Course
Differentiating Cognitive Aging and Dementia
Course Highlights
- In this course we will learn about the differences between cognitive aging and dementia, and why it is important for nurses to be able to recognize both.
- You’ll also learn the basics of neurological determinants noted in those with dementia, as well as treatments and nursing interventions.
- You’ll leave this course with a broader understanding of how to differentiate between normal cognitive aging and dementia in patients.
About
Contact Hours Awarded: 1.5
Course By:
Amy Lynn White
CNO, MSN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Often, individuals, family members, and healthcare workers fail to understand the relationship of neurological symptoms related to dementia. It can be rather difficult to differentiate normal cognitive aging and age-related memory loss versus early signs of dementia, which may need further diagnosis and treatment. Many of us tend to become more forgetful as we age and may need a bit longer to remember things, become distracted more easily, or have issues with multi-tasking. Even though these changes are normal and typically occur during middle age, they can very well become a nuisance and even frustrating at times. But how can one know that these are normal and are not an early symptom and determinant of dementia? For most individuals, these changes are a normal result of cognitive aging, but it is important to understand the differences so diagnosis can be accurate and efficient in treating these individuals who are dealing with dementia.
With an increasing number of age-related illnesses, it is sometimes difficult to differentiate dementia and normal age-related memory loss and verify the proper treatment for family members and nurses caring for this population. However, the differences must be made clear so proper understanding, treatment options, and medical interventions can be made accurately for this special population to receive the care they truly need and deserve.
Justification of Knowledge
With the ever-increasing numbers of diagnosed dementia cases, it is important to understand the neurodegenerative processes that involve damage to the brain, which can lead to progressive, incapacitating behavioral, cognitive, and motor dysfunctions that typically end with dementia. In individuals that have fully manifested dementia, there are typically neurological signs that precede the full onset of dementia and recognizing these distinctions can often be a challenge (7).
Since both dementia and age-related memory loss have similarities, making clear distinctions can often be a challenge. Caregivers often think that his/her loved one may be suffering from dementia when it may be normal age-related memory loss and vice versa.
The syndrome of dementia is typically characterized by progressive deterioration of various cognitive functions. Some of the major neurological symptoms noted are agitation, apathy, depression, delusions, hallucinations, anxiety, irritability, euphoria, and sleep disturbance (6).
The normal age-related memory loss may be related to the hippocampus, an area of the brain involved in the formation and retrieval of memories, certain hormones and proteins that repair and protect brain cells decrease with age, and older individuals typically experience decreased blood flow to the brain, which can affect one’s memory (6).
The Alzheimer’s Society of Canada noted that about 40 percent of people aged 65 and above would experience some form of “memory loss” without any underlying health causes. It’s simply a part of normal cognitive aging, but there are noticeable differences when dealing with a form of dementia (1). The differences noted are as follows:
- Inability to perform routine tasks
- Difficulty recalling the right words
- Forgetting the names of family members
- Misplacing objects
- Experiencing moods that do not match the situation
- Issues with balance
Inability to perform routine tasks – the individual may forget how to drive to a location they go to regularly, or he/she may have difficulty managing his/her budget.
Difficulty recalling the right words – the individual may have to pause to consider how to express what he/she wants to say and typically has more difficulty with verbal communication. The individual may also start calling familiar objects by the wrong name.
Forgetting the names of family members – the individual may misplace the names of family members and those that are seen daily.
Misplacing objects – the individual may lose an object such as car keys or glasses and not be able to find it later because he/she does not identify as his/her own. An example of this is that a person with normal “memory loss” will actively search for an object that has been misplaced, while a person with Alzheimer’s may not remember he/she needs glasses at all.
Experiencing moods that do not match the situation – the individual will have unexpected mood swings that do not match the current circumstance. It is important to keep in mind that certain medications have side effects that can affect mental function, so it is important to seek guidance from the individual’s primary care physician to rule out any side effects.
Issues with balance – the risk of falling increases as dementia progresses, and elderly individuals are eight or nine times more likely to fall than older people who have not been diagnosed with a form of dementia. Fine motor skills also seem to progress as the disease worsens.
We should be investing our efforts in observing and reporting any potential signs of underlying dementia. Early diagnosis of dementia leads to more effective treatment options and advanced decision-making for interventions needed. Accurate diagnosis of dementia is the ultimate key to proper treatment, and both health care providers and caregivers need to provide empathy in caring for these individuals. As part of reaching these goals, it will be necessary for all those caring for individuals with dementia to become more knowledgeable about dementia, proper care aspects, and the most effective approaches that need to be used with this vulnerable population. In doing so, these practices will provide both the support and care needed to successfully care for those with dementia.

Self Quiz
Ask yourself...
- As a health care provider or caregiver, what can we do to assist these individuals with dementia to receive the proper care and treatment they each deserve and need?
- What are some of the key differences between normal cognitive aging and dementia?
- Why do you think it is so important to differentiate dementia from normal cognitive aging?
What is Dementia versus Cognitive Aging Memory Loss?
At one point or another in our lives, we have misplaced a set of keys, totally blanked on remembering someone’s name, forgot a phone number, or walked into a room to do or get something and forgot and then began wondering what you went in there for. Even though memory lapses can be frustrating, most likely, they are not cause for concern. These normal, cognitive aging memory changes are not the same issue as dementia.
As one grows older, there are various physiological changes that can cause variations in brain functions that one typically doesn’t even think about. A few examples of these are the process of the longer duration to both learn and to recall information, one is not as quick as he/she used to be, and it can sometimes take longer to recall events to mind. Cognitive aging memory lapses typically have little impact on one’s daily activities and one’s ability to do what he/she wants to do.
Dementia is marked by a persistent and often disabling decline in two or more intellectual abilities such a memory, judgment, language, and abstract thinking. The chart below compares normal cognitive aging changes to those that may indicate dementia (6):
Cognitive Aging Memory Changes | Symptoms That May Indicate Dementia |
| Ability to function independently and pursue normal activities of daily living | Difficulty conducting simple tasks (paying bills, dressing appropriately, self-grooming, etc.) and forgetting how to do things that one has done many times |
| Ability to recall and describe periods of forgetfulness | Unable to recall or describe specific situations where memory loss was present |
| May hesitate or pause to remember directions, but does not get lost in places that are familiar | Gets lost or disoriented in familiar places and unable to follow directions |
| Occasional problems finding the right words, but no problem holding a conversation | Words are often forgotten, garbled, misused, and misunderstood. Phrases and stories are repeated several times within the same conversation |
| Judgment and decision-making ability are the same | Difficulty making choices. Poor judgment or behavior may be conducted socially inappropriately |
In addition to normal, cognitive aging, there are other conditions that mimic dementia, and these can be caused by medications, minor head trauma or injury, emotional disorders, alcoholism, vitamin B-12 deficiency, hypothyroidism, and brain disease. Once these symptoms are noted, it is imperative that the individual undergoes an examination by his/her primary care physician to determine if further testing needs to be done in order to assess the degree of memory impairment and accurate diagnosis.
One may ask if other conditions can cause memory loss. The answer is “yes,” and it is important to remember that everyone is different and may be exhibiting similar symptoms from another medical condition.
Common Types of Dementia
Alzheimer’s Disease
Studies have shown that 60-80% of people with dementia have Alzheimer’s. The individual presents with symptoms such as memory loss and difficulty planning and performing routine tasks. The symptoms are mild at first but progressively worsen. Other symptoms noted may be confusion about person, place, time, difficulty speaking and/or writing, losing things and inability to find them, showing poor judgment, and mood and personality changes (2).
Vascular Dementia
Individuals with this type of dementia typically have had a stroke, and symptoms depend on which part of the brain is affected by the stroke. The first signs noted with vascular dementia is typically poor judgment or difficulty planning, organizing, and making decisions. Other noted symptoms are memory problems that disrupt the individual’s daily life, difficulty speaking and understanding speech, difficulty recognizing sights and sounds that used to be familiar, becoming confused or agitated easily, changes noted in mood and personality, and difficulty walking and having increased falls (2).
Dementia with Lewy Bodies (DLB)
Lewy bodies consist of tiny, microscopic deposits of a protein that form in some individual’s brains. The name is traced back to the scientist who discovered them. The deposits of the protein develop and form in the part of the brain called the cortex, and the symptoms include difficulty thinking clearly, making decisions, or paying attention. The individual also has problems with memory, experiencing hallucinations, unusual sleepiness during the day, periods of “blanking out” or staring, difficulty with movement including slowness, and trouble walking, and the individual may have dreams where he/she acts out physically and may include walking, talking, and kicking (2).
Parkinson’s Disease Dementia
Studies have shown that individuals with nervous system disorders experience this type of dementia an estimated 50-80% of the time. Typically, the symptoms of dementia develop approximately ten years after a person is first diagnosed with Parkinson’s. Individuals with Parkinson’s Disease have the same symptoms as DLB and both conditions exemplify signs of Lewy bodies in his/her brains (2).
Frontotemporal Dementia (FTD)
Individuals with this type of dementia have developed cell damage in areas of the brain that control judgment, planning, emotions, movement, and speech. These individuals may also experience behavior and personality changes, sudden lack of inhibition in social and personal situations, problems thinking of the correct words when speaking, and movement problems such as shakiness, muscle spasms, and balance problems (2).
Huntington’s Disease
This disease is caused by a genetic defect that is typically passed from one family member to another. The individual may have the gene for this disease at birth, but typically the symptoms do not usually start until the ages of 30-50. The individual typically has difficulty with thinking and reasoning, memory, judgment, organizing, planning, and concentrating (2).
Creutzfeldt-Jakob Disease
In this type of dementia, a protein called prions cause normal proteins in the brain to begin developing into abnormal shapes. This disease is a rare condition that leads to dementia symptoms that occur suddenly and quickly become worse. The individual may experience memory and concentration problems, poor judgment, mood swings, confusion, sleep problems, depression, trouble walking, and twitching or jerking muscles (2).
Normal Pressure Hydrocephalus
A buildup of fluid in the brain is noted in this type of dementia and includes difficulty walking, concentrating personality, and behavior changes. In some cases, the extra fluid can be drained from the brain into the abdomen through a long, thin tube called a shunt (2).
Wernicke-Korsakoff Syndrome
A severe shortage of thiamin (vitamin B-1) is noted in this type of dementia and is noted most in individuals who are long-term heavy drinkers. The most common symptom noted is problems with memory, but typically one’s problem-solving, and thinking skills are not affected (2).
Neurological Determinants Noted in Individuals with Dementia
In a study conducted by a Dementia Research Group, information was collected regarding neurological symptoms using a NEUROEX assessment based on surveys of older adults living in low and middle-income countries. The data collected involved 10,856 adults participating in the baseline assessment. Exploratory and confirmatory analyses were used to explore the neurological symptoms.
The results indicated that there were four dimensions of neurological signs, which are associated with lesions related to specific regions of the brain. The results showed that neurological symptoms were consistent with the areas of the frontal, cerebellar, extrapyramidal, and more generalized disturbances of gait were noted. The pout reflex symptom is a common symptom seen in the frontal lobe and is associated with vascular dementia. Difficulties in fine finger movements are typically impairments related to cerebellar dysfunction. Tremor and rigidity are typically seen as extrapyramidal deficits that are related to Parkinson’s Disease. Gait ataxia which is a result of dysfunction of the frontal area of the brain was also noted and may include mixed types of symptoms with other symptoms of a non-neurological nature such as arthritis, respiratory, and vascular issues (7).
Due to certain other conditions that mimic dementia, many times normal, cognitive aging memory loss can be mistaken as a form of dementia. Also, certain medical conditions and vitamin deficiencies such as hypothyroidism, hydrocephalus, Vitamin B12 deficiency, infections, and certain prescription and over-the-counter medications can cause dementia-like symptoms well. It is imperative that a proper assessment is completed by an individual’s primary care physician or referral to a neurologist to rule out any underlying causes for these symptoms that may not be true dementia.

Self Quiz
Ask yourself...
- What is the likelihood that individuals are misdiagnosed with dementia when in reality, it may be normal cognitive aging and age-related memory loss?
Treatment and Interventions for Nurses and Caregivers
Pharmacological Interventions
Even though there is no cure for dementia or any disease-modifying agents that can fully combat Alzheimer’s disease and the related dementia, there are some medications that can assist with slowing down the progression of cognitive loss. These medications are classified as anti-dementia drugs and can only be prescribed by a medical doctor. Medications prescribed are given based on the type of dementia characterized by the individual. It is important to note that the individual may experience side effects as with any medication and the medications used for dementia are typically expensive (5).
Non-Pharmacological Interventions
There are various therapies used to support those diagnosed with dementia, and to aid is assisting the nurses and/or family caregivers who are caring for these individuals. Not all therapies work for each individual experiencing dementia, and it is important to work together as a team with both medical providers and family members to provide and offer the best-individualized solution. The types of non-pharmacological interventions are as follows (5):
Cognitive Stimulation Therapy (CST)
Cognitive Stimulation Therapy is used for those individuals with mild to moderate dementia, and the individual is invited to partake in therapeutic sessions with a trained practitioner that specializes in skills related specifically to individuals with dementia. A session consists of themed activities that are designed to stimulate and engage the individual with dementia. Some of the themes used may include topics such as money, current affairs, food, and clothing. The sessions are typically held twice a week, beginning with 14 sessions followed by 24 maintenance sessions. The key aspects focused on are person-centeredness, involvement, respect, inclusion, fun, choices, the use of reminiscence, and strengthening relationships (5).
Reminiscence Therapy
Reminiscence therapy allows a person with dementia to tap into his/her long-term memory and experience memories that were pleasurable. With this type of therapy, it has been considered one of the most popular and can be enjoyed by the individual with dementia, health service professionals, and relatives. The therapy can be completed in several formats using life story work, simple or general reminiscence, and specific or special reminiscence (5).
Validation Therapy
Validation therapy attempts to use a practitioner to communicate with the person with dementia by showing empathy with his or her feelings, and special meaning is displayed behind the person’s speech and behavior assisting the individual. Validation therapy aims to validate the individual’s emotions by acknowledging one’s feelings and the aim to make the person with dementia as happy as possible, even though there may be misconceptions and misinterpretations. It is important to keep in mind that if a demented individual is experiencing delusions or false beliefs which can cause added distress, validation therapy is not the best source of therapy (5).
Reality Orientation
This type of therapy helps the individual with dementia by reminding him/her about the present. Self-identity is reinforced, and recognition of one’s surrounding environment is also emphasized. The different forms used with reality orientation are calendars, reminder boards, and cueing and typically take place in groups or individually. It is important to be mindful of the fact that the individual may have difficulty remembering current or recent events due to his/her cognitive impairment (5).
Physical Exercise
The act of exercising has been shown to benefit people with and without cognitive impairment and has been found to be extremely beneficial to those who once led a very active life. It is important to encourage individuals with dementia to participate in some form of physical activity and to make adaptations as needed once dementia progresses. In formulation exercise programs for these individuals, attention should be given to the individual’s abilities, preferences, interests, and safety needs. Physical activity has also been recognized for its effects on reducing depressive symptoms and behavioral disturbances such as aggression and agitation (5).
Multisensory Stimulation: Snoezelen Rooms
Multisensory stimulation is increasingly being used in long-term residential care settings to help individuals with dementia who may be agitated or restless. A Snoezelen room incorporates multiple sources of stimulation such as light, watercolor, fiber optics, contrasting textures, quiet music, and soft furnishings. All these features are meant to help relax the individual with dementia and can also enhance communication between the individual and his/her caregiver (5).
Aromatherapy
Aromatherapy is often used with individuals with dementia, and the use of smells, massage, and bathing can stimulate pleasurable emotions for the individual with dementia. Two of the most used essential oils are lavender and a special type of balm. Aromatherapy has proven in many trials to produce a decrease in agitation among these individuals with dementia (5).
Health systems are working to improve in this area and to recognize the burden that is presented upon caregivers caring for those with dementia. There is a gap between the need for treatment, the active provisions for treatment, and educating families regarding the options that are available for treatment. Many families seem to feel the burden is too great to care for his/her loved one with dementia independently. Due to this reason, it is imperative that both physical and emotional support be offered. Many times, families are not aware of the resources available for this population of individuals, and they need assistance and education to evaluate the available options. All these factors should encourage the importance of increased support, health, and awareness among this vulnerable population.
Are we doing a sufficient job at ensuring that the population of individuals with dementia and their caregivers are receiving the proper health and support they need?
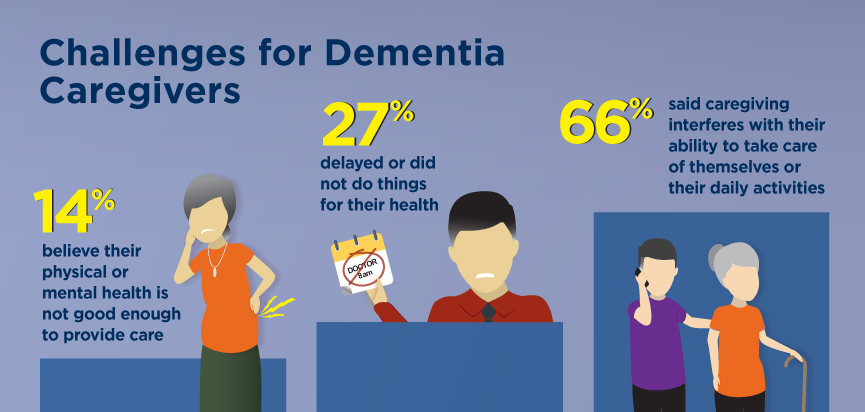
The following are some challenges that were reported among caregivers, and it is important to keep these in mind when formulating the best treatment plan for the individual with dementia (8):
Since it can be challenging to correctly diagnose and treat those individuals with dementia symptoms and other disorders, how can one determine the best assessment tool to use?
There is not one single tool that is recognized as the best overall assessment tool to determine if a full dementia evaluation is needed. There are several different ones, but the two that seem to be used consistently are the GPCOG, a screening tool for cognitive impairment designed to be used in primary care settings. And the Mini-Cog is an assessment tool that consists of a three-minute recall test assessing memory and a scored-clock drawing test. The results are evaluated by a healthcare provider, who then determines if a full-diagnostic assessment is needed (5).
It is necessary to assess individuals with dementia for anger and aggressiveness that can stem from overstimulation or boredom. Feelings of being overwhelmed, bored, or lonely can all trigger anger or aggression. Also, once one factor into the scenario that the individual is experiencing confusion, one realizes that the individual is more than likely not even fully aware of what he/she is doing and his/her actions. The greatest concern during an episode such as this is to maintain the individual’s safety and the safety of others. If the individual is approachable, it is important to talk calmly and in a non-judgmental way to the individual during a period such as this to allow him/her to de-escalate and hopefully turn from being so angry and aggressive. During episodes such as these, it is also important to allow others to assist and help if they are present and available. It sometimes takes two or three individuals to calm someone in this state of mind due to dementia.
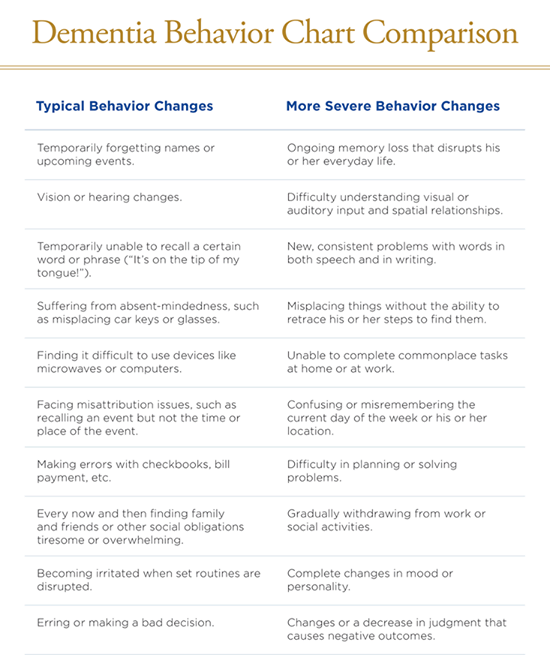
The greatest barriers include reluctance to seek help, fear of loss of independence, or concerns about how others will perceive dementia. Other barriers include the lack of skills to recognize the possible signs and symptoms of dementia, as it can sometimes be difficult to differentiate from normal cognitive aging. Dementia is a diagnosis that requires precise and detailed assessments over several consultations that typically span over several months. In an effort to assist health care members, family members, and caregivers caring for those with dementia, a chart has been created for use that demonstrates typical behavior changes noted with dementia to more severe behavior changes (8).
Working with someone with characteristics of dementia and normal cognitive aging and age-related memory loss can be challenging, and it is important to be able to clearly distinguish between the two in order to obtain the needed and crucial treatments necessary if needed.
Assessment is a crucial factor in determining if dementia is present or if the signs and symptoms are an indicator of normal cognitive aging and age-related memory loss. Assessment is also the first identification to obtain the needed treatment for the individual and to offer services and support to the family members or caregivers.
Individuals with dementia may feel that they are no longer in control and may not trust their judgment. They may also experience the effects of stigmas and social isolation, such as not being treated the same by certain people due to their diagnosis. All these issues can have a negative impact on the individual’s self-esteem.

Self Quiz
Ask yourself...
What are the main concerns noted among an individual with dementia that becomes angry and aggressive?
Many people voice that obtaining the proper treatment in a timely manner is an incredible challenge among those with dementia. What are the major barriers to a timely diagnosis of dementia?
What effect can negative attitudes have on an individual with dementia?
Moving Forward: The Future of Individuals with Dementia
With increased awareness among this vulnerable population and the number of individuals diagnosed with dementia, the future for those caring for these individuals proves that advanced care and education needs which have been a recent focal point, have proven successful. The information below details some highlights for the future that is seemingly optimistic (4):
- Recent study from 1988 – 2015 has shown a 13 percent decreased per decade in the incidence of dementia in the United States and Europe.
- If trends continue, there could be 15 million fewer people living with dementia in high-income countries by 2040.
- Change is likely linked to increased health education along with a better understanding of modifiable risk factors, such as diet and exercise.
- Experts stress the need for doctors, health care members, individuals, family members, and caregivers to develop healthy habits to lower one’s risk for developing dementia.
Both small and large actions can be taken as a client care health advocate for positive results to be obtained. First, volunteer or assist in a facility that offers services to these individuals, educate yourself and your immediate circle on the facts surrounding dementia, serve as a mentor, and receive the necessary education and training to pursue legislative advocacy. Throughout the entire process of advocacy, these elements need to remain – confidentiality, purpose, equality, diversity, empowerment and most importantly, treating the individual with dementia with empathy, compassion, and respect.
The care and treatment for those with dementia and the ones caring for these individuals certainly can improve if healthcare workers, family members, and caregivers are all trained and educated on the symptoms, treatment options, and available resources to assist those caring for these individuals.
Education is the ongoing key to becoming more aware of proper care and treatment options for individuals with dementia. Increased knowledge and expertise in this area and serving as an advocate for these individuals by listening and representing the individual’s views must be in place for this population to receive the necessary and adequate care they each deserve. Questions can be asked on the individual’s behalf in order to ascertain that necessary treatment options and support services are being offered. It is also imperative to use a holistic approach with both the individual with dementia and the health care member(s), caregiver(s), and family members to maintain open communication, empathy, and compassion while developing the best plan of action for the individual.
References + Disclaimer
- Published on January 17. (2020, September 16). Normal Aging vs. Alzheimer’s: Key Differences – Page 2 of 6. ActiveBeat. https://www.activebeat.com/your-health/normal-aging-vs-alzheimers-6-key-differences/2/.
- Casarella, J. (2020, September 29). Types of Dementia Explained. WebMD. https://www.webmd.com/alzheimers/guide/alzheimers-dementia.
- Dementia Care Case Study. Helping Hands Home Care. (2020, August 12). https://www.helpinghandshomecare.co.uk/home-care-services/dementia-care/dementia-care-case-study/.
- Gray, D. (2020, August 12). Why Dementia Risk Is Declining and What That Means for the Future. Healthline. https://www.healthline.com/health-news/why-dementia-risk-is-declining-and-what-that-means-for-the-future.
- Interventions Pharmacological and Non-Pharmacological. Dementia Services Information and Development Centre. (n.d.). https://dementia.ie/.
- Melinda. (2021, April 19). Age-Related Memory Loss. HelpGuide.org. https://www.helpguide.org/articles/alzheimers-dementia-aging/age-related-memory-loss.htm.
- Pasquini, L., Llibre Guerra, J., Prince, M., Chua, K.-C., & Prina, A. M. (2018). Neurological signs as early determinants of dementia and predictors of mortality among older adults in Latin America: a 10/66 study using the NEUROEX assessment. BMC Neurology, 18(1). https://doi.org/10.1186/s12883-018-1167-4
- Welcome to Five Star Senior Living. (n.d.). https://lp.fivestarseniorliving.com/.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate

