience” (15).

Self Quiz
Ask yourself...
- What was your own experience as a new graduate nurse, and what impact does that have on your career today?
New Graduate Nurse Turnover Rates
The overall nurse turnover rate has increased 5% over the last decade; however, the new graduate nurse turnover rate alone has increased that much in just four years (4,10).
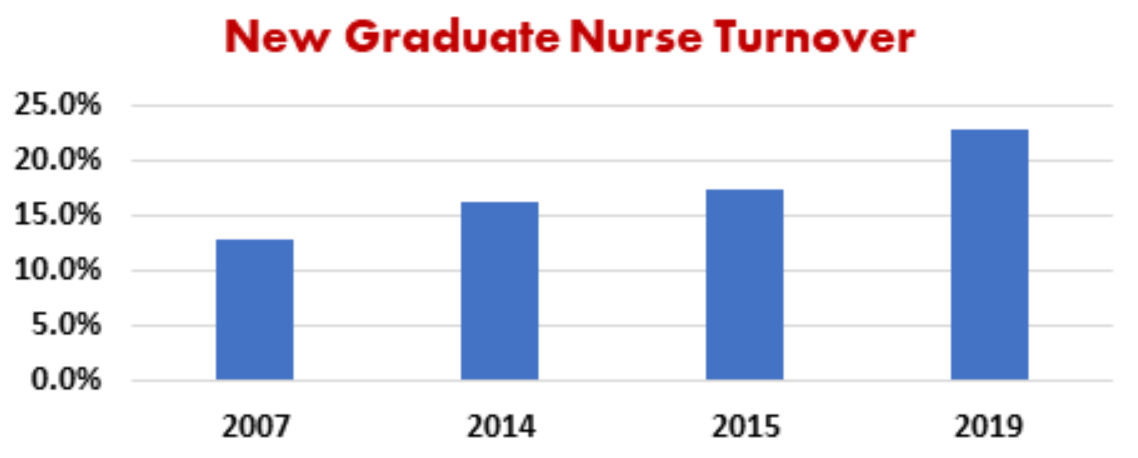
After only their first year, the new nurses’ turnover rates continue to rise until almost half of them have either left their departments or nursing in its entirety (4).
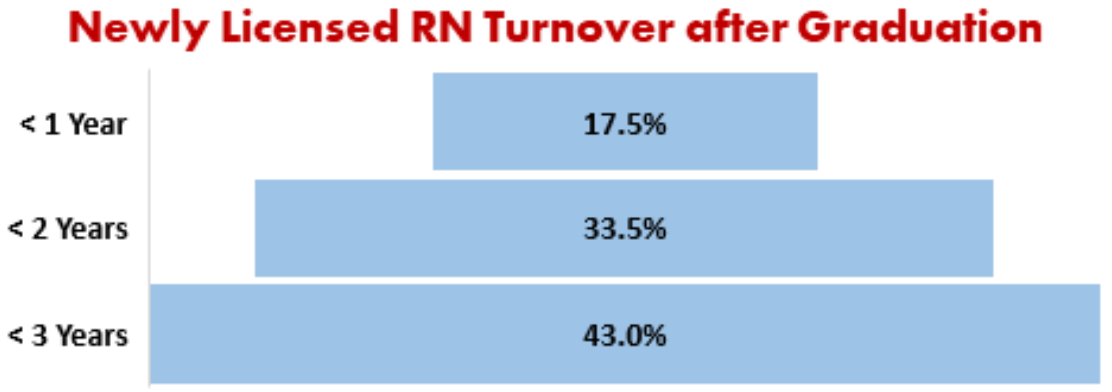
Of further concern, in a 2020 The Nursing Solutions, Inc. nurse turnover report, they project a significant increase in nurse deficits as a result of the COVID-19 pandemic (11). The report surveyed over 1000 nurses, and the results determined that 96% of respondents showed signs of burnout, and 56% reported they would be leaving either direct patient care specialties or the nursing profession in its entirety through resignation or retirement (11).

Self Quiz
Ask yourself...
- Thinking of your fellow nurse graduates, what percentage do you predict will leave the nursing field and why?
Reasons for New Nurse Turnover
There are various reasons as to why new nurses are leaving the field and contributing to the increase in nurse turnover; however, there is one trend that has remained consistent for decades. The initial peer-to-peer and orientation/precepting relationships established can truly make or break a new nurse.
Researchers often correlate the incivility and bullying of nurses to a lacking collegial or peer-to-peer relationships. Many nurses who cite bullying or incivility in the workplace often claim they are leaving the job due to their preceptors. For nurses with years of experience under our belt, since collegial relationships are a primary driver of turnover and retention for new nurses, we must assume responsibility for our part as peers and work to reduce the continuous rise in new nurse turnover.

Self Quiz
Ask yourself...
- How meaningful are collegial relationships to you at this point in your career versus your first year in nursing?
Effects of New Graduate Nurse Turnover
There is no argument that the cost of increasing new nurse turnover rates has all-encompassing effects. New graduates may lack the full in-person experience of nursing and are not fully prepared to meet all practice-based standards; this requires more hands-on training and nursing experience. Nurse-sensitive outcomes, including falls, pressure ulcers, and nosocomial infections, suffer in the hands of continual learners (8). Higher rates of mortality have been linked to higher turnover rates (6).
Although the training and precepting of new nurses is necessary on all accounts, it can be challenging and demanding for the already short-staffed and stressed nurses with experience. With the combination of continuous training and increased workload demands, patient satisfaction and community trust in the organization begins to erode (8). Employee morale for both new and experienced nurses suffer due to the increase in expectations and workload (6). In high patient volume scenarios, training and precepting may take the back burner to cover patient census, which leads to missed learning opportunities and perpetuates a lack of clinical expertise as the new nurses move forward in their career. This lack of knowledge can lead to intolerance or ridicule by the better-prepared nurse and possible disciplinary action for the up-and-coming nurse.
The cost for recruitment and hiring of new nurses along with the costs for filling vacated positions with travel and contracted nurses are estimated to be 5% of a hospital’s annual budget (6). Since labor cost accounts for up to 50% of the budget, productivity remains a top priority despite increased workload demands; leaving staff and administrators disconnected in determining actions that may positively affect patient and staff satisfaction.
I understand that these are not new statistics, and few nurses would knowingly jeopardize their safety and patient care. However, the fact remains that the culture persists, and the new nurses that receive this type of treatment pass it on. As part of the change process, our first action may start with recalling what it was like for us as new graduate nurses.

Self Quiz
Ask yourself...
- Do you have examples, either positive or negative, of nursing turnover affecting your unit’s patient care and satisfaction?
Challenges for new nurses
New nurses typically receive the “short end of the stick” when joining an organization, as the employer will most likely fill them in the neediest shifts, including nights, rotating, weekend, and holiday shifts. While this is not ideal for the new nurse, we accept it as part of the dues that they must make.
The Nursing Times Workforce reports that many nurses come into the field with anxiety (12). When I first became a nurse, I, too, experienced anxiety. I ended up mentioning my feelings to one of my colleagues who supportively advised me that my anxiety was a good sign; it indicated that I would be a more cautious nurse. I took comfort in this, but as I now reflect, I do not believe it to be the whole truth.
Cautiousness is a characteristic in and of itself, and although it can present as anxiety, the feeling of dread can be resolved with positive experiences that lead to confidence. The anxiety that I felt, and what new nurses typically describe tends to be fear-based, whether it is real or perceived. On top of this, up to 18% of hospital nurses report symptoms of depression which is double the general population (12).
When you couple this anxiety with incivility, bullying, or general lack of support, it becomes easy to see how the rates of new nurse turnover continue to rise. Below are just a few examples of sub-Reddit postings from current new nurses and the challenges they are facing with their mental health:
“My anxiety/depression has worsened to the point where I can’t sleep the night before I work and I’m constantly overthinking or worrying about my job. I’m miserable and on edge, and I feel like this just can’t be worth it. I was looking to move out of bedside nursing and was curious what my options are, especially with less than a year of experience” (17).
“Hello! I work dayshift med surg. My biggest issue is when I get home, I’m anxious. I think about my shift and worry I forgot something. I get nervous that when I come back the next day, the night nurse will pick me apart because I missed things. I sleep terribly in between shifts. I just always worry about what I did. Need advice. Does this happen to anyone else? Best tips to not worry?” (18).
“I am fresh off orientation and am beginning to suffer from anxiety attacks while at home. I wake up in sweats thinking about my unit. I feel weak because my peers are not feeling these same things. It’s disheartening knowing that I worked my butt off in nursing school to end up feeling like crap every day. I don’t know what to do. I hear it gets better, but now I’m questioning if I should’ve ever become a nurse. Caring for people is all I wanted to do, but maybe I wasn’t cut out for this” (19).

Self Quiz
Ask yourself...
- What advice would you give to support other nurses with anxiety or depression?
Bullying and Incivility
The American Nurses Association defines bullying as “repeated, unwanted harmful actions intended to humiliate, offend and cause distress in the recipient” (2).
As previously mentioned, bullying is a prevalent issue in the field of nursing, and there are many speculations as to why it is common for nurses to bully their colleagues. One being, that nurses tend to garner less respect from other disciplines such as doctors or pharmacists. Other reasons may be due to the natural competitiveness of the healthcare professions, or the inability to control most of their work environment and patient outcomes so overstepping and bullying fellow nurses is their only constant form of control or normalcy (7). Common examples of bullying in nursing include verbal abuse and harassment.
Incivility is a form of bullying, except the intent is more ambiguous; so much so that it often goes unrecognized and can even be disguised as a learning opportunity. Incivility often gets ignored by management out of empathy for the experienced nurses being under stress, or out of fear of confronting a trained nurse and causing them to leave – contributing to the chronic short-staffing in healthcare facilities. Nurses who experience this behavior tend to pass it on as a rite of passage, leading to the perpetuation of nurses’ culture “eating their young” (4). Some signs of the behavior include (15):
Behavior | Examples |
Eye Rolling | Response to a new RN’s request for assistance. |
Disrespect | Intentionally not informing a new nurse of best practice or other information relevant to the organization. |
Gossip | Overstating or exaggerating a new nurse’s shortcomings, faux pas, or errors to co-workers. |
Blaming | Naming a new nurse as part of an incident report. |
Rudeness | Informing a new nurse of the burden you are undertaking by precepting. |
Unfriendiness | Refusal to greet or include a new nurse in social conversation. |
Ignoring | Being unavailable to the new nurse. A survey of new graduates revealed 27.5% of nurses reported preceptors were rarely or never available (4). |

Self Quiz
Ask yourself...
- Have you experienced or witnessed acts of incivility or bullying against yourself or your peers?
- Thinking back, how has your specific nursing unit handled acts of incivility or bullying?
How to Support New Nurses
In the article, “4 Compelling Theories Why Nurses ‘Eat Their Young,’” Maura Hohman says, “The number one most powerful behavior is for the witness to speak up and support the person who is being targeted (7).” While this is easier said than done, there is evidence that developing a script to confront individuals when this occurs can be useful (3). At the very least, it shows support for the new nurse. Other essential activities to improve instances of incivility and bullying in the workplace while reducing the new nurse turnover rate include:
- Becoming familiar with your organization’s policies and procedures on incivility, bullying, and workplace violence. If your organization does not address this issue, it is your responsibility to recommend and participate in developing the needed policies. The American Nurses Association’s “Nurses Bill of Rights” is a useful reference (2).
- Advocating for education on recognizing and preventing incivility and bullying through your professional association, nursing schools, and organization (3).
- Practicing “Just Culture.” Unless the same error occurs repeatedly, the new nurse’s intent is your primary tool for guiding consequences. Never blame or name if unnecessary when reporting an error. Limit your information to the facts only. Mistakes are to be investigated for the root cause, which is rarely person-related, and almost always process, culture, and system design.
- Learning opportunities are just that; don’t chastise. If you are angry or irritated, consider your real intent. Learning opportunities are rarely cultivated in an emotional environment.
- Being a supporter of other nurses.
- American Nurses Association’s civility best practices include:
- Strive to develop clear verbal and non-verbal communication. Be direct when needed and always respectful.
- Treat others with kindness, as well as collegiality, and always dignity.
- Be mindful that every individual suffers, and your actions and words affect others.
- Avoid gossip and call it out when you hear it from others.
- Rely on facts; never speculate and be slow to conclude until evidence has been discovered.
- Be collaborative and share information when appropriate.
- Offer assistance and accept appropriate refusal graciously.
- Be aware, accountable, and responsible for your actions.
- Speak directly to the person with whom you have an issue.
- Seek other points of view, perspectives, and experiences. Listen to others with interest.
- Apologize when necessary.

Self Quiz
Ask yourself...
- Are you knowledgeable of your hospital’s policies on incivility, bullying, and workplace violence?
- Do your hospital policies align with the American Nurses Association?
Recognizing Burnout and Opportunities to Reduce New Nurse Turnover
Since a lack of collegial relationships and peer-to-peer support are contributing factors leading to burnout and turnover, there is a lot you can do to prevent both. Besides following the steps above, recognizing burnout and signs of pending turnover are essential to quick intervention. The symptoms of burnout are noticeable in this at-risk population who may begin:
- Not participating in social activities.
- Not participating in improvement activities or opposing workplace changes.
- Calling off shifts, especially when they have been highly dependable.
- Arriving late for their shift.
- Taking excessive breaks or leaving the floor for support personnel activities when not necessary.
- Presenting with a negative attitude or being insensitive to patients and families.
- Verbalizing overwhelming anxiety or dread at coming to work (14).
If you notice these behaviors, it is time to intervene in order to avoid nurse turnover. One of the best strategies is to become a mentor or friend to them. Having someone to vent to helps relieve stress, and your engagement will go a long way in building positive experiences for the new nurse (14). If you have an employee assistance program, refer them to your human resources depart and inform them of all the available resources that you know of. Employee assistance programs offer confidential counseling for many personal and work-related concerns. If the situation persists, get your manager involved. It is their job to know and offer additional supportive resources to their employees.

Self Quiz
Ask yourself...
- Can you think of a nurse who your outreach may support?
Conclusion
There are many contributing factors to new nurse turnover. It is the responsibility of healthcare organizations, professional associations, and nursing educators to work together to improve the barriers that are causing this consistent increase in nurse turnover rates that are further contributing to the global nursing shortage. In order to deliver quality patient care, improve health outcomes, and increase workplace satisfaction we need nurses.
No matter how much experience you have, there are ways you can contribute to ending this increasing new nurse turnover, and that is by becoming an advocate and mentor for them. Speak up to support a new nurse and become familiar with your organization’s incivility, bullying, and workplace violence policies.
References + Disclaimer
Human Trafficking – Michigan
- https://polarisproject.org
- https://humantraffickinghotline.org/state/michigan
- https://www.dhs.gov/blue-campaign/what-human-trafficking
- United Nations Office on Drugs and Crime. (2016). Global report on trafficking in persons, 2014. New York, NY: United Nations.
- https://www.justice.gov/humantrafficking/what-is-human-trafficking
- https://www.cdc.gov/violenceprevention/sexualviolence/trafficking.html
- https://polarisproject.org/2019-us-national-human-trafficking-hotline-statistics/
- https://polarisproject.org/wp-content/uploads/2019/09/LGBTQ-Sex-Trafficking.pdf
- Hachey, L., & Phillippi, J. (2017). Identification and management of human trafficking victims in the emergency department. Advanced Emergency Nursing Journal, 39(1), 31–51.
- Doi: 10.1097/TME.0000000000000138
- https://swmihumantrafficking.org/michigans-human-trafficking-law/
- 11.https://www.michigan.gov/documents/ag/Safe_Harbor_for_Trafficking_Victims_693456_7.pdf
- https://humantraffickinghotline.org/what-human-trafficking/federal-law
- https://www.michigan.gov/mdhhs/0,5885,7-339-73971_7119_50648_44443-157836–,00.html
- Update: Identifying human trafficking patients alert. Patient Safety Monitor Journal. 2018;19(9):6. Accessed October 31, 2020. http://search.ebscohost.com/login.aspx?direct=true&db=ccm&AN=131246408&site=eds-live
- Identifying Victims of Human Trafficking: What to Look for in a Healthcare Setting. Journal of Legal Nurse Consulting. 2020;31(3):30-33. Accessed October 31, 2020. http://search.ebscohost.com/login.aspx?direct=true&db=ccm&AN=145452392&site=eds-live
- https://www.state.gov/identify-and-assist-a-trafficking-victim/
- National Human Trafficking Hotline. Comprehensive human trafficking assessment tool. Retrieved from https://humantraffickinghotline.org/sites/default/files/Comprehensive%20Trafficking%20Assessment.pdf
- https://www.acf.hhs.gov/sites/default/files/orr/fact_sheet_sex_trafficking.pdf
Michigan Pain and Symptom Management for Nurses
- https://www.cdc.gov/nchs/products/databriefs/db390.htm
- Institute of Medicine. (2011). Relieving pain in America: A blueprint for transforming prevention, care, education, and researchpdf iconexternal icon. Washington, DC: National Academies Press
- https://www.merriam-webster.com/dictionary/pain
- Nahin, R. (2012). Estimates of pain prevalence and severity in adults: United States. Journal of Pain, 16(8), 769-80. doi: 10.1016/j.jpain.2015.05.002
- Yam, M., Loh, Y., Tan, C., Adam, S., Manan, N., & Basir, R. (2018). General pathways of pain sensation and the major neurotransmitters involved in pain regulation. International Journal of Molecular Sciences, 19(2164), 1-23. doi: 10.3390/ijms19082164
- Swift, A. (2018). Understanding pain and the human body’s response to it. Nursing Times, 114(3), 22-26. Retrieved from https://www.nursingtimes.net/clinical-archive/pain-management/understanding-the-effect-of-pain-and-how-the-human-body-responds-26-02-2018/
- https://www.cdc.gov/media/releases/2016/p0315-prescribing-opioids-guidelines.html
- https://www.michigan.gov/documents/lara/LARA_DHHS_Opioid_Laws_FAQ_05-02-2018_622175_7.pdf
- https://healthteam.msu.edu/patients/Policies-Forms/opioid-laws-FAQ.aspx
- https://www.michigan.gov/opioids/0,9238,7-377-88143_88345—,00.html
- Griesler, P., Hu, M., Wall, M., & Kandel, D. (2019). Medical use and misuse of prescription opioids in the US adult population: 2016-2017. American Journal of Public Health, 109(9), 1258-65. doi: 10.2105/AJPH.2019.305162
- https://www.michigan.gov/mdhhs/0,5885,7-339-71550_2941_4871_79584—,00.html
- Mills, S., Nicolson, K., & Smith, B. (2019). Chronic pain: a review of its epidemiology and associated factors in population-based studies. British Journal of Anesthesiology, 12(2), 273-283. doi: 10.1016/j.bja.2019.03.023
- Dahan, A., Velzen, M., & Niesters, M. (2014). Comorbidities and the complexities of chronic pain. Anesthesiology, 121(4), 675-677. doi: 10.1097/ALN.0000000000000402
- https://www.mhanational.org/chronic-pain-and-mental-health
- Mir, H. Miller, A., Obremskey, W., Jahangir, A. & Hsu, J. (2019). Confronting the opioid crisis: practical pain management and strategies. The Journal of Bone and Join Surgery, 101(23), 1-6. doi: 10.2106/JBJS.19.00285
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Fifth edition. 2014.
- Wardhan, R., & Chelly, J. (2017). Recent advances in acute pain management: understanding the mechanisms of acute pain, the prescription of opioids, and the role of multimodal pain therapy. F1000 Research, 6(2065), 1-10. Doi:10.12688/f1000research.12286.1
- https://static.practicalpainmanagement.com/sites/default/files/pain-management-medications.pdf
- https://www.cdc.gov/drugoverdose/training/nonopioid/508c/
- Ackley, B. J., Ladwig, G. B., Msn, R. N., Makic, M. B. F., Martinez-Kratz, M., & Zanotti, M. (2019). Nursing Diagnosis Handbook E-Book: An Evidence-Based Guide to Planning Care. Mosby.
- Hemmatipour, A., Karami, F., Sadouni, Z, Hatami, A., Jahanirmehr, A. & Saberipoiur, B., (2020). A comparison between nurses’ and patients’ views on barriers to pain management. Journal of Nursing and Midwifery Sciences, 2018(5), 47-52. Doi: 10-4103/JNMS.JNMS_16_18
- https://www.jointcommission.org/media/tjc/newsletters/quick_safety_drug_diversion_final2pdf.pdf
Opioid Abuse
- https://www.deamuseum.org/ccp/opium/history.html
- https://americanaddictioncenters.org/opiates/controlled-substances
- https://www.cdc.gov/injury/features/prescription-drug-overdose/index.html
- https://www.cdc.gov/drugoverdose/prescribing/guideline.html
- https://www.cdc.gov/drugoverdose/pdf/guidelines_at-a-glance-a.pdf
- https://www.cdc.gov/drugoverdose/pdf/pdo_checklist-a.pdf
- APA Webster, Lynn R. MD Risk Factors for Opioid-Use Disorder and Overdose, Anesthesia & Analgesia: November 2017 – Volume 125 – Issue 5 – p 1741-1748 doi: 10.1213/ANE.0000000000002496
- Andrea L. Nicol, Robert W. Hurley, Honorio T. Benzon Anesth Analg. Author manuscript; available in PMC 2018 Nov 1. Published in final edited form as: Anesth Analg. 2017 Nov; 125(5): 1682–1703. doi: 10.1213/ANE.0000000000002426
- Mart van Laar, Joseph V Pergolizzi, Jr, Hans-Ulrich Mellinghoff, Ignacio Morón Merchante, Srinivas Nalamachu, Joanne O’Brien, Serge Perrot, Robert B Raffa
- Open Rheumatol J. 2012; 6: 320–330. Published online 2012 Dec 13. doi: 10.2174/1874312901206010320
- Pak, S. C., Micalos, P. S., Maria, S. J., & Lord, B. (2015). Nonpharmacological interventions for pain management in paramedicine and the emergency setting: a review of the literature. Evidence-based complementary and alternative medicine: eCAM, 2015, 873039. https://doi.org/10.1155/2015/873039
- Safer D. J. (2019). Overprescribed Medications for US Adults: Four Major Examples. Journal of clinical medicine research, 11(9), 617–622. https://doi.org/10.14740/jocmr3906
- Dydyk AM, Jain NK, Gupta M. Opioid Use Disorder. [Updated 2020 Jun 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553166/
- https://www.cdc.gov/drugoverdose/training/oud/accessible/index.html
Vaping Induced Lung Injuries
- Centers for Disease Control and Prevention. (2019). Electronic cigarettes. Retrieved from: https://www.cdc.gov/tobacco/basic_information/e-cigarettes/index.htm
- Centers for Disease Control and Prevention. (2019). Smoking and tobacco use: for healthcare providers. Retrieved from: https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease/healthcare-providers/index.html
- Chatham-Stephens, K, et al. (2019). Characteristics of hospitalized and non-hospitalized patients in a nationwide outbreak of e-cigarette, or vaping, product use-associated lung injury. Morbidity Mortality Weekly, 68(1076-1080). Retrieved from: https://www.cdc.gov/mmwr/volumes/68/wr/mm6846e1.htm?s_cid=mm6846e1_w
- Dinikar, C. & O’Connor, G. T. (2016). The health effects of electronic cigarettes. The New England Journal of Medicine, 375 (1372-1381). Retrieved from: https://www.nejm.org/doi/full/10.1056/NEJMra1502466
- Halpern, S. D., et al. (2018). A pragmatic trial of e-cigarettes, incentives, and drugs for smoking cessation. The New England Journal of Medicine, 378(2302-2310). Retrieved from: https://www.nejm.org/doi/full/10.1056/NEJMsa1715757
- Martinelli, K. (2018). Teen vaping: What you need to know. Child Mind Institute. Retrieved from: https://childmind.org/article/teen-vaping-what-you-need-to-know/
- Rubinstein, M. L., et al. (2018). Adolescent exposure to toxic volatile organic chemicals from e-cigarettes. Pediatrics, 141(4). Retrieved from: https://pediatrics.aappublications.org/content/141/4/e20173557
- U.S. Department of Health and Human Services. (2016). E-cigarette use among youth and young adults: a report of the Surgeon General. Retrieved from: https://e-cigarettes.surgeongeneral.gov/documents/2016_SGR_Full_Report_non-508.pdf
LGBTQ Cultural Competence
- Waisel DB. Vulnerable populations in healthcare. Curr Opin Anesthesiol. 2013;26(2):186–92.
- Freid VM, Bernstein AB, Bush MA. Multiple chronic conditions among adults aged 45 and over: Trends over the past 10 years. NCHS Data Brief. 2012;2012(100):1–8.
- Institute of Medicine. Collecting sexual orientation and gender identity data in electronic health records: workshop summary. Washington DC: National Academy of Sciences; 2013.
- Quinn GP, Sanchez JA, Sutton SK, Vadaparampil ST, Nguyen GT, Green BL, et al. Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA-Cancer J Clin. 2015;65(5):384–400
- Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health. 2010;100(10):1953–60.
- Dilley JA, Simmons KW, Boysun MJ, Pizacani BA, Stark MJ. Demonstrating the importance and feasibility of including sexual orientation in public health surveys: health disparities in the Pacific northwest. Am J Public Health. 2010;100(3):460–7.
- Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay, and bisexual older adults: results from a population-based study. Am J Public Health. 2013;103(10):1802–9.
- Bauermeister J, Eaton L, Stephenson R. A multilevel analysis of neighborhood socioeconomic disadvantage and transactional sex with casual partners among young men who have sex with men living in metro Detroit. Behav Med. 2016;42(3):197–204.
- Smalley KB, Warren JC, Barefoot KN. Differences in health risk behaviors across understudied LGBT subgroups. Health Psychol. 2016;35(2):103–14.
- Staats C, Capatosto K, Wright RA, Jackson VW. State of the science: Implicit bias review 2016. Columbus: Kirwan Institute.
- Cochran SD, Bandiera FC, Mays VM. Sexual orientation-related differences in tobacco use and secondhand smoke exposure among US adults aged 20 to 59 years: 2003-2010 National Health and nutrition examination surveys. Am J Public Health. 2013;103(10):1837–44.
- Remafedi G, French S, Story M, Resnick MD, Blum R. The relationship between suicide risk and sexual orientation: results of a population-based study. Am J Public Health. 1998;88(1):57–60.
- Charlton BM, Corliss HL, Missmer SA, Frazier AL, Rosario M, Kahn JA, et al. Reproductive health screening disparities and sexual orientation in a cohort study of U.S. adolescent and young adult females. J Adolesc Health. 2011;49(5):505–10.
- Matthews AK, Brandenburg DL, Johnson TP, Hughes TL. Correlates of underutilization of gynecological cancer screening among lesbian and heterosexual women. Prev Med. 2004;38(1):105–13.
- Tracy JK, Lydecker AD, Ireland L. Barriers to cervical Cancer screening among lesbians. J Women’s Health. 2010;19(2):229–37.
- Grossman AH, D’Augelli AR. Transgender youth: invisible and vulnerable. J Homosex. 2006;51(1):111–28.
- Krehely J. How to close the LGBT health disparities gap. Center for American Progress; 2009. p. 1–9.
- Buchmueller T, Carpenter CS. Disparities in health insurance coverage, access, and outcomes for individuals in same-sex versus different-sex relationships, 2000-2007. Am J Public Health. 2010;100(3):489–95.
- Heck JE, Sell RL, Gorin SS. Health care access among individuals involved in same-sex relationships. Am J Public Health. 2006;96(6):1111–8.
- Kamen C, Palesh O, Gerry AA, Andrykowski MA, Heckler C, Mohile S, et al. Disparities in health risk behavior and psychological distress among gay versus heterosexual male Cancer survivors. LGBT Health. 2014;1(2):86–U103.
- Legal L. When health care Isn’t caring: lambda Legal’s survey of discrimination against LGBT people and people with HIV. New York: Lamba Legal; 2010.
- Grant JM, Mottet LA, Tanis J. National Transgender Discrimination Survey Report on health and health care. Washington DC: National Center for Transgender Equality and National Gay and Lesbian Task Force; 2010.
- Shires DA, Jaffee K. Factors associated with health care discrimination experiences among a National Sample of female-to-male transgender individuals. Health Soc Work. 2015;40(2):134–41.
- Eliason MJ, Dibble SL, Robertson PA. Lesbian, gay, bisexual, and transgender (LGBT) physicians’ experiences in the workplace. J Homosex. 2011;58(10):1355–71.
- Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25(6):445–54.
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8.
- Mereish EH, Bradford JB. Intersecting identities and substance use problems: sexual orientation, gender, race, and lifetime substance use problems. J Stud Alcohol Drugs. 2014;75(1):179–88.
- Torres CG, Renfrew M, Kenst K, Tan-McGrory A, Betancourt JR, Lopez L. Improving transgender health by building safe clinical environments that promote existing resilience: results from a qualitative analysis of providers. BMC Pediatr. 2015; 15:187.
- Burke SE, Dovidio JF, Przedworski JM, Hardeman RR, Perry SP, Phelan SM, et al. Do contact and empathy mitigate Bias against gay and lesbian people among heterosexual first-year medical students? A report from the medical student CHANGE study. Acad Med. 2015;90(5):645–51.
- Sabin JA, Riskind RG, Nosek BA. Health care Providers’ implicit and explicit attitudes toward lesbian women and gay men. Am J Public Health. 2015;105(9):1831–41.
- Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882–7.
- Wilson TD, Brekke N. Mental contamination and mental correction: unwanted influences on judgments and evaluation. Psychol Bull. 1994;116(1):117–42.
- Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit Bias in health care: a narrative review. Group Process Interg. 2016;19(4):528–42.
- Greenwald AG, Banaji MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychol Rev. 1995;102(1):4–27.
- Van Ryn M, Saha S. Exploring unconscious bias in disparities research and medical education. JAMA. 2011;306(9):995–6.
- Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998;74(6):1464–80.
- Nosek BA, Riskind RG. Policy implications of implicit social cognition. Soc Issue Policy Rev. 2012;6(1):113–47.
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
- Shavers VL, Fagan P, Jones D, Klein WMP, Boyington J, Moten C, et al. The state of research on racial/ethnic discrimination in the receipt of health care. Am J Public Health. 2012;102(5):953–66.
- Chapman EN, Kaatz A, Carnes M. Physicians and implicit Bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28(11):1504–10.
- Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment: Confronting racial and ethnic disparities in health care. Brian D. Smedley, Adrienne Y. Stith, and Alan R. Nelson, Editors; Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care; Board on Health Sciences Policy; Institute of Medicine. Washington, DC; 2003.
- Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41.
- Greenwald AG, Banaji MR, Nosek BA. Statistically small effects of the implicit association test can have societally large effects. J Pers Soc Psychol. 2015;108(4):553–61.
- Khan A, Plummer D, Hussain R, Minichiello V. Does physician bias affect the quality of care they deliver? Evidence in the care of sexually transmitted infections. Sex Transm Infect. 2008;84(2):150–1.
- Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P. (2019). Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC medical education, 19(1), 325. https://doi.org/10.1186/s12909-019-1727-3
- Human rights campaigns. Glossary of terms. Retrieved from https://www.hrc.org/resources/glossary-of-terms
- Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community, a field guide. Joint Commission. Retrieved from https://www.jointcommission.org/ /media/enterprise/tjc/imported-resource assets/documents/lgbtfieldguide_web_linked_verpdf.pdf?db=web hash=1EC363A65C710BCD1D4E14ED120CB2
- Delivering culturally sensitive care to LGBTQI Patients. The Journal for nurse practitioners. Volume 13, issue 5 p342-347.
Coronavirus: Nursing Considerations
- COVID-19 overview and infection prevention and Control priorities in non-us HEALTHCARE SETTINGS. (n.d.). Retrieved February 25, 2021, from https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/overview/index.html#background
- Commissioner, O. (n.d.). A Closer Look at COVID-19 Diagnostic Testing. Retrieved January 05, 2021, from https://www.fda.gov/health-professionals/closer-look-covid-19-diagnostic-testing
- Overview of Testing for SARS-CoV-2 (COVID-19). (n.d.). Retrieved January 05, 2021, from https://www.cdc.gov/coronavirus/2019-ncov/hcp/testing-overview.html
- Watson, J., Whiting, P. F., & Brush, J. E. (2020). Interpreting a covid-19 test result. Bmj, M1808. doi:10.1136/bmj.m1808
- Cascella M, Rajnik M, Cuomo A, et al. Features, Evaluation, and Treatment of Coronavirus. [Updated 2020 Oct 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554776/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7369540/
- Long-Term Effects of COVID-19. (n.d.). Retrieved January 11, 2021, from https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html
- J. (2020, December 28). A New Strain of Coronavirus: What You Should Know. Retrieved January 11, 2021, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/a-new-strain-of-coronavirus-what-you-should-know
- Dhont, S., Derom, E., Braeckel, E., Depuydt, P., & Lambrecht, B. (n.d.). The pathophysiology of ‘happy’ hypoxemia in COVID-19. Retrieved January 14, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7385717/
Effective Communication in Nursing
- Dictionary by Merriam-Webster: America’s most-trusted online dictionary. (n.d.). Retrieved February 22, 2021, from https://www.merriam-webster.com/
- Effects of poor communication in healthcare. (n.d.). Retrieved February 22, 2021, from https://www.hipaajournal.com/effects-of-poor-communication-in-healthcare/?amp
Flu Treatment, Symptoms, and Red Flags
- Centers for Disease Control and Prevention. (2012). Respiratory hygiene/cough etiquette in healthcare settings. Retrieved from:
- https://www.cdc.gov/flu/professionals/infectioncontrol/resphygiene.htm
- Centers for Disease Control and Prevention. (2017). How the flu virus can change: “drift and shift”. Retrieved from: https://www.cdc.gov/flu/about/viruses/change.htm
- Centers for Disease Control and Prevention (2018). Estimates of flu vaccination coverage among adults- US 2017-2018 flu season. Retrieved from: https://www.cdc.gov/flu/fluvaxview/coverage-1718estimates.htm#ref3
- Centers for Disease Control and Prevention (2018). Estimates of flu vaccination coverage among children- US 2017-2018 flu season. Retrieved from: https://www.cdc.gov/flu/fluvaxview/coverage-1718estimates-children.htm
- Centers for Disease Control and Prevention. (2018a). Influenza antiviral medications: summary for clinicians. Retrieved from: https://www.cdc.gov/flu/professionals/antivirals/summary-clinicians.htm#
- Centers for Disease Control and Prevention. (2018b). Influenza vaccination: a summary for clinicians. Retrieved from: https://www.cdc.gov/flu/professionals/vaccination/vax-summary.htm
- Centers for Disease Control and Prevention. (2018c). Overview of influenza testing methods. Retrieved from: https://www.cdc.gov/flu/professionals/diagnosis/overview-testing-methods.htm
- Centers for Disease Control and Prevention. (2018d). Prevention strategies for seasonal influenza in healthcare settings. Retrieved from: https://www.cdc.gov/flu/professionals/infectioncontrol/healthcaresettings.htm
- Centers for Disease Control and Prevention. (2018e). Preventing the flu: good health habits can help stop germs. Retrieved from: https://www.cdc.gov/flu/protect/habits/index.htm
- Centers for Disease Control and Prevention. (2018f). Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization
Nursing Documentation 101
- 29-1141 Registered Nurses. (2018, March 30). Retrieved March 1, 2019, from https://www.bls.gov/oes/2017/may/oes291141.htm
- Hendrich, A., Chow, M. P., Skierczynski, B. A., & Lu, Z. (2008). A 36-hospital time and motion study: how do medical-surgical nurses spend their time? The Permanente journal, 12(3), 25-34.
- Health IT Quick Stats. (2019, February 6). Retrieved March 1, 2019, from https://dashboard.healthit.gov/quickstats/quickstats.php
- Medical Practice Efficiencies & Cost Savings. (2018, August 13). Retrieved March 1, 2019, from https://www.healthit.gov/topic/health-it-and-health-information-exchange-basics/medical-practice-efficiencies-cost-savings
- Meaningful Use. (2017, January 18). Retrieved March 1, 2019, from https://www.cdc.gov/ehrmeaningfuluse/introduction.html
- Miller, L., Stimely, M., Matheny, P., Pope, M., McAtee, R. & Miller, K. Novice Nurse Preparedness to Effectively Use Electronic Health Records in Acute Care Settings: Critical Informatics Knowledge and Skill Gaps. (2014). Online Journal of Nursing Informatics,18(2). Retrieved March 1, 2019, from https://www.himss.org/novice-nurse-preparedness-effectively-use-electronic-health-records-acute-care-settings-critical
- HHS Office of the Secretary,Health Information Privacy Division. (2016, February 25). Individuals’ Right under HIPAA to Access their Health Information. Retrieved March 1, 2019, from https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/access/index.html
- Office for Civil Rights (OCR). (2015, December 18). 2000-Why is the HIPAA Security Rule needed and what is the purpose of the security standards. Retrieved March 1, 2019, from https://www.hhs.gov/hipaa/for-professionals/faq/2000/why-is-hipaa-needed-and-what-is-the-purpose-of-security-standards/index.html
- AHIMA Work Group (2013). Integrity of the Healthcare Record: Best Practices for EHR Documentation (2013 update). Journal of AHIMA,84(8), 58-62. Retrieved March 1, 2019, from http://library.ahima.org/doc?oid=300257#.XHuU6YhKiUl
- What is Malpractice? (n.d.). Retrieved from https://www.abpla.org/what-is-malpractice#medical
- Cady, R. F., Esq. (2009). Criminal Prosecution for Nursing Errors. JONA’s Healthcare Law, Ethics, and Regulation,11(1), 10-16. Retrieved March 1, 2019, from https://www.nursingcenter.com/cearticle?an=00128488-200901000-00003&Journal_ID=260876&Issue_ID=848807
- Kann, B. R., Beck, D. E., Margolin, D. A., Vargas, D., & Whitlow, C. B. (Eds.). (2018). Improving Outcomes in Colon & Rectal Surgery. Retrieved March 1, 2019, from https://www.books.google.com/books?id=O61vDwAAQBAJ&dq=
- Improving Outcomes in Colon & Rectal Surgery edited by Brian R. Kann, David E. Beck, David A. Margolin, H. David Vargas, Charles B. Whitlow&source=gbs_navlinks_s
- Peters, P. G. (2008). Twenty Years of Evidence on the Outcomes of Malpractice Claims. Clinical Orthopaedics and Related Research, 467(2), 352-357. doi:10.1007/s11999-008-0631-7
- Singh, H. (2018). National Practitioner Data Bank Generated Data Analysis Tool. Retrieved March 1, 2019, from https://www.npdb.hrsa.gov/analysistool/
- Top 5 Malpractice Claims Made Against Nursing Professionals. (n.d.). Retrieved March 1, 2019, from https://www.proliability.com/portals/0/docs/nursemalpracticewhitepaper.pdf
- American Nurses Association. (2010). ANA’s Principles for Nursing Documentation. Retrieved February 28, 2019, from https://www.nursingworld.org/~4af4f2/globalassets/docs/ana/ethics/principles-of-nursing-documentation.pdf
- Lippincott Nursing Education. (2018, February 22). Lippincott Nursing Education Blog. Retrieved March 1, 2019, from http://nursingeducation.lww.com/blog.entry.html/2018/02/22/nursing_documentatio-S5hF.html
- Reising, D. L., & Allen, P. N. (February 2007). Protecting yourself from malpractice claims. American Nurse Today,2(2). Retrieved March 1, 2019, from https://www.americannursetoday.com/protecting-yourself-from-malpractice-claims/.
- Reising, D. L. (2012). Make your nursing care malpractice-proof. American Nurse Today,7(1). Retrieved March 1, 2019, from https://www.americannursetoday.com/make-your-nursing-care-malpractice-proof/
End of Life Process
- No References
Alzheimer’s Nursing Care
- Alzheimer’s disease fact sheet. (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet
- Preventing Alzheimer’s disease: What do we know? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/preventing-alzheimers-disease-what-do-we-know
- How is Alzheimer’s disease treated? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/how-alzheimers-disease-treated
- Behavior changes and communication in Alzheimer’s. (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/topics/behavior-changes-and-communication-alzheimers
- How is Alzheimer’s disease diagnosed? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/how-alzheimers-disease-diagnosed
PTSD in Nursing
- Torres, F. (2020, August). What is Post-traumatic Stress Disorder. Retrieved February 17, 2021, from https://www.psychiatry.org/
- DSM-5 Diagnostic Criteria for PTSD Trauma-Informed Care in Behavioral Health Sciences NCBI. (n.d.). Retrieved February 17, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK207191/box/part_ch3box16/
- Posttraumatic Stress Disorder (PTSD): Patient Health Information. (n.d.). Retrieved February 17, 2021, from https://www.mayoclinic.org/diseases-conditions
- PTSD Examined: The five types of Post-traumatic Stress Disorders. (2020, August 26). Retrieved February 18, 2021, from https://bestdaypsych.com/ptsd-examined-the-five-types-of-post-traumatic-stress-disorder/
- What are the stages of PTSD. (2020, July 15). Retrieved February 18, 2021, from https://pyramidfbh.com/what-are-the-stages-of-ptsd/
- Mallvoire, B. L., Girard, T. A., Patel, R., & Monson, C. M. (2018). Functional connectivity of hippocampal sub regions in PTSD: Relations with symptoms. BMC Psychiatry, 18(129). https://doi:10.1186/s12888-018-1716-9
- Brewin, C. R., Gregory, J. D., Lipton, M., & Burgess, N. (2010). Intrusive images in psychological disorders: characteristics, neural mechanisms, and treatment implications. Psychological Review,117(1), 210-232. https://doi:10.1037/a0018113
- Posttraumatic stress disorder in doctors. (2005, February 26). Retrieved February 18, 2021, from https://www.bmj.com/330/7489/s86
- Mealer, M. Burnham, E. L., Goode, C. J., Rothbaum, B. & Moss, M. (2009). The prevalence and impact of posttraumatic stress disorder and burnout syndrome in nurses. Depression and Anxiety, 26(12), 1118-1126. https://doi.org/10.1002/da.20631
- Watkins, L. E., Sprang, K. R., & Rothbaum, B. O. (2018). Treating PTSD: A Review of Evidence-Based Psychotherapy Interventions. Frontiers in Behavioral Neuroscience, 12(258). Retrieved February 28, 2021, from https://www.frontiersin.org/article/10.338/fnbeh.2018.00258
- Medications for PTSD. (2017, July 31). Retrieved March 01, 2021, from https://www.apa.org/ptsd-guideline/treatment/medications
- Gore, T. A. (2018, November 14). Posttraumatic Stress Disorder Medication. Retrieved March 01, 2021, from https://emedicine.medscape.com/article/288154-medication#3
- Rosinta, U., & Robiana, M. (2019, February). The Effects of Progressive Muscle Relaxation in Reducing Fatigue among Nurses in Mental Hospital. Indian Journal of Public Health Research & Development, 10(2), 289-295. Retrieved March 2, 2021 from https://www.web.b.ebscohost.com/abstract?direct=true&profile=ehost&scope=site&authtype=crawler&jml=09760245&AN=13
- US Department of Veterans Affairs, V. (2014, January 15). Stress Inoculation Therapy (SIT). Retrieved March 02, 2021, from https://www.ptsd.va.gov/apps/decisionaid/resources/PTSDDecisionAidSIT.pdf
Nursing Ethics
- Gallup Poll finds nursing is most honest and ethical profession. (2021, January). Oakland University News,, . https://oakland.edu/oumagazine/news/nursing/2021/gallup-poll-finds-nursing-is-most-honest-ethical-profession
- Rushton, C. (2017, January). Why ethics?. John Hopkins Nursing. https://magazine.nursing.jhu.edu/2017/01/why-ethics/
- Fowler, M., “Nursing’s Code of Ethics, Social Ethics, and Social Policy,” Nurses at the Table: Nursing, Ethics, and Health Policy, special report, Hastings Center Report 46, no. 5 (2016): S9-S12. DOI: 10.1002/ h
- Florence Nightingale Pledge. (2010) https://nursing.vanderbilt.edu/news/florence-nightingale-pledge/#:~:text=I%20solemnly%20pledge%20myself%20before,knowingly%20administer%20any%20harmful%20drug
- Rich, K., & Betts, J. (). Ethical theories and approaches. Jones & Bartlett Learning.
- The ICN Code of Ethics for Nurses (2021). https://www.icn.ch/system/files/documents/2020-10/CoE_Version%20for%20Consultation_October%202020_EN.pdf
- Edmonton, C. & Zelonka, C. (2019). My own worse enemy: the nurse bullying epidemic. Nursing Administration Quarterly. July – September. 43(3). 274-279.
- Bell, J.A. ( 2013). Five generations in the nursing workforce. Journal for Nurses in Professional Development 29( 4 ) https://www.sgna.org/Portals/0/Bell_FiveGenerationsInTheNursingWorkforce_2013.pdf
- Should Euthanasia Or Physician Assisted Suicide Be Legal(2019). https://euthanasia.procon.org/
- Llamas, J. V. (2018, November). The moral and ethical dilemma of physician assisted suicide. Minority Nurse, (), . https://minoritynurse.com/the-moral-and-ethical-dilemma-of-physician-assisted-suicide/
- 11. Lockwood, W. (2020, April). Jurisprudence and nursing ethics. http://file:///D:/Ethics%20in%20Nursing/Jurisprudence.pdf
Ensuring Patient Confidentiality in Nursing
- American Nurses Association. (2015, June). American nurses association position statement on privacy and confidentiality. https://www.nursingworld.org/~4ad4a8/globalassets/docs/ana/position-statement-privacy-and-confidentiality.pdf
- Emergency Nurses Association. (2014). Sheehy’s manual of emergency care. In B. B. Hammond & P. G. Zimmermann (Eds.), Sheehy’s Manual of Emergency Care (7th ed., pp. 3–4). Elsevier Health Sciences.
- U.S. Department of Health & Human Services. (2015, November 6). Methods for De-identification of PHI. HHS.gov. https://www.hhs.gov/hipaa/for-professionals/privacy/special-topics/de-identification/index.html
- U.S. Department of Health & Human Services. (2013, July 26). Summary of the HIPAA Privacy Rule. HHS.gov. https://www.hhs.gov/hipaa/for-professionals/privacy/index.html
- U.S. Equal Employment Opportunity Commission. (2008). The Genetic Information Nondiscrimination Act of 2008 | U.S. Equal Employment Opportunity Commission. U.S. Equal Employment Opportunity Commission. https://www.eeoc.gov/statutes/genetic-information-nondiscrimination-act-2008
- Westrick, S. J. (2014). In Essentials of nursing law and ethics (2nd ed., pp. 77–84). Jones & Bartlett Learning.
A Nurse’s Guide: How to Deal with Difficult Patients
- Ratson, M. (2017, March 09). The value of ANGER: 16 reasons it’s good to get angry. Retrieved February 17, 2021, from https://www.goodtherapy.org/blog/value-of-anger-16-reasons-its-good-to-get-angry-0313175
- National Institute for the Clinical Application of Behavioral Medication. (2020, August 28). How anger affects the brain and body [infographic]. Retrieved February 18, 2021, from https://www.nicabm.com/how-anger-affects-the-brain-and-body-infographic/
- Okuda, M., Picazo, J., Olfson, M., Hasin, D., Liu, S., Bernardi, S., & Blanco, C. (2015, April). Prevalence and correlates of anger in the community: Results from a national survey. Retrieved February 19, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4384185/
- Brooker, C. (2017, July). Communication with angry patients through de-escalation. Retrieved February 18, 2021, from https://www.elsevierclinicalskills.co.uk/SampleSkill/tabid/112/sid/1727/Default.aspx
- Moyer, N. (2019, April 22). Amygdala hijack: What it is, why it happens and how to make it stop. Retrieved February 18, 2021, from https://www.healthline.com/health/stress/amygdala-hijack#overview
- Seladi-Schulman, J. (2018, March 21). Hypothalamus: Anatomy, function, diagram, conditions, health tips. Retrieved February 18, 2021, from https://www.healthline.com/human-body-maps/hypothalamus
- Seladi-Schulman, J. (2018, June 11). Pituitary gland overview. Retrieved February 18, 2021, from https://www.healthline.com/health/human-body-maps/pituitary-gland
- Awdish, R., & Berry, L. (2017, October 13). The importance of making time to really listen to your patients. Retrieved February 24, 2021, from https://www.physicianleaders.org/news/the-importance-of-making-time-to-really-listen-to-your-patients#:~:text=Actively%20listening%20conveys%20respect%20for,to%20truly%20listen%20to%20patients
- Price, O., & Baker, J. (2012). Key components of de-escalation techniques: A thematic synthesis. Retrieved February 25, 2021, from https://www.researchgate.net/profile/Owen-Price-2/publication/221837683_Key_components_of_de-escalation_techniques_A_thematic_synthesis/links/5a1e8b21458515a4c3d1faa0/Key-components-of-de-escalation-techniques-A-thematic-synthesis.pdf
*Patient names changed for anonymity.
How to Reduce New Nurse Turnover
- American Association of Colleges of Nursing. (2020, September). Nursing Shortage. Retrieved March 2021, from aacnnursing.org: https://www.aacnnursing.org/news-information/fact-sheets/nursing-shortage
- American Nurses Association. (2015, July 22). Practice & Advocacy. Retrieved from incivility, bullying and workplace violence: https://www.nursingworld.org/practice-policy/nursing-excellence/official-position-statements/id/incivility-bullying-and-workplace-violence/
- Boesch, M. B. (2017). Nurses Eat Their Young”: A Novel Bullying Educational Program for Student Nurses . Journal of Nursing Education and Practice, 11-21.
- Brewer, C. D. (2007). Newly licensed RNs characteristics, work attitudes, and intentions to work. American Journal Of Nursing, 58-70.
- Curtin, L. S. (2020, August). Nurse turnover: Understand it reduce it. American Nurse Journal, 57-59. Retrieved from MyAmericanNurse.com: https://www.myamericannurse.com/wp-content/uploads/2020/08/an8-Turnover-728.pdf
- HealthStream. (2017, October 11). To improve healthcare outcomes, we must focus on turnover. Retrieved from The Healthcare and Administration Blog: https://www.healthstream.com/resources/blog/blog/2017/10/11/to-improve-healthcare-quality-outcomes-we-must-focus-on-turnover
- Hohman, M. (2019, June 13). 4 compelling theories why nurses “eat their young.” Retrieved from florence-health.com: florence-health.com/career/nurse_practitioner/4-compelling-theories-as-to-why-nurses-eat-their-young/
- Kerfoot, K. (2013, September 21). New nurse turnover and patient safety: What’s the problem? Retrieved from Patient Safety & Quality Healthcare: https://www.psqh.com/news/new-nurse-turnover-and-patient-safety-whats-the-problem/
- Lockhart, L. (2020, March/April). Strategies to reduce nursing turnover. Retrieved from Nursing Made Incredibly Easy!: https://journals.lww.com/nursingmadeincrediblyeasy/fulltext/2020/03000/strategies_to_reduce_nursing_turnover.10.aspx
- Nursing Solutions, Inc. (2019). 2019 National health care retention & RN staffing report. NSI Nursing Solutions, Inc.
- Nursing Solutions, Inc. (2021). 2021 RN labor market update. NSI Nusrsing Solutions, Inc.
- Nursing Times. (2019, September 02). Nurses support their young: From competitors to mentors. Retrieved from Nursing Times-Workforce: https://www.nursingtimes.net/news/workforce/nurses-support-young-competitors-mentors-02-09-2019/
- Nursing Times. (2019, September 02). Nursing Times-Mentors. Retrieved March 2021, from Nursing Times: https://www.nursingtimes.net/roles/mentors/advertising-feature-avoid-nurse-burnout-02-09-2019/
- [email protected]. (2010, June 15). Seven strategies to avoid burnout. Retrieved from Healthleaders: https://www.healthleadersmedia.com/nursing/seven-strategies-reduce-nurse-burnout/
- Schmidt, K. (2017, August 23). How to recognize and prevent bullying in nursing. Retrieved from Nurse.com: https://www.nurse.com/blog/2017/08/23/how-to-recognize-and-prevent-bullying-in-nursing/
- u/martianteen. (2021, March). Bullying at work: nursing. . Retrieved from Reddit: https://www.reddit.com/r/nursing/comments/lxah2z/bullying_at_work/
- u/phol10. (2021, March). New nurse dealing with new onset of anxiety (r/nursing, 2021) nursing. Retrieved from Reddit: https://www.reddit.com/r/nursing/comments/lvugdi/new_nurse_dealing_with_new_onset_of_anxiety/
- u/schwee. (2021, March). Looking to leave bedside nursing; nursing. Retrieved from Reddit: https://www.reddit.com/r/nursing/comments/lyw80s/looking_to_leave_bedside_nursing/
- u/tjgirl. (2021, March). Post shift anxiety: nursing. Retrieved from Reddit: https://www.reddit.com/r/nursing/comments/lvtmwz/post_shift_anxiety/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate

