Course
A-Fib and Stroke Risk
Course Highlights
- In this course we will learn about A-Fib and Stroke Risk.
- You’ll also learn about the CHADs Stroke Risk Scoring System.
- You’ll leave this course with a broader understanding of how oral anticoagulants are used to reduce stroke risk in patients with A-FIb.
About
Contact Hours Awarded: 1.5
Course By:
Joanne Kuplicki
MA, RN, ccrn, Nc-bc
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
“Stroke remains the 5th leading cause of death and disability in the United States” (1), and yet there are many times where clinicians struggle to find the exact cause. The diagnosis of stroke is often finalized only after a risk factor analysis and diagnostic images that are done post event. A-fib and stroke are increasing in frequency in our population due to longevity and other risk factors. A-fib and stroke should be investigated thoroughly in order to prevent future events and assist patients and families in self-management and stroke prevention. Nursing staff play a crucial role in educating patients regarding risk factors for prevention and signs/symptoms of A-fib and stroke. Recent development of many new oral anticoagulants demands that the bedside nurse knows which are appropriate for A-fib and stroke risk reduction.
Pathophysiology of A-Fib and Stroke
Strokes occur when the blood vessels to the brain either rupture or are blocked by a clot. These incidents reduce the blood flow to the brain, which carries essential elements like oxygen and nutrients for cell survival.
Ischemic strokes caused by a clot or emboli are the more common cause of stroke and occur in approximately 87% of cases. Strokes that originate from cardiac factors are known as “cardio-embolic.“ Atrial fibrillation (A-fib) is one of the major cardiac causes responsible for cardioembolic strokes. In atrial fibrillation, blood can pool in the upper chamber atriums due to the chaotic rhythm.
“Cardioembolic stroke accounts for 14-30% of all ischemic strokes and atrial fibrillation is the most common cause” (2). The risk of A-fib and stroke increases with age, and it has been noted that strokes from atrial fibrillation tend to be more severe. Other causes of cardioembolic stroke include myocardial infarction, mechanical cardiac valve placement, and dilated cardiomyopathy.
In general, the risk factors of cardioembolic stroke overlap with the general risk factors for stroke and include hypertension, diabetes mellitus, hyperlipidemia, cardiac diseases, and lifestyle factors, not just atrial fibrillation. A cardioembolic stroke occurs when blood clots or emboli travel from the heart or aorta and lodge in the cerebral circulation, causing ischemia.
The clot or emboli that is formed can also be made of bacteria or fat, and when this travels to the cerebral vessels, the consequence can be devastating. The course of illness depends on the severity of the stroke, pre-existing conditions, age, and any complications presented. Stroke can be a rapid onset medical emergency. Most hospitals require patient education regarding stroke signs, symptoms, and management, such as when to call for EMS in a timely manner.

Self Quiz
Ask yourself...
- Have you ever had a patient/client who had difficulties maintaining anticoagulation regimens and lab follow–up? Did they ever present with clotting disorders such as DVT, PE, or Stroke?
- TEE and/or Echocardiogram exams are often ordered by practitioners for patients in A-Fib. If a thrombus was found within the heart’s upper chambers, would this be a critical result to be reported immediately? What treatment can you anticipate?
Risk Factors for A-Fib and Stroke
The following chart by the American Heart Association shows the risk factors for A-fib and stroke and shows which are modifiable versus which are not (3).
| Modifiable | Non-Modifiable |
| Hypertension | Age |
| Hypercholesterolemia | Race (2x higher risk for African Americans) |
| History Transient ischemic attack or TIA or Carotid Stenosis | Sex (women have higher risk) |
| Diabetes Mellitus | Ethnicity |
| Elevated homocysteine | History of migraine headaches |
| Heart Disease (A-fib, valve disease, prosthetic valve, mitral stenosis) | Sickle cell disease |
| Excess alcohol | Fibromuscular dysplasia |
| Use of tobacco products or illicit drugs | Heredity |
| Use of oral contraceptives | |
| Obesity | |
| Physical inactivity |
The clinical team must work with the patients and families to identify the specific risk factors for each patient to prevent future events. Patients with Atrial fibrillation as the cause of stroke will have an anticoagulation regimen prescribed. Traditional and “designer“ anticoagulants on the market can be confusing and difficult to differentiate benefits/risks.

Self Quiz
Ask yourself...
- Do any of these risk factors surprise you?
- Are patients always aware or forthright regarding their risk factors?
CHADs and Stroke Risk Scoring in A-Fib
Cardiologists and other clinicians use a scoring system to evaluate the stroke risk for those with non-valvular atrial fibrillation. The CHADS2 and the revised CHA2DS2-VASc scoring systems assist the practitioners and patients in making anticoagulation decisions. Patients with high scores (>2) are at significant risk for stroke with a 5.9% annual risk with a score of 3 and as high as 18.2% annual risk for those with a score of 6. The CHADS2 did not include some additional risk factors for stroke and was revised to the CHA2DS2-VASc, which now includes vascular disorders and expansion of age and gender risks. See tables below.
CHADS2 Score: Stroke Risk Assessment in Atrial Fibrillation: (4)
Score | CHADS2 Risk Criteria |
1 point | Congestive heart failure |
1 point | Hypertension |
1 point | Age ≥ 75 years |
1 point | Diabetes mellitus |
2 points | Stroke/transient ischemic attack |
CHADS2 Score and Corresponding Annual Stroke Risk: (4)
CHADS2 Score | Adjusted Stroke Risk (%) |
0 | 1.9 |
1 | 2.8 |
2 | 4 |
3 | 5.9 |
4 | 8.5 |
5 | 12.5 |
6 | 18.2 |
CHA2DS2-VASc Score and Risk Criteria: (4)
Score | CHA2DS2-VASc Risk Criteria |
1 point | Congestive heart failure |
1 point | Hypertension |
2 points | Age ≥75 years |
1 point | Diabetes mellitus |
2 points | Stroke/Transient Ischemic Attack/Thromboembolic event |
1 point | Vascular disease (prior MI, PAD, or aortic plaque) |
1 point | Age 65 to 74 years |
1 point | Sex category (i.e., female sex) |
The 2014 AHA/ACC/HRS guideline agrees with previous guidelines established by the European Society of Cardiology that oral anticoagulants be based on this objective scoring method. They advise anticoagulants for men with a CHA2DS2-VASc score of 1 or greater and women with a score of 2 or higher. We can see that this revised scoring is more inclusive of common risk factors that we have seen in the clinical arena.

Self Quiz
Ask yourself...
- Would explaining the risk for stroke CHADS2 scoring system to patients and families assist them in making decisions about anticoagulants?
- What are the common concerns that patients and families have regarding taking “blood thinners“?
Case Study
A 76-year-old male patient presents to ED with cellulitis and feeling palpitations at times with shortness of breath. He has a history of diabetes mellitus, peripheral arterial disease with right toe amputation, and a history of recent cessation of smoking. His blood pressure is 150/88 HR 130 Rhythm- “New Onset“ Atrial Fibrillation, RR 16 and Temperature of 100.5 F. He did not want to come to the hospital, his wife insisted since his cellulitis wounds started spreading and weeping. He seemed tired and ‘cranky“ lately, per his wife. He is treated with broad–spectrum IV antibiotics and moderate–rate fluid replacement. Cardiology was called to evaluate the A-Fib.

Self Quiz
Ask yourself...
- Using the CHA2DS2-VASc risk scoring system what would his score be?
- Would he qualify for oral anticoagulants?
- Would IV heparin infusion be considered in his case?
Oral Anticoagulants in A-Fib and Stroke Reduction
There are many oral anticoagulants available now, and each has its unique properties. If Coumadin (warfarin) is used, the INR goal is an average 2.5 (2-3); however, there are situations, especially in the over age 75 group, that a lower average goal of 2.0 INR is acceptable. Warfarin has an onset of 36-48 hours and can last in the system for 2-5 days, delaying any surgical procedures. Other oral anticoagulants for atrial fibrillation include Pradaxa (dabigatran), Xarelto (rivaroxban), Eliquis (apixaban), and Savaysa (edoxaban). Each has a unique half-life and reversal.
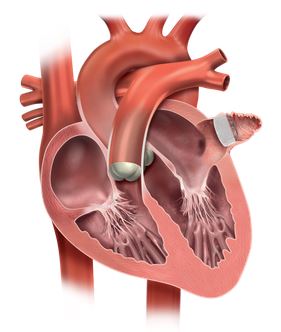
For those unable to take anticoagulants and who are at risk for atrial thrombus (which can form in the left atrial appendage due to reduced contractility during atrial fibrillation), a newer procedure has been developed called “Watchman.” In this procedure, a tent–like device is placed in the LA appendage to seal it off. “In nonvalvular atrial fibrillation, 90% of stroke–causing clots come from the left atrial appendage” (5). The outpouching of the sac is seen protruding from the left atrium in the diagram below (5).
Conclusion
Many patients with atrial fibrillation, whether chronic or acute, will have risk factors for stroke. The clinical team’s responsibility is to assess the risk of A-fib and stroke, then educate patients to assist in making decisions regarding stroke prevention. The risk of stroke from atrial fibrillation is a real concern as our population ages, and we have increasing amounts of patients diagnosed with A-fib and stroke. For patients presenting with ischemic stroke, the causal factors must be investigated to prevent stroke reoccurrence, which may include proper management of anticoagulants for atrial fibrillation.
References + Disclaimer
- American Stroke Association. (2021, February 11) “About Stroke“. https://www.stroke.org/en/about-stroke
- Babkair, Linda (2017) “Cardioembolic stroke: A Case Study“ Critical Care Nurse (37) 1, 170-174
- American Heart Association. (2021, February 11) “Stroke Risk factors“. https://www.stroke.org/en/about-stroke/stroke-risk-factors
- Tarek, Aham MD Medscape update (2021, February 17) “CHADS2 and CHA2DS2-VASc Score for Stroke Risk Assessment in Atrial Fibrillation“. https://emedicine.com/article/2172597-overview
- Watchman.com (2021, February 15) “Physician Resources: About the Procedure.“ https://www.watchman.com/content/watchman-com1/hcp
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate

