Course Content
Coronavirus: Everything Nurses Need to Know (Viewing Only)
Course Content (Viewing Only)
 Course: Coronavirus: Everything nurses need to know
Course: Coronavirus: Everything nurses need to know
Contact hours: 1.5
To earn continuing education credits for this course, enroll here.
Introduction
The outbreak of coronavirus and its slow spread into the United States has caused panic throughout the world. But did you know that the term “coronavirus” actually refers to more than just one type of virus?
As a healthcare provider, you should be sure to keep yourself informed with the latest news regarding this epidemic and prepare yourself for the possibility of encountering it in your workplace. Here’s everything you need to know about this group of viruses, the virus that’s currently affecting China and slowly spreading around the globe and how it’s diagnosed and treated.
What is a Coronavirus?
Coronaviruses are a group of viruses that have been known to cause moderate to severe respiratory symptoms that may mimic influenza. These symptoms include cough, runny nose, sore throat, body aches and pneumonia.
Coronaviruses have been affecting humans for several years, but there has not been an outbreak of epidemic proportions since the SARS epidemic of 2003. Coronaviruses are aptly named for the crown-like appearance the virus takes on when examined under a microscope (“corona” is Latin for “crown) (1). The 2019-nCoV is a respiratory virus, meaning it inhabits and attacks the lower and upper respiratory tract. This can cause symptoms ranging from a runny nose, cough or pneumonia.
Note the spikes or “crowns”, which give the virus it’s unique shape.
According to the Centers for Disease Control, there are seven different types of coronaviruses (1):
- 229E (alpha coronavirus)
- NL63 (alpha coronavirus)
- OC43 (beta coronavirus)
- HKU1 (beta coronavirus)
- MERS-CoV (the beta coronavirus that causes Middle East Respiratory Syndrome, or MERS)
- SARS-CoV (the beta coronavirus that causes severe acute respiratory syndrome, or SARS)
- 2019 Novel Coronavirus (2019-nCoV)
The most common types of coronaviruses that affect the human population are human coronaviruses 229E, NL63, OC43, and HKU1. However, there are instances where a coronavirus originates in animals and evolves into a virus that can affect humans.
The three most historically well-known types of these coronaviruses are the 2019 Novel Coronavirus (the most recent outbreak originating in Wuhan Province, China), Severe Acute Respiratory Syndrome (SARS), and Middle East Respiratory Syndrome (MERS).
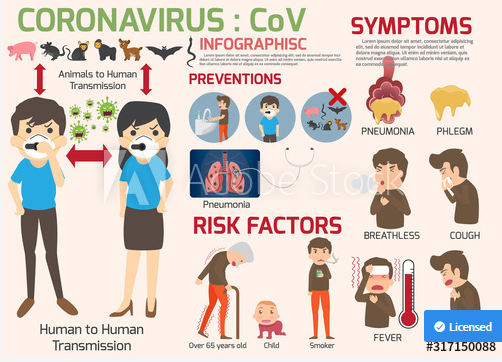
All of these types of coronavirus cause respiratory illness with symptoms that are very similar to upper respiratory infections and seasonal influenza (13). Symptoms can range from mild to severe. Below, you’ll find a breakdown of each:
2019 Novel Coronavirus (2019 nCoV OR COVID-19)

The coronavirus that has appeared in recent days is the 2019 Novel Coronavirus. This particular type of coronavirus was identified in Wuhan Province, China and has been shown to be the virus that has caused severe respiratory illnesses in several people. The virus is, at the time of this writing, spread to six continents and in dozens of countries.
It is thought that the virus may have originated in an outdoor market that sold snakes, other animals and seafood, as many of the victims of the virus reported being in that type of environment. Person-to-person viral transmission has been reported and is thought to be the primary route of spread, after the initial zoonotic transmission. The primary route of transmission is though to be droplet and/or airborne. This means infected persons can spread the virus by coughing / sneezing into the air.
Signs and Symptoms of 2019 Novel Coronavirus
The current outbreak of Novel Coronavirus has similar symptoms to MERS and SARS – fever, cough and shortness of breath. Similar to the other two types of coronavirus, severe cases may cause respiratory distress and failure, leading to mechanical ventilation and possible death. Again the 2019 nCoV is primarily a respiratory virus.
Those most at risk for complications and death include the elderly, those with weakened immune systems, and children (14). However, severe pneumonia and death have occurred in a small subset of young, healthy individuals.
Common signs and symptoms reported include:
- Cough
- Sneezing
- Runny nose
- Shortness of breath
- Fever
- Fatigue

What is the typical cause of death for those diagnosed with nCoV?
What are predominant symptoms of nCoV?
 What to Do if You Suspect Coronavirus
What to Do if You Suspect Coronavirus
According to the Centers for Disease Control guidelines, this is what you should do if you suspect your patient has coronavirus (8):
- IMMEDIATELY place a mask over the patient’s nose and mouth
- Place your patient on airborne and contact isolation (see below guidelines)
- Protect yourself by wearing a mask over your nose and mouth
- Practice good hand hygiene and implement universal precautions when coming into contact with a suspected patient
- Notify your hospital’s infection control department
- Notify local and state health departments
- Immediately notify the CDC’s Emergency Operations Center (EOC) at 770-488-7100 and complete a 2019-nCoV case investigation form
- Evaluate the patient for signs of pneumonia / ARDS and sepsis, with appropriate treatments.
Clinical monitoring and care of Coronavirus patients
Remember that the 2019-nCoV primarily affects the lungs. About 80% of cases are mild and may cause mild inflammation in the lungs, which may or may not be clinically relevant. However, in the other 20% of cases viral pneumonia and ARDS may develop. In many cases patients have been reportedly stable and then experienced rapid deterioration with sepsis and ARDS in less than 24 hours, leading to death.
For this reason, all patients diagnosed with 2019-nCoV should have all vitals signs, especially oxygen saturation checked. A decrease in oxygen saturation, adventitious lung sounds, or tachypnea (rales/crackles/rhonchi/wheezing) should be investigated with imaging. A plain chest Xray or CT chest without contrast should be ordered. Infiltrates may be noted and would indicate viral pneumonia is likely occurring.
If a patient develops viral pneumonia due to 2019-nCoV, strong consideration should be given to admitting the patient with continuous oxygen saturation monitoring at a minimum. If there are signs of sepsis (hypotension, tachycardia, tachypnea, high fever, signs of end of organ failure) appropriate measures should instituted- including fluid therapy.
According to early reports acute respiratory distress syndrome (ARDS) has developed rapidly in patients, including young healthy patients causing death in a short span of time. In ARDS, the alveoli of the lungs fill with fluid and inflammatory particles and respiratory failure may rapidly ensure, within a matter of minutes to hours. ARDS treatment is nuanced, but includes ventilatory support when needed and minimizing oxygen consumption (see our ARDS course).
The other aspects of care include supportive care. As 2019-nCoV causes sepsis and ARDS, the treatment is for those conditions and not specific to 2019-nCoV. The treatment for these conditions are complicated, and we have courses to cover both topics and help you understand these treatments.
Other key aspects of care include careful monitoring, and escalating care (transfer to ICU or higher level of care) with any signs of deteriorating. Pulmonary critical care specialists should be consulted early in the disease process and should likely lead the care team for these patients, as they are most experienced at treating both ARDS and sepsis.

Take-home points for treatment of patients with 2019-nCoV
- The virus affects the respiratory system and can lead to ARDS, which is the likely cause of death in 2019-nCoV patients. For this reason, pulmonary / critical care teams should be involved early in patients with confirmed or suspected pneumonia
- Patients with suspected or confirmed 2019-nCoV should be examined for signs of pneumonia, including adventitious lung sounds, tachypnea, excessive sputum production, or a decrease in oxygen saturation. If these are present, imaging should be obtained and appropriate clinical monitoring / treatments should be started. Note: imaging may not reveal infiltrates early in the disease process – this should not exclude a diagnosis of pneumonia.
- If ARDS develops patients should be admitted to the ICU and treatment initiated according to established ARDS guidelines. You can learn more about this in our ARDS course.
- If sepsis develops, standard sepsis treatment, including fluids, should be initiated early. Other key aspects of sepsis treatment include checking and trending lactic acid and drawing blood cultures. You can learn more about sepsis treatment in our sepsis course.
- Bacterial co-infections may be present with viral pneumonia. Strong consideration should be given to antibiotic therapy in 2019-nCoV patients with clinical pneumonia. In many viral ARDS cases, bacterial co-infections exist.
- Infectious disease consult should be obtained early, along with notification of proper state and federal (CDC) health officials.
- The mortality rate for 2019 nCoV appears to be around 2% currently, however, the mortality rate of those who develop clinically apparent pneumonia is much higher and should be treated a such.
- Currently, there is no anti-viral medication to treat coronavirus and there is no vaccine to prevent it. The National Institute of Health (NIH) is in the preliminary stages of developing a vaccine against coronavirus, but there is no word regarding when that vaccine will be released (13). However, in cases of pneumonia where bacterial co-infection cannot be ruled out, antibiotic therapy may be prudent, depending on the patient.

What testing / examinations should be done to evaluate for viral pneumonia?
If pneumonia is diagnosed or suspected, what treatments and monitoring should begin?
What are some signs that coronavirus patients are developing sepsis?
Diagnosis of Coronavirus
The diagnosis of the SARS and MERS types of coronavirus is made by laboratory polymerase chain reaction (PCR) testing, through the examination of both respiratory specimens (including nasopharyngeal or oropharyngeal aspirates or washes, nasopharyngeal or oropharyngeal swabs, broncheoalveolar lavage, tracheal aspirates, and sputum), as well as blood testing. For the 2019 novel coronavirus, diagnostic testing is only available at the Centers for Disease Control at the time of this writing (11). However, there are plans by the CDC to make the test available at select facilities in the near future.
Transmission of Coronavirus
According to a World Health Organization situation report, the incubation time for 2019 novel coronavirus is estimated to be between 2-10 days. It is not yet known if the virus can be spread during the incubation period, including when a patient is asymptomatic (12). Symptoms may appear as little as two days after initial exposure and as many as 14 days after initial exposure.
The transmission of coronavirus has been linked to animal-human transmission. The SARS and MERS types of the virus are thought to have originated in bats. In SARS cases, bats transmitted the virus to civet cats, which then transmitted the virus to humans. In MERS cases, bats were thought to have transmitted the virus to camels, which then transmitted the virus to humans.
Human-to-human transmission in all types seems to occur when humans that are carrying the virus are in close contact with other people. That may include those that are caring for a sick relative, those that are traveling in close quarters with an infected person, or those that have intimate contact with an infected person (8).
Questions to Ask Your Patient
One of the most important things to consider in the evaluation of a possible coronavirus patient is their medical and travel history. Here are some questions you should be asking your patients:
- Have you traveled out of the country within the last 21 days?
- If so, where have you traveled?
- Has anyone in your household been sick recently?
- Have you had any sick contacts in the last 21 days?
- Are you feeling ill today?
- When did your symptoms start?
- What are your symptoms?
- What is the highest your fever has been?

What questions should you be asking patients that you suspect may have coronavirus?
What precautions should you immediately take if you suspect coronavirus?
Prevention for Healthcare Providers
As a healthcare provider, there are several things you can do to prevent the spread of coronavirus and prevent it from affecting you. One of the most important things you can do now is review the concept of isolation precautions and the different forms that exist. Isolation guidelines exist under the assumption that all bodily fluids contain “transmissible infectious agents” (9).
Patients suspected of having coronavirus should immediately place a mask over their nose and mouth. Healthcare providers should quickly place the patient under contact and airborne isolation, as well as initiating standard precautions (13).
Here’s a breakdown of each one, according to the CDC (9):
Standard Precautions: Standard precautions should be used when coming into contact with any patient, regardless of possible or actual diagnoses. Standard precautions include:
- Proper hand hygiene (this means washing your hands with soap and water or using an alcohol-based hand sanitizer after every patient contact)
- Use of mask or face shield if necessary
- Eye protection if needed
- Safe injection practices
- Use of gloves
- Cleaning all equipment that has been in contact with a patient with an approved disinfecting wipe
Contact Isolation: Contact isolation guidelines exist to protect healthcare workers from being exposed to infectious, multi-drug resistant organisms that may be present in wounds, bodily fluids, or other sites. The guidelines are also in place to prevent the spread of those microorganisms to other patients in healthcare settings via care providers. that warrant contact isolation include but are not limited to:
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Vancomycin-resistant enterococcus (VRE)
- Carbapenem-resistant Enterobacteriaceae
- 2019 novel Coronavirus
Healthcare personnel caring for a patient on contact isolation should don a gown and gloves when performing patient care. Gown and gloves should be doffed prior to exiting the room after completing patient care, and hand hygiene should immediately be performed.
Airborne Isolation: Airborne isolation precautions are put in place to prevent the transmission of infection via respiratory particles that are able to survive and travel long distances through the air.
Under airborne isolation precautions, healthcare providers must don a mask or N95 respirator, depending on the type of infection present. An N95 respirator is a special face mask that filters 95% of very small particles out of the air breathed in by the person wearing it. The patient must be placed in a negative-pressure and must be the only patient in the room.
If no negative pressure room is available, the patient must be placed in a private room and must don a face mask over their nose and mouth. Immunocompromised or those who do not have immunity to rubeola, varicella, or other communicable diseases for which there exist vaccines are not advised to care for these patients if at all possible.
*IMPORTANT: In order to ensure a properly fitted N95 respirator in airborne isolation precautions, healthcare providers must attend an approved education course and be fitted for a respirator by fit testing and seal checks. This will ensure that no errant particles are able to get through the respirator.

Name the three main types of isolation precautions.
What isolation precautions are required to be implemented for patients suspected of having coronavirus?
Prevention in the Community
There are several things nurses can teach patients in order to prevent the spread of coronavirus in the community. The virus can be spread through droplets in the air and can survive up to three to six feet before dying (13). Coronavirus can also live on surfaces. With these things in mind, be sure to counsel your patients to do the following:
- Wear a mask that covers your nose and mouth when around others while you are experiencing symptoms.
- Practice good hand hygiene – this means washing your hands with hot, soapy water for one minute. Be sure to wash your hands after touching your face or any secretions that may come from your nose and mouth. Utilize an alcohol-based hand sanitizer frequently, unless your hands are visibly soiled.
- Sanitize surfaces in your home that other people may come into contact with.
- If you are caring for someone who has been diagnosed with coronavirus, avoid close contact with that person. If you must come into close contact with them, wear a mask over your nose and mouth. Be sure to wash your hands after every encounter. Use separate dishes and eating utensils than the infected person.
- Patients with clinically stable coronavirus should be quarantined. The choice of self-quarantine VS mandatory is a choice that must be made on an individual basis.
Key Points to Remember
- Symptoms of coronavirus are related to the respiratory tract. Pneumonia is possible and may lead to respiratory failure and even death.
- Coronavirus is thought to have originated in bats, which then transmitted the virus to animals (cats, camels, snakes). However, this has not been confirmed.
- The incubation period for coronavirus is estimated to be 2-14 days. Patients may be contagious during this incubation period.
- Some patients with coronavirus may not exhibit any symptoms. Symptom severity can range from mild to severe/ life-threatening.
- Treatment of coronavirus is supportive. There is no known treatment for this virus itself. Patients should be evaluated for pneumonia / ARDS and sepsis, with appropriate treatments .
- There is no vaccine for coronavirus.
- There is no effective, tested antiviral for the coronavirus.
- Patients suspected of having coronavirus should immediately be placed under airborne and contact isolation. Standard precautions should be initiated.
- If you suspect your patient has coronavirus, immediately notify the hospital infection control department, local and state health departments, and the Centers for Disease Control Emergency Operations Command.
- Testing for coronavirus is currently only available through the CDC currently. Key centers will likely receive testing kits within the near future.
- Patients with 2019 nCoV may be clinically stable initially with a rapid decline. For this reason, careful monitoring is key to preventing mortality.
Conclusion
Although coronavirus has been affecting humans for many years, there are still new forms evolving today. As healthcare providers, you have a responsibility to understand the virus and its effects on the population.
Remember, guidelines and recommendations can change at the drop of a hat, so be sure to continue to check in with local, state and national health organizations for any changes. You are part of the line of defense to prevent the spread of this deadly virus, so be sure to stay informed.

